To describe clinical presentation, preoperative study, intervention, histology, surgical complications and follow-up characteristics, and survival in patients with thyroid carcinoma (TC) with less than 18 years at presentation.
Material and methodsretrospective analysis of clinical data of all children and adolescents followed in S. João Hospital from January 1, 2000 to March 31, 2010 with histologic diagnosis of TC.
ResultsTwenty-three patients were identified, 19 girls, and 4 boys. Median age at presentation was 17.0 years. Annual incidence was 2.3 cases/year. The main presenting symptom was a solitary thyroid nodule (60.8%). Three (13%) patients had risk factors for TC, 2 of the 3 had previous cervical irradiation. The other was a smoker. Total thyroidectomy was performed in 16 (69.6%), and 10 patients underwent a second surgical procedure. Four (17.4%) patients had postoperative complications. Histologic examination revealed differentiated TC in all, papillary thyroid carcinoma (PTC) in 86.9%, follicular carcinoma in the remaining. All patients received thyroxine suppressive therapy and 20 underwent therapeutic radioactive iodine (131I). During follow-up (7.1 years), 7 out of the 23 patients presented new metastases and needed new treatment. All patients are currently alive.
ConclusionsTC is a reality in pediatric population, thyroid routine examination should take part in all clinical examination in children and adolescents.
Describir la presentación clínica, el estudio preoperatorio, la intervención quirúrgica y complicaciones, así como la histología, el seguimiento y la supervivencia de pacientes con carcinoma tiroideo (CT) cuya edad es inferior a los 18 años en el momento de la presentación.
Material y métodosanálisis retrospectivo de los datos clínicos de todos los niños y adolescentes con diagnóstico histológico de CT seguidos en el Hospital São João, Oporto, desde el 1 de enero de 2000 hasta el 31 de marzo de 2010.
Resultadosse identificaron veintitrés pacientes, 19 niñas y 4 niños. La mediana de la edad de presentación fue de 17,0 años con una incidencia anual de 2,3 casos/año. El síntoma principal de presentación (60,8%) fue nódulo tiroideo solitario. Tres (13%) de los pacientes presentaban factores de riesgo para CT, 2 de los 3 habían recibido irradiación cervical. El otro era un fumador. Se realizó una tiroidectomía total en 16 pacientes (69,6%), 10 pacientes necesitaron una segunda intervención quirúrgica. Cuatro (17,4%) presentaron complicaciones postoperatorias. El examen histológico reveló CT diferenciado en todos los casos, con carcinoma papilar tiroideo en el 86,9% y carcinoma folicular en los restantes. Todos los pacientes recibieron tratamiento supresor con tiroxina y 20 recibieron tratamiento con yodo radiactivo terapéutico. Durante el seguimiento (7,1 años), 7 de los 23 pacientes presentaron nuevas metástasis y necesitaron un nuevo tratamiento. Todos los pacientes están vivos en la actualidad.
ConclusionesEl CT es una realidad entre la población pediátrica y los exámenes clínicos de niños y adolescentes debería incluir siempre una examen rutinario del tiroides.
Thyroid carcinoma is a rare disease in the first two decades of life,1 accounting for approximately 0.5–3% of malignant neoplasms in this age group.2 Nevertheless, 10% of all thyroid carcinomas occur before the age of 21 years.1,2 The incidence of this type of carcinoma in children and adolescents ranges from 0.2 to 5cases/million/year and is greater in patients with history of exposure to ionizing radiation.2 It is very rare before the age of 10 years and its incidence increases with age. There is a female predominance, with a female–male ratio 2.5–6:1.1
Patients typically present with a cervical mass but may also present with cervical lymphadenopathy, voice changes, or hyperthyroidism.3
When compared to adults, palpable thyroid nodules are less common in children and adolescents, with an incidence of 1.5%.4 However, the rate of malignancy among pediatric thyroid nodules is approximately 16%, about three times that of adults. In pediatric population there is also a much greater incidence of lymph node metastasis (40–80%) and distant metastasis (25%),5 but without an overall increase in mortality.1,6
High risk factors for thyroid carcinoma are younger age, male sex, large primary tumor size, extrathyroidal tumor extension, palpable lymph nodes, distant metastases at diagnosis, residual cervical disease after thyroidectomy, inadequate thyroid hormone suppression, diffuse sclerosing, or follicular thyroid histology.6
The authors present a retrospective review of all cases of thyroid carcinomas followed by pediatric endocrinology in S. João Hospital during the time period of the study.
Material and methodsCases were identified by searching the Department of Pathology database, for confirmed histologic diagnosis of thyroid carcinoma (TC) in patients less than 18 years at presentation. All tissues were obtained after surgical intervention (hemithyroidectomy, completion thyroidectomy [CT] or total thyroidectomy [TT]) at Hospital S. João, Porto, from January 1, 2000 to March 31, 2010.
A retrospective study was undertaken. A review of health records was conducted to determine patient demographics, risk factors, family history of thyroid disorders or malignancies, preoperative thyroid function, interventions (surgery and radioactive iodine [RAI]), and follow-up data. Data collection ended in May 30, 2011.
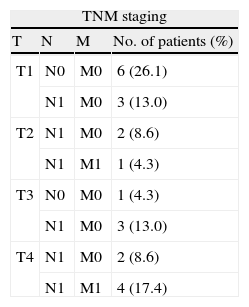
Tumor staging was performed based on the TNM (tumor-node-metastases) tumor classification system.7 All patients aged less than 45 years (all in this study) were classified as stage 1 (any T, any N, M0) or stage 2 (any T, any N, M1). Staging was assessed using data collected after thyroidectomy.
Statistical analysis was performed using SPSS 17.0; analysis of variance was used as appropriate depending on the continuous or discrete nature of the data. Multiple regression analysis was performed on selected clinically important variables. Significance was set at p<0.05.
The study was approved by the Hospital S. João pediatric endocrinology coordinator and an informed consent was signed by parents or children legal guardian.
ResultsTwenty-three eligible cases were identified, including 19 girls and four boys; median age at presentation was 17.0 years (range 10–18 years). Annual incidence was 2.3cases/year. The distribution of newly diagnosed patients was maximal in 2003 (6 cases), followed by the years 2000 and 2005 (4 cases each), no new case in 2007.
The main presenting motive was a solitary thyroid nodule with (7–30.4%) or without (7– 30.4%) associated systemic symptoms (namely anorexia, asthenia, dysphagia, cough, dyspnea, weight loss, polydipsia, and hyperthyroidism symptoms), followed by a palpable lateral cervical mass (3 – 13%) and accidentally detected mass in routine medical exam (3–13%); in one patient asthenia was the sole complaint. No data available about the clinical presentation in two of the patients. The symptoms started 10.8±13.2 (range 1–48) months before seeking medical attention (n=17). Three (13%) patients had risk factors for TC: 2 (8.7%) had received external therapeutic radiation for treatment of previous malignancies (Hodgkin lymphoma – last treatment 10.3 and 2.9 years before) and 1 was a smoker. One patient had preexisting thyroid disease (Grave's disease) and 2 were under prescription of thyroid medication: 1 L-thyroxin and 1 propylthiouracil. Six patients had family history of thyroid disease, although there is no family record of TC.
On the initial endocrine evaluation (n=21), 15 had normal thyroid function, 3 had thyrotoxicosis (raised thyroxin [T4] and decreased thyroxin stimulating hormone [TSH]) and 3 had hypothyroidism (decreased T4 and elevated TSH). Four (n=9) had positive antithyroid antibodies (antithyroglobulin and antiperoxidase antibodies) and 18 (n=23) had abnormal thyroid description in neck ultrasound. Hypoechogenic thyroid nodules described in 8 patients, nodules associated with cervical lymph node enlargement in five, calcificated nodules in two, and goiter in two. On physical exam 19 patients had abnormal thyroid palpation. Pubertal data were incomplete in medical records, and hence could not be evaluated.
Fine needle aspiration biopsy (FNAB) was performed in 17 patients and led to diagnosis of TC. In the reminder the diagnosis was established by histology after thyroidectomy.
Total thyroidectomy (TT) was performed in 16 (69.6%), with radical unilateral cervical lymph node dissection in 4 patients. Seven were treated with initial hemithyroidectomy. Ten patients underwent a second surgical procedure after review of the final pathology result of initial procedure or in the follow-up. The re-operated patients can be separated in two groups: group 1 – those who were submitted to TT after initial hemithyroidectomy or incomplete TT (n=7, mean 3.0±0.9 months after first procedure); group 2 – patients that were submitted to cervical node dissection (n=3, mean 96.0±55.7, range 3–108 months).
Four (17.4%) patients had postoperative complications, 2 persistent hypocalcemia and 2 transient hoarseness (one with associated transient hypocalcemia), which recovered spontaneously.
Histology revealed papillary thyroid carcinoma (PTC) in 20/23 patients (86.9%), 2 (8.7%) had diffuse sclerosing-PTC, and papillary TC-follicular variant in 7 (30.4%). In the remaining 3 patients follicular carcinoma was detected. Multiple tumor foci of papillary type were detected in 5 patients. Tumor size (n=18) ranged from 0.2 to 4.5cm (maximum diameter); 2 children had tumors measuring <1.0. Eighteen (78.3%) had stage 1 disease and 5 (21.7%) had stage 2 (4 patients had lung metastasis and 1 had thymic metastases). Four of the patients with stage 2 disease were males. TNM staging details of all patients are summarized in Table 1.
Twenty (87.0%) patients underwent therapeutic radioactive iodine (RAI), with a range of 1–6 doses. The first RAI treatment was done 5.0±5.1 months postoperative, 11 received first treatment within 3 months after surgery. Thyroid hormone therapy was applied in all patients.
The mean duration of follow-up was 84.9 months (range: 12–134 months). Seven patients presented new metastases in the cervical, mediastinal lymph nodes, lungs, and bones and need treatment during follow-up, 2 were re-operated and the others received additional RAI treatment. When patients completed 19 years they began to be followed by an adult endocrinologist. The patients were followed by clinical examination, thyroid and neck ultrasound, TSH, T4, and serum Tg levels every 6 months in order to detect recurrence or progression of the disease. Other exams (e.g. body cintigraphy) were performed when necessary.
All patients are alive and currently asymptomatic, but one patient had residual disease detected in FNAB in last follow-up (March 2011) and was referred to surgery.
Patients found to have TC in stage 2 was correlated with male sex (X2=17.4; p=0.001), and older age (X2=28.3; p=0.01). However, not related with histology, tumor size or need to re-intervention. Tumor diameter was not correlated with histology. Neither positive titer of thyroid peroxidase antibodies, nor TSH abnormal levels were associated with advanced disease (TNM classification).
DiscussionAlthough TC is known as an adult disease it is a reality in pediatric population. It is of the general knowledge that its occurrence and clinical course are different from those of the adult.1 Because most (up to 93%) of the thyroid malignancies in this age group tend to be well differentiated, and despite a tendency for children to present with advanced disease (including pulmonary metastases), survival outcomes are favorable (80–100% at age of 30 years).3
The annual number of children found to have TC at our institution did not increase during the time period of the study and the annual variation is not significant. Unfortunately, in our country there is no oncologic database in order to know the true incidence of TC in this age group, as well as its evolution over time. Other recognized study handicap is that our hospital is not the single hospital that attends and follows TC in our region, and so the true incidence of this disease remains unknown. Nevertheless, the current study is one of the first Portuguese studies addressing clinical data in the field of TC in children and adolescents. It is limited by the inherent bias of a retrospective review, and lacks some details, particularly in the oldest cases (without computerized clinical data).
The major conclusions are discussed below. The female to male ratio in our patients was 4.75–1, which is consistent with published data.1,8 Male were more likely to have disseminated disease at presentation (stage 2 in 100%), this is in keeping with previous studies that report that boys are more prone to develop subsequent metastases as well as have decreased disease-free survival.6 The initial clinical complaint was a thyroid nodule or cervical mass in the majority (73.9%) of our patients, and this is the most common presentation form of TC described (60–80%).2 There was a background of clinical thyroid disease in 1 patients and other 2 (8.7%) had developed TC has a secondary malignancy after treatment of a primary disease with cervical radiation. In fact, TC accounts for about 10% of second malignancies among cancer survivors, especially Hodgkin lymphoma, due to treatment not only with radiation but also with alkylating agents.9 So, this study supports the importance to render special attention in patients with known risk factors for TC. Some clinicians advocate that regular ultrasonography to screen for thyroid nodules, with precocious biopsies in suspicious nodules should take part of a regular follow up in cancer survivors.6 Cervical exam on first evaluation was abnormal in 82.6% of the cases, what reinforces the importance of thyroid palpation as part of physical exam in children and adolescents. There are a number of well-established predictors of malignancy in thyroid nodules that include hard and fixed lesions, rapid growth of nodules, large size, associated hoarseness, dysphagia, or lymphadenopathy.10 There are also suspicious ultrasonographic characteristics of thyroid nodules associated with higher risk: hypoechoic and solid, and in addition have microcalcifications, irregular borders, central blood flow on Doppler imaging, and a high anteroposterior to transverse ratio.10 Ten (43.5%) of our patients had high risk nodules description in the initial study. We only have information about the nodule diameter and no data about anteroposterior to transverse ratio.
Thyroid function was normal in 71.4% of the cases which is consistent with published data.2 We found no relation between abnormal TSH level or positive titer of thyroid antibodies with disease stage, but that could be due to the small number of patients of our series.
FNAB proved its diagnostic value, in all cases (n=17) with prior FNAB the diagnostic was established with this technique. All TCs were well differentiated and 86.9% of our patients had papillary carcinoma, similar distribution has been reported by other authors.1,2,6 Complications rate after surgery was low in the current study and must be so in general if patients are referred to specialized surgeons.1,6 The majority of authors recommend total or near-total thyroidectomy as the initial approach of TC1; in our series only one patient treated with initial hemithyroidectomy did not require re-intervention. Twenty of our 23 patients (87.0%) had received additional therapy with radioactive 131I; however, there were no complete data regarding the doses and so no conclusions can be determined with this information. No patient had radioiodine-related secondary malignancies over the follow-up period, which is short. The risk is small but does exist.1 All patients received suppressive doses of L-thyroxine and were closely monitored as defined by current guidelines.
Our survival rate was 100%, but at last follow-up one patient had residual disease. Considering the slow course of TC, this is a relatively short time of median follow-up (7.1 years). Continued monitoring is needed and the close contact between pediatric and adult a life-long period in order to recognize and treated promptly any local or distant metastasis. A temporal extension of the study will allow more reliable conclusions.
In summary, even those children and adolescents with advanced TC have an overall good prognosis. A national oncologic database is needed with the intention of improving our understanding of this pathology, prompt diagnosis and optimizing treatment of pediatric TC.
Conflict of interestThe authors have no conflict of interest to declare.