Tuberculosis is an endemic disease in developing countries with an increasing incidence. Intestinal tuberculosis is a rare presentation in the absence of pulmonary disease and has a wide spectrum of clinical manifestations, mimicking other diseases such as Crohn's disease or neoplastic diseases; therefore the diagnosis is a challenge for physicians. A case is presented of a 34-year-old patient with vague abdominal symptoms with previous diagnosis of adenocarcinoma of the colon, who attended our medical unit for a second opinion.
La tuberculosis es una enfermedad endémica en algunos países en desarrollo con una incidencia que va en aumento. La tuberculosis intestinal es una presentación rara en ausencia de enfermedad pulmonar, y tiene un amplio espectro de manifestaciones clínicas que pueden simular otras enfermedades como enfermedad de Crohn o enfermedades neoplásicas, es por ello que representa siempre un reto diagnóstico. Describimos un caso de un paciente de 34 años con síntomas vagos con diagnóstico previo de adenocarcinoma del colon que acudió a nuestro hospital por una segunda opinión.
Tuberculosis is an endemic disease in Mexico and in developing countries. Although it is a common infectious disease with a rising incidence, intestinal tuberculosis (ITB) is not a common presentation with a wide spectrum of clinical manifestations, simulating other diseases such as Crohn's disease or a wide range of malignant diseases.1 Because of the wide variety of non-specific manifestations (diarrhea, constipation, nausea, abdominal pain, abdominal mass) the correct diagnosis remains being a challenge. Molecular, histologic and endoscopic studies allow a better diagnostic approach in patients with high suspicion of ITB.2 Histologic diagnosis with Ziehl–Nielsen stain shows acid-fast bacilli and granuloma, however less than 30% of biopsies show bacilli. On the other hand, real-time PCR assay in colonic tissue only has a sensitivity of 40–75%. Culture of biopsy is the gold standard however it requires 3–8 weeks to provide conclusive results.3 Therefore an integral approach is important to make a correct diagnosis and initiate the proper therapy as soon as possible.
Case presentationA 34-year-old male was admitted to the Internal Medicine Department of Medica Sur Clinic and Foundation with a 2-month-history of unintentional weight loss of 17kg, increase in bowel movements with loose and unformed stools, and abdominal pain in right lower quadrant. The diarrhea was associated with abdominal discomfort and it occurred up to 5 times a day. He referred non-quantified fever with afternoon predominance, and diaphoresis. He had history of an episode of pancreatitis of unknown etiology 3 years prior to this hospitalization, allergy to ceftriaxone, and a right orchiectomy for non-specified reason. He came from a rural town in Puebla state in Mexico and had a story of ingestion of non-pasteurized dairy products including milk and cheese. He denied prior contact with patients with tuberculosis and has no pets. He has family history of type 2 diabetes mellitus and one late uncle with history of non-specified cancer.
Previously he had been admitted to another Institution for diagnostic approach, where lab tests were carried out only with alterations in liver function tests with a cholestatic pattern, alkaline phosphatase (AP) 146U/L, and gamma glutamyl transpeptidase (GGT) 163U/L, the rest of lab tests were normal. In the same hospitalization, a thoracoabdominal CT scan was performed with finding of a tumor in right colon and cecum, with report of possible malignant characteristics, abdominal and retroperitoneal nodes and a distant lesion in lung with report of probable metastasis, the diagnosis of adenocarcinoma of the colon was given. He attended to our institution for a second opinion.
On examination, blood pressure was 119/62mmHg, the pulse 74 beats per minute, and temperature 36.4°C. Plain chest X-rays were normal. Abdomen was painful at medium compression, and a solid, undefined, immobile, painful mass of 5–6cm of diameter was palpable in right lower quadrant, with no signs of acute abdomen. In the Emergency Department new lab tests were performed with the next results hemoglobin 10.4g/dL, platelets 541×103/ml, leukocytes 6.6×103/ml, glucose 87.5mg/dL, creatinine 0.87mg/dL, total proteins 6.47g/dL, albumin 2.66g/dL, direct bilirubin 0.11mg/dL, alanine aminotransferase 20U/L, aspartate aminotransferase 21U/L, AP 125U/L, GGT 106U/L, lactic dehydrogenase 163U/L.
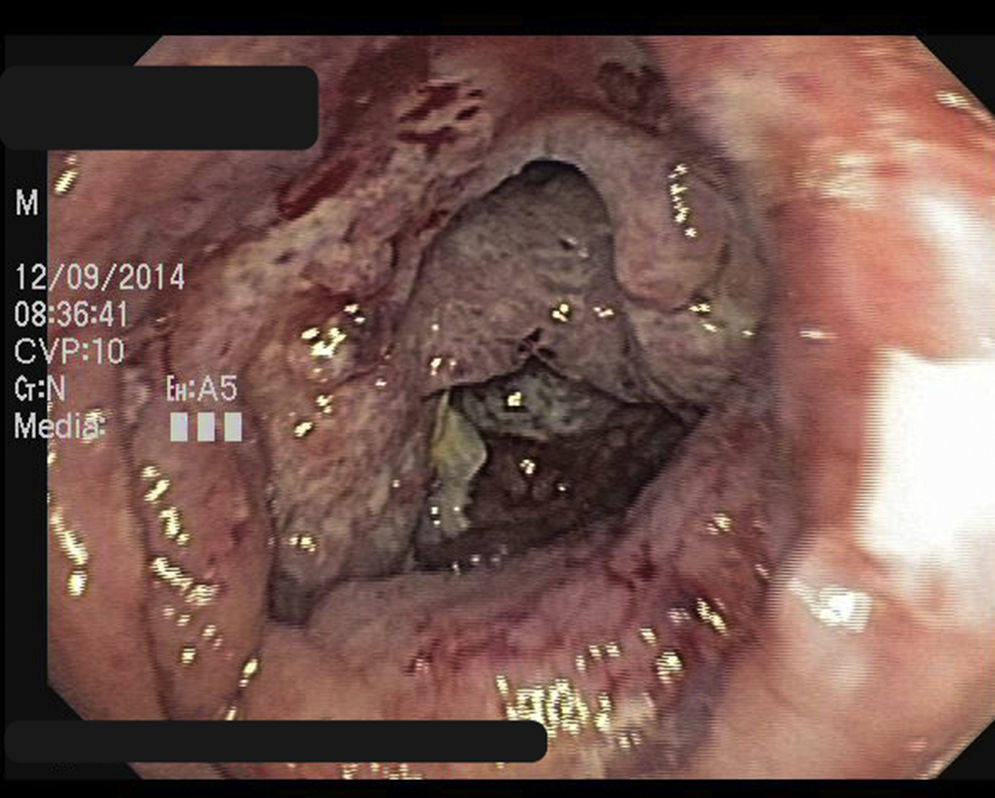
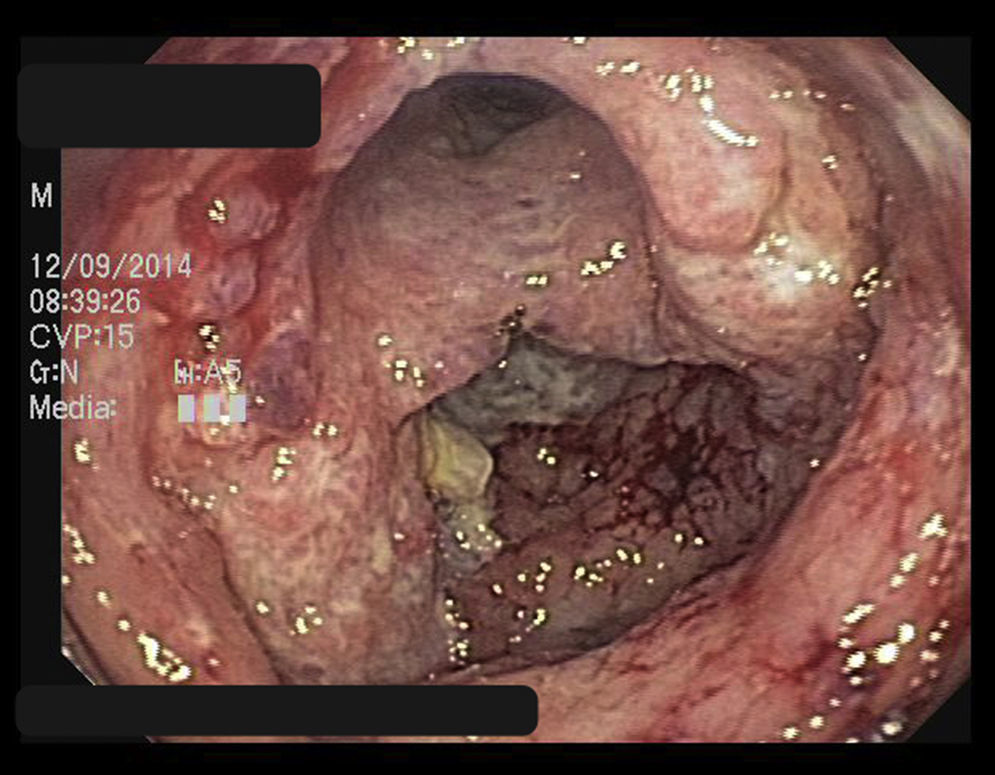
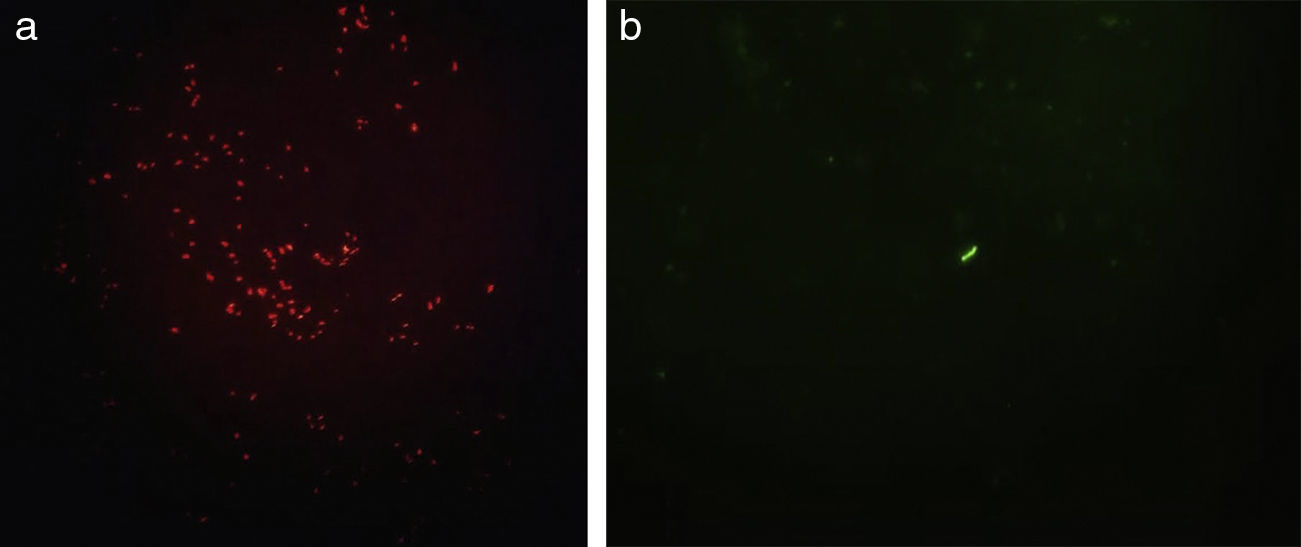
A new CT scan was performed with finding of thickened colonic wall in ascending colon, with mediastinal, retroperitoneal adenopathies, bilateral pulmonary nodules and splenomegaly. Therefore a colonoscopy was done. A stenotic, nodular-shaped and ulcerated zone of 25cm approximately was found, with loss of normal morphology, between terminal ileon and cecum (Figs. 1 and 2), biopsies were taken. Auramine-Rhodamine stain of the biopsies showed abundant fluorescent acid-fast bacilli (Fig. 3). Real-time PCR assay of the biopsies was positive for isoniazid and rifampin-sensitive Mycobacterium tuberculosis. Shortened, directly observed therapy strategy (DOTS) for tuberculosis with ioniazid 300mg, rifampin 600mg, pirazinamid 1600mg and ethambutol 1200mg was initiated.
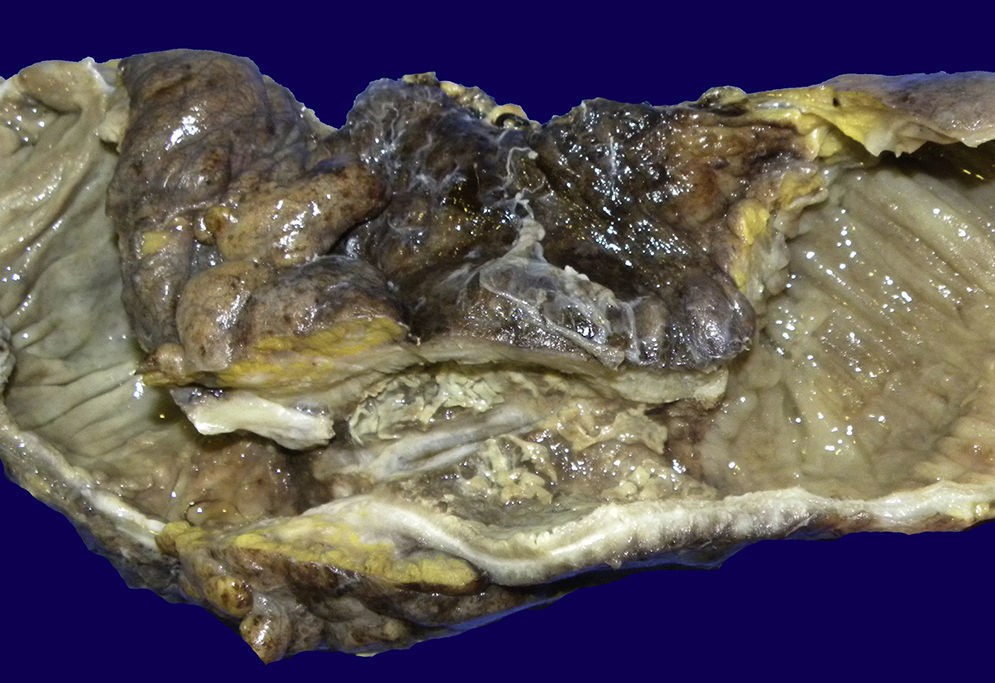
One month after the treatment was initiated, he was re-admitted to the Emergency Department because of intense abdominal pain, cramps, arthralgia and myalgia. The patient had, previous to his admission, an episode of non-bloody diarrhea and vomit of gastric contents. Plain abdominal X-rays showed bowel distention and multiple gas-fluid levels, therefore a CT scan was carried out and bowel occlusion was confirmed. Open exploratory laparotomy was performed with finding of multiple peritoneal implants and an ileocecal tuberculoma; therefore open right hemicolectomy with ileo-transverse anastomosis was completed (Fig. 4). He remained hospitalized for 5 days for post-surgical surveillance with appropriate evolution and was discharged, to continue DOTS.
DiscussionITB is a rare extrapulmonar variety of tuberculosis, with an increasing incidence in the last decades, specially in endemic countries such as Mexico. The diagnosis of ITB is always a challenge, and it is difficult to make the correct differential diagnosis specially with Crohn's disease and with different neoplasic diseases. The diagnostic approach, has implications in correct management and therefore in survival of patients, while ITB is a curable disease, Crohn's disease is a progressive relapsing illness, and intestine neoplasms, such as linfoma or adenocarcinoma may have an endoscopic appearence of circumferential thickening, with ulcers and fistulae formation that mimicks Crohn's disease or ITB.4 Although tuberculosis is a much more common disease in Mexico than Crohn's disease, incidence of inflammatory bowel disease in Mexico seems to be rising,5 probably, because it has become a more known disease and physicians suspect it more frequently, for this reason is imperative for Mexican doctors to recognize and learn to make the differential diagnosis of these diseases, particularly because ITB is a curable disease with the appropriate treatment initiated early. In this aspect, a diversity of endoscopic, histologic and biochemical criteria has been considered to diagnose correctly ITB.3 Considering endoscopy, Sato et al., classify endoscopic findings in four types: type 1 showing linear ulcers with circunferential arrangement with a nodullary mucosa; type 2 showing irregular, rounded ulcers without nodules; type 3 multiple erotions limited to colon; and type 4 aphtous ulcers limited to the ileum. In this case, the patient showed type 1 findings.2 After the hemicolectomy was carried out, the macroscopic view of the surgical piece, showed stenosis of the lumen and ulcerations, with a totally modified morphology. The macroscopic view of the tuberculoma could have mimicked adenocarcinoma. In a prospective study by Chalya et al., 49.6% (127 patients) of 256 patients with abdominal tuberculosis presented with intestinal obstruction, and 82.8% of the sample underwent surgical treatment, and only 6.6% presented with an ileo-cecal mass. 6 Almost 75% of patients with intestinal obstruction present with data of malabsorption, in this case the patient only presented one episode of diarrhea at the time of the occlusion, without any other data of malabsorption.7
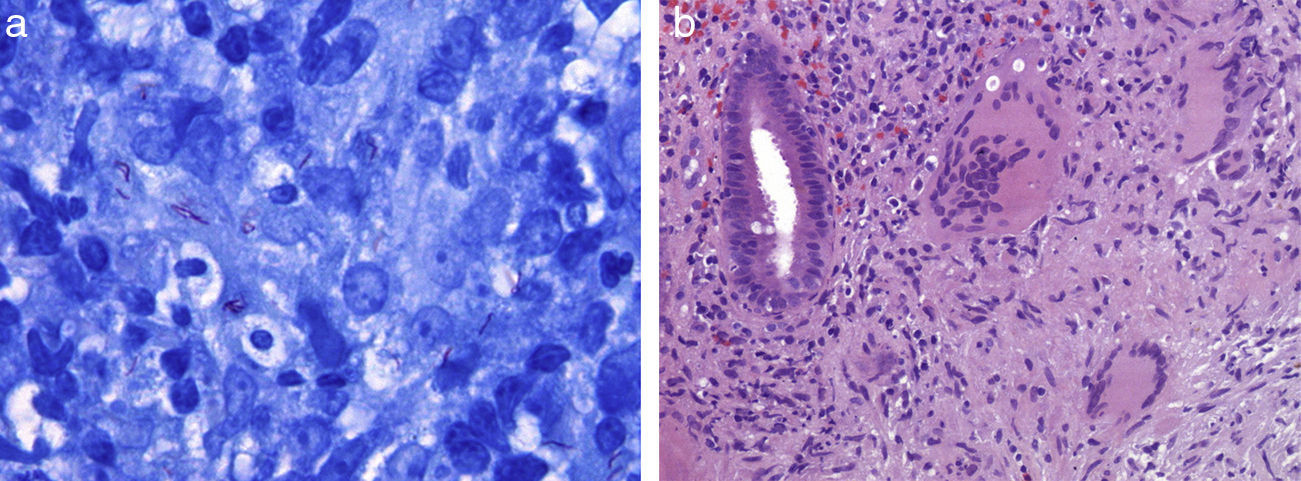
Regarding histological diagnosis, the typical findings in tuberculosis are the large granulomas, usually larger than 200m, multiple and confluent. And a distinctive characteristic of the granulomas in tuberculosis is the central caseiation, 8 although the most trustworthy finding in the biopsies, is the evidence of M. tuberculosis.3 In this case we could observe several acid-fast bacilli present in the preparations of biopsy specimens. It is worth to mention that when the histological tests of the surgical piece of the hemicolectomy where performed, although numerous acid fast bacilli were found in Ziehl–Nielsen stain (Fig. 5a and b), the typical image of caseating necrosis and granulomas was absent, however hyalinized lymph nodes could be observed.
On the other hand, nucleic acid amplification by PCR of M. tuberculosis in biopsy samples can facilitate diagnosis due to higher sensitivity and specificity than culture, and results can be obtained in 48h instead of 6–8 weeks. This lab test can also identify potential drug resistance, such as to rifampicin or to isoniazid.
The ITB is a disease that may mimic many other diseases; therefore a correct approach is necessary for the correct diagnosis and treatment. In this case where previous tests showed a probable malignant disease, thanks to the modern technology such as PCR in the biopsy tissue the patient initiated treatment for tuberculosis a few days after the colonoscopy was performed.
FundingThe authors did not receive sponsorship to undertake this article.
Conflict of interestThe authors declare no conflict of interest.