Intraductal papillary mucinous neoplasm (IPMN) of the pancreas is a papillary proliferation of ductal epithelium and represents a spectrum of disease ranging from benign to malignant lesions. IPMN is an increasingly recognized cause of acute and recurrent pancreatitis. The prevalence of this neoplasm in the setting of recurrent acute pancreatitis is variable. Males are affected with IPMN more often than females (ratio 1.4:1). The age at presentation is most commonly in the sixth decade of life.
La neoplasia mucinosa papilar intraductal (NMPI) del páncreas es una proliferación papilar del epitelio ductal, representa un espectro de enfermedades que van desde lesiones benignas a malignas. La NMPI es una causa cada vez más reconocida de pancreatitis aguda y recurrente. La prevalencia de esta neoplasia en el escenario de pancreatitis aguda recurrente es variable. Los varones se ven afectados más frecuentemente que las mu-jeres (relación 1.4:1). La edad de presentación es más común en la sexta década de la vida.
Introduction
Intraductal papillary mucinous neoplasm (IPMN) is an intraductal mucin-producing epithelial neoplasm that arises from the main pancreatic duct (MDIPMN), secondary branch ducts (BD-IPMN), or both (mixed type, Mix-IPMN). After being first reported by Ohashi and colleagues in 1982, IPMN is increasingly reported worldwide and accounts for about 5% of pancreatic neoplasms resected at referral centers.1 Most patients diagnosed with IPMN are asymptomatic. When associated with symptoms, IPMN can present with abdominal pain, weight loss, jaundice, steatorrhea, diabetes, and pancreatitis.2 The purpose of this case report is to raise the awareness of IPMN as a potential cause of acute and acute recurrent pancreatitis even in a young patient.
Case report
We present a 21-years-old man patient, who presented with recurrent acute pancreatitis. Personal medical history was not significant. The patient presented to our hospital with complaints of acute onset of severe epigastric pain, nausea and vomit. The patient had presented two previous episodes of acute pancreatitis in the last year, with no apparent cause. On admission he had a lipase of 1 682 UI/l. Transabdominal ultra-sound, liver function tests, blood count, calcium and triglycerides were normal.
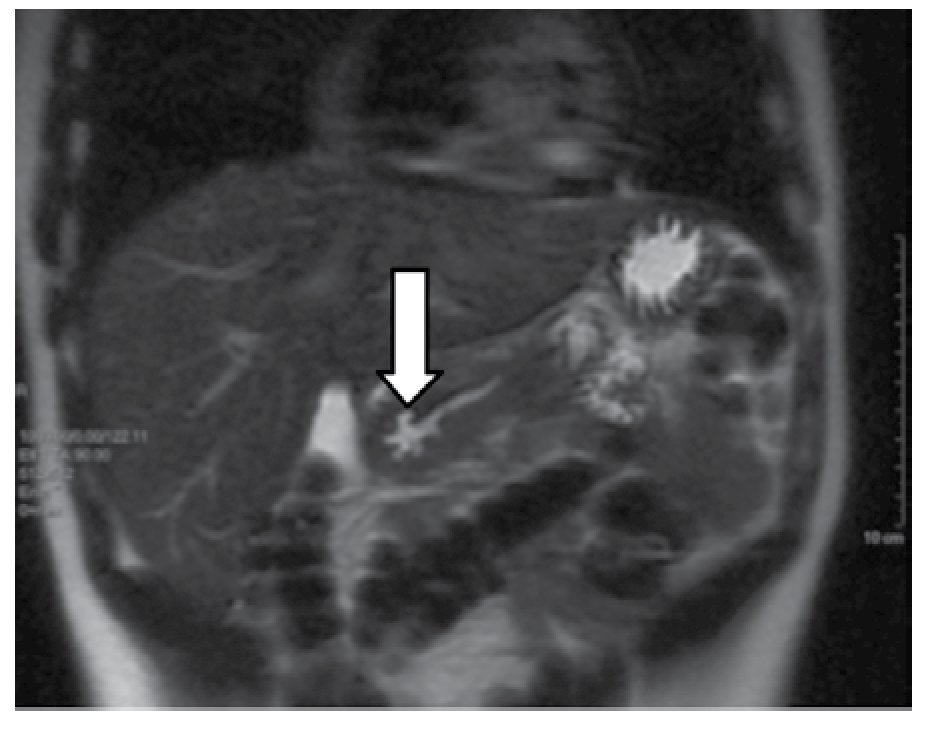
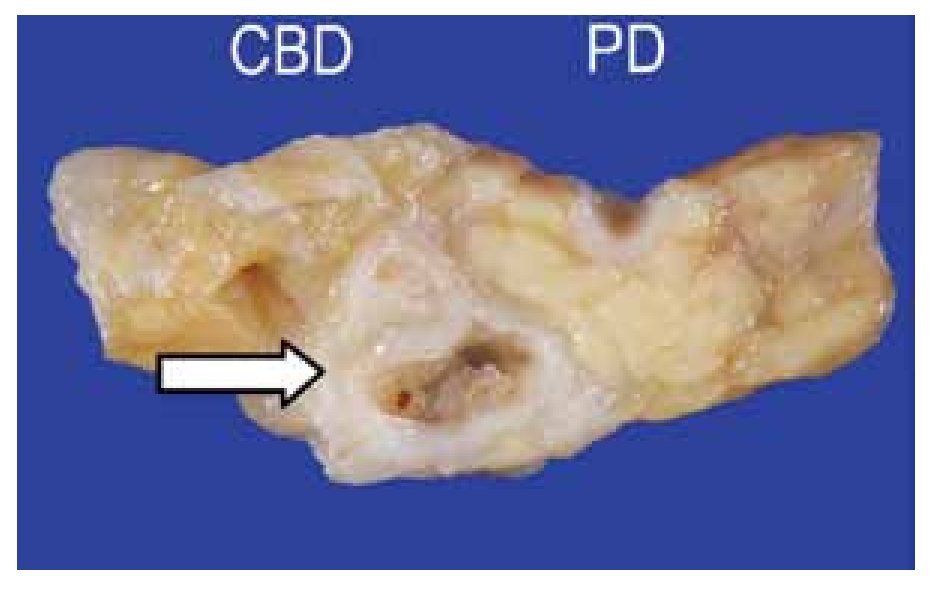
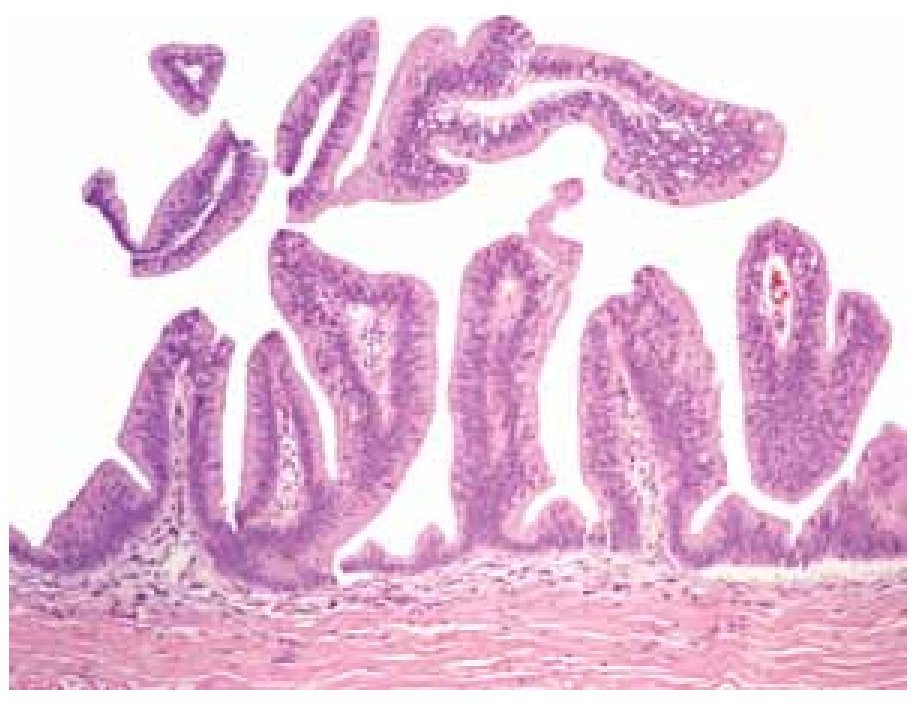
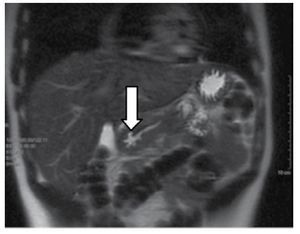
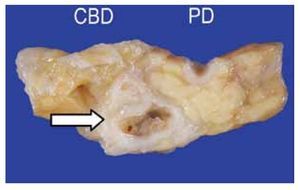
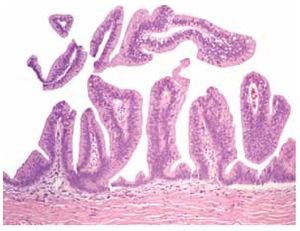
Magnetic resonance cholangiopancreatography (MRCP) showed a stellar image in the pancreatic neck with a normal main pancreatic duct (Figure 1). The endoscopic ultrasound (EUS) showed a small multicystic area of 10 x 9 mm in size with septa connected through a side branch with the main pancreatic duct without solid component or lymphadenopathy; the diagnosis of side branch IPMN was suggested (Figure 2). Patient underwent to pancreatoduodenectomy and the pathology reported a sidebranch duct IPMN, with pancreatic intraepithelial neoplasia type 2 (PanIN-2) (Figures 3 and 4). Since the surgery, patient has recovered well and is asymptomatic after eighteen months of follow-up.
○ Figure 1. Magnetic resonance cholangiopancreatography that shows a stellar image (white arrow) in the neck of the pancreas with normal main pancreatic duct.
○ Figure 2. Linear EUS that shows a small multicystic lesion with septa in the neck of the pancreas (white arrow) connected through a side branch with the main pancreatic duct.
○ Figure 3. Cross section of Whipple surgery product showing the head of the pancreas. A dilated secondary branch 8 mm in size showed papillary projections into the lumen (white arrow). In the upper portion, the normal common bile duct (CBD) and the pancreatic duct (PD) are shown.
○ Figure 4. High magnification hematoxylin and eosin (H&E) stain of the neoplasm of intestinal type which was composed of papillary structures lined by pseudostratified mucin-producing columnar epithelium with mild dysplastic changes (H&E stain, 200 X).
Discussion
Intraductal papillary mucinous neoplasm (IPMN) of the pancreas is a papillary proliferation of ductal epithelium and represents a spectrum of disease ranging from benign to malignant lesions. The IPMNs affect males more often than females (ratio 1.4:1), and the age of presentation is commonly in the sixth decade of life.1 IPMN may be categorized into three forms on the basis of the areas of involvement: main pancreatic duct (MD-IPMN), side branch (SB-IPMN), or combined.1,3 Both MD-IPMN and SB-IPMN may be the cause of pancreatitis.4
Our patient was 21 years old when the diagnosis was made, and presented with recurrent attacks of acute pancreatitis. Tumors, both benign and malignant, are related to recurrent pancreatitis in 9% of patients,5 pancreatic ductal adenocarcinoma has been most commonly associated with pancreatitis.6 However, cystic pancreatic tumors including IPMN are anincreasingly recognized cause of acute and recurrent pancreatitis. The rate of AP in IPMN patients is highly variable with rates in published surgical series from 12% to 67%.3 AP, mural nodules higher than 6 mm, dilated main pancreatic duct (> 6 mm) and BD-IPMN measuring > 3 cm are often indicative of the necessity of surgery according to the guidelines.1,7
Although branch duct IPMN has a lower prevalence of malignancy than main or mixed IPMN,8 our patient was symptomatic, with recurrent attacks of acute pancreatitis, so we considered his best treatment was pancreatoduodenectomy.
Overall 5-year survival rate for resected noninvasive IPMN is 77% to 100%. Recurrence rates after resection of noninvasive IPMN (adenoma, borderline, and carcinoma in situ) are about 8% and generally occur in the pancreatic remnant.1 Pancreatoduodenectomy has 30-40% morbidity and 5% mortality.9 The purpose of this case report is to raise the awareness of IPMN as a potential cause of acute and acute recurrent pancreatitis even in a young patient. Pancreatic intraepithelial neoplasia (PanIN) is an epithelial neoplasm of the pancreatic duct that can be seen in conjunction with IPMN. PanIN-3 is a significant risk factor for ductal adenocarcinoma, PanIN-1 and PanIN-2 demonstrate less nuclear atypia and they are not associated with ductal adenocarcinoma, and do not require further resection.1 Endoscopic ultrasound (EUS) appears to be diagnostic in the majority of patients with previously unexplained pancreatitis, and offers an alternative to endoscopic retrograde cholangiopancreatography and magnetic resonance cholangiopancreatography.10
Correspondence:
David García Rangel, MD.
Gastroenterology Department. Instituto Nacional de Ciencias Médicas y Nutrición "Salvador Zubirán".
Vasco de Quiroga 15, Col.
Sección XVI, Tlalpan.
Mexico City, Mexico.
E-mail: davgaran@hotmail.com