La colangiopancreatografía por resonancia magnética (MRCP) es una técnica de imagen que se usa frecuentemente para evaluar los conductos biliares y pancreáticos. Las indicaciones clínicas son muy similares a las de colangiopancratografía retrógrada endoscópica (CPRE) e incluyen: litiasis biliar, neoplasias del tracto pancreatobiliar, anomalías congénitas, variantes anatómicas y enfermedades inflamatorias. Los nuevos escáneres de 3T permiten obtener una mejor resolución de imagen y mayor relación señal ruido, resultando en una mejor calidad de imagen. MRCP dinámica con estimulación con secretina es útil para evaluar anomalías del conducto pancreático y de la unión pancreatobiliar. Los medios de contraste que se eliminan predominantemente por vía biliar, son una alternativa para evaluar la anatomía de la vía biliar y fístulas biliares posterior a cirugía.
Magnetic Resonance Cholangiopancreatography (MRCP) is a non-invasive imaging technique used frequently to evaluate the biliary and pancreatic ducts. The clinical indications are similar to those for endoscopic retrograde cholangiopancreatography (ERCP) including: calculous disease, neoplasms, congenital anomalies, anatomical variants and inflammatory processes. With the use of new 3 Tesla scanners, the image resolution and signal to noise ratio have improve significantly resulting in better image quality. MRCP after secretin stimulation is a valuable dynamic technique to evaluate complex pancreatic ductal anomalies and anomalous pancreaticobiliary junction. Contrast agents that are specifically excreted into the bile allows an important alternative to evaluate biliary anatomy and are mainly used detect leaks after biliary surgery.
Introduction
Since the early 1990's magnetic resonance cholangiopancreatography (MRCP) has evolved from a questionable imaging technique for evaluation of the biliary tract and pancreatic duct to a extremely powerful tool to evaluate and diagnose pancreatobiliary disease.1
Part of the acceptance of MRCP is the improving technique that allows a similar appearance of the biliary tree and pancreatic duct using a non-invasive approach compared to endoscopic retrograde cholangiopancretography (ERCP). For many years, ERCP has been considered the standard of reference for imaging the biliary tract and pancreatic duct, however, it is an invasive examination associated with complications that occur in to 5% of all attempts and that range from subclinical to life threatening, like pancreatitis, hemorrhage, cholangitis and gastrointestinal tract perforation.1-3
The clinical indications to perform MRCP are very similar to those for ERCP including: biliary stones, biliary and pancreatic neoplasms, congenital anomalies and anatomical variants, sclerosing cholangitis and sphincter of Oddi dysfunction. An advantage of MRCP over ERCP is the evaluation of the biliary tree in postoperative situations wherein access with and endoscope to the major papilla is limited.4,5
With recent technology innovations like the advent of new 3.0 Tesla scanners it is possible to obtain images with increased in signal to noise ratio (SNR) resulting in better quality imaging with less imaging time.
With the new contrast agents that are specifically excreted into the bile allows an important alternative to evaluate biliary anatomy and are mainly used detect leaks after biliary surgery or for anatomic mapping before living donor liver transplantation.6,7
Technical considerations
There are two main distinct approaches to visualize the biliary tree with MRCP. Both methods relies on the visualization of fluid filled structures which appears bright on T2 weighted sequences do to its physical properties. Taking advantage of the property, two approaches are used to acquire images: thick slab (single shot fast spin echo) and multi-section thin slab (single or multi-shot fast spin echo) techniques.4
Thick slab techniques uses 20-150 mm thickness oblique coronal slabs in different angles parallel to the biliary tree. Every image is acquired in a few seconds. The result consists of multiple images covering projections in 180° within one minute. Fluid filled structures like the stomach, small intestine, colon, collecting urinary system, medullary canal, cystic lesions might overlap the tree. The overlapping effect of the upper GI tract can be diminished using a commercially available iron containing negative contrast. A cheaper alternative is pineapple juice. Thick slab is ideal to obtain a general overview of the biliary tree. Visualization of small lesions or ductal stones can be limited so it is important to always correlate with the thin slab or axial images.
Thin slab consists in the acquisition of individual multiple thin section (2 to 5 mm thickness) until a predetermined 3D volume of patient anatomy is completed. Each of these thin sections can be acquired in a single breath hold or during shallow breathing. The advantage of this technique is a higher spatial resolution. Shorter echo times decrease the amount of artifacts. The acquisition of 3D data offers several options for post-processing. Small filling defects or tumors are better evaluated using this technique compared to thick slab images.4,7-9
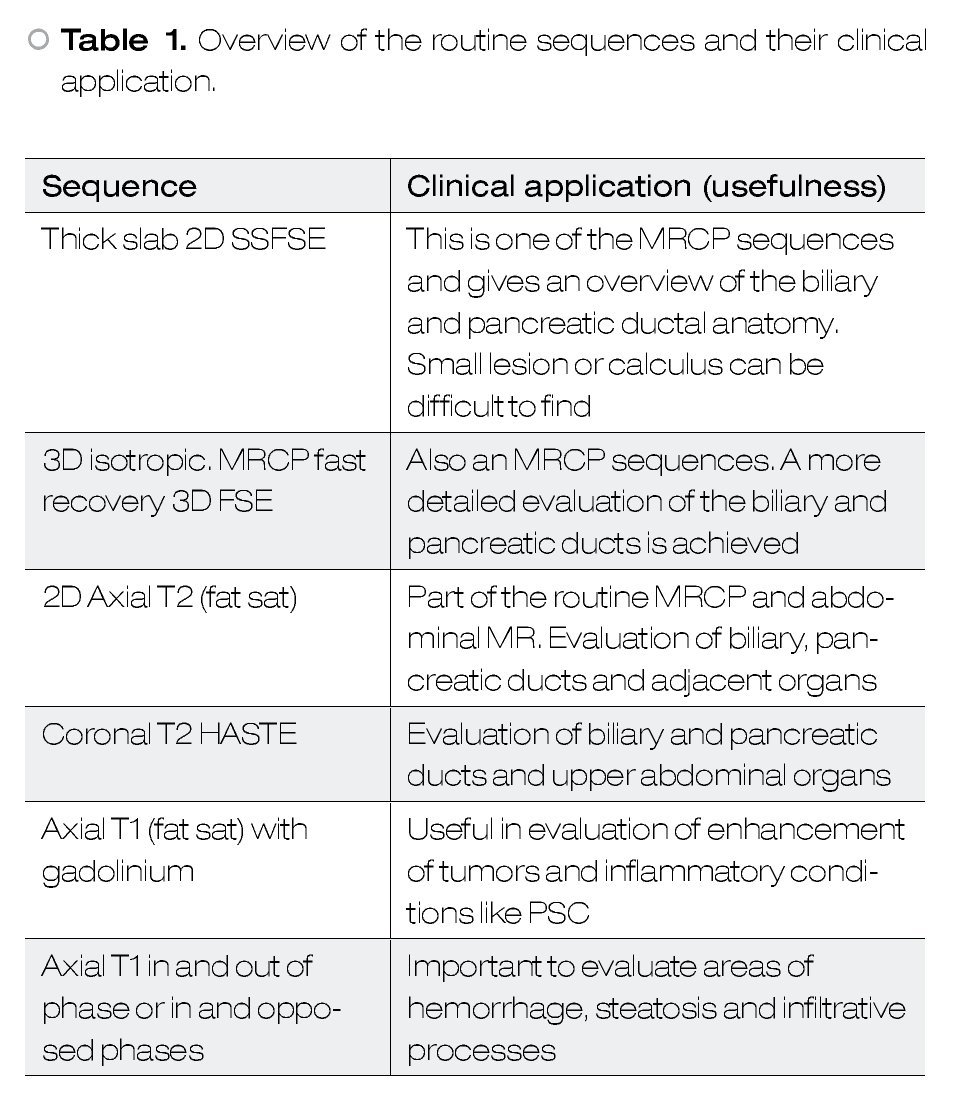
In addition to the MRCP sequences it is always recommendable to acquire other sequences to have an overview of the upper abdomen and to characterize other abnormalities. Many recommend the use of heavily T2-weigthed sequences, non fat-suppressed sequences (half-Fourier acquisition single-shot turbo spin-echo HASTE) allowing visualization of solid organs as well has the pancretobiliary tract. The use of T1, dynamic and post-contrast T1 with fat saturation sequences can provide important information when evaluating neoplasms or disorders like primary sclerosing cholangitis. Gradient echo in and out of phase sequences are useful in evaluating parenchymal anomalies (e.g. steatosis) and hemorrhage/blood clots.2,3Table 1 shows an overview of the routine sequences and their clinical application.
Several methods of image post-processing can be used for MRCP images the most useful are 3D volume rendering and maximum intensity projection (MIP). In a simplistic explanation of these techniques, 3D volume rendering consists of a computer algorithm used to transform serially acquired images in 3D images.
In MIP the highest intensity voxels in a determined volume are incorporated in a 2D or 3D image.
These methods are widely used in CT or MR-angiography but are also helpful in MRCP to have an anatomical overview before or after surgery or have a better understanding of tumor extension.10
Clinical applications
Anatomical variants
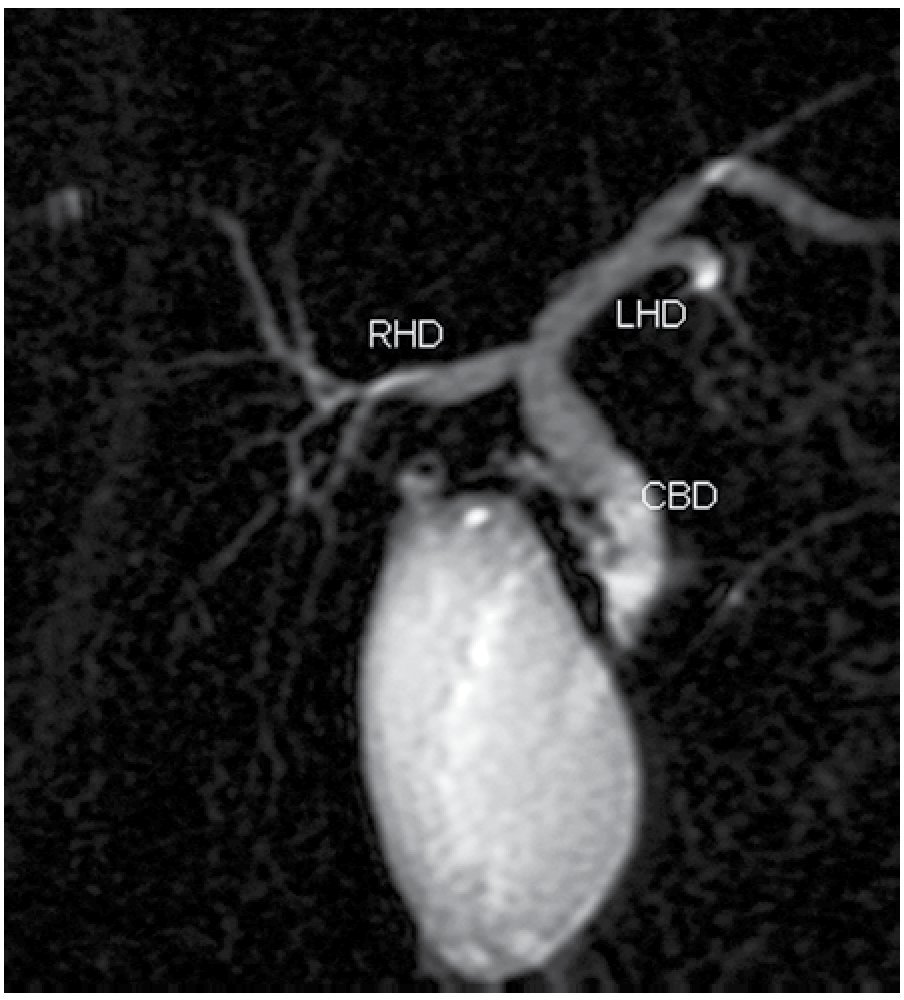
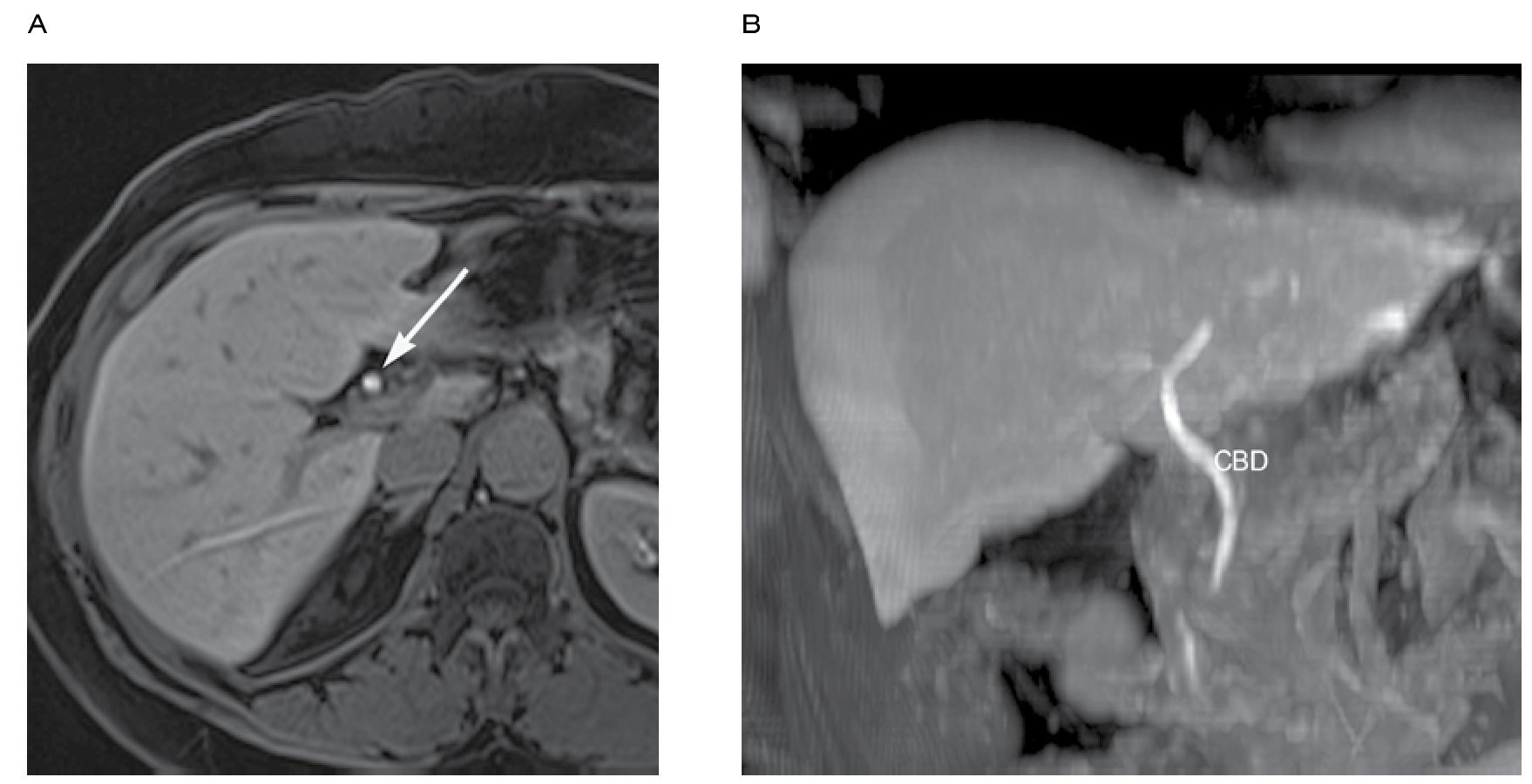
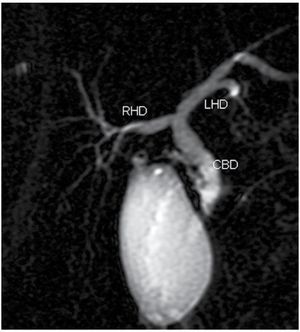
The classically described anatomic configuration of the bile duct, consisting of two right segmental hepatic ducts (anterior and posterior) joining to form the right hepatic duct and two major segmental branches on the left lobe (medial and lateral) is present in 50%-60% of the population (Figure 1).11
| Figure 1. Normal MRCP, thick slab image showing the anatomic configuration of the bile ducts, consisting of two right segmental hepatic ducts joining to form the right hepatic duct (RHD) and two major segmental branches on the left lobe (LHD). The RHD and LHD join together in the common hepatic duct and then the cystic duct join to form the common bile duct (CBD).
Anatomic variants of the biliary tract are frequent in up to 37% of individuals. The crossover anomaly is characterized by the dorsocaudal branch of the right hepatic duct entering the central left hepatic duct occurring in 13%-19% of the population (Figure 2). Trifurcation of the biliary ducts is also common occurring in 19%.5,11
|Figure 2. Thick slab image showing a crossover variant consisting in the right posteriorhepatic duct draining into the left hepatic duct.
These variants become very important in patients undergoing biliary surgery particularly hepatic living donor transplant.
Choledocal cysts
Bile duct cyst or choledocal cysts are rare cystic dilatations of the biliary tree. There are five types according to the Todani classification:
1. Type I is the most common (80%-90%) and is defined as a fusiform dilatation of the common bile duct (CBD)
2. Type II is a true saccular diverticulum from the extrahepatic bile duct.
3. Type III or choledocele, represents a protusion of a dilated segment of the distal CBD into the duodenum.
4. Type IV is subdivided in two subtypes IVa, which consists of fusiform dilatation of the CBD with intrahepatic extension and IVb, consisting of multiple saccular cystic dilatations of only the extrahepatic bile ducts.
5. Type V or Caroli disease is rare disease that manifests cystic dilatations of only the intrahepatic bile ducts. Also associated with renal cystic disease and renal tubular ectasia (Figure 3).
| Figure 3. Oblique coronal MIP (maximum intensity projection) obtained from a 3D isotropic thin slab sequence, showing multiple cystic dilatations of the intrahepatic bile ducts.
Choledocal cysts are surgically corrected because of the risk of cystolithiasis, recurrent cholangitis, pancreatitis and malignant transformation to cholangiocarcinoma. MRCP is an excellent method to delineate the biliary cysts and the extent.5,12
Pancreas divisum
Pancreas divisum is the most common congenital anomaly of the pancreatic ductal system being reported in 4%-10% of the population. This anomaly results when the ventral and dorsal pancreatic ducts fail to fuse. It is usually asymptomatic but is more frequently seen in patients with recurrent pancreatitis than in the general population.
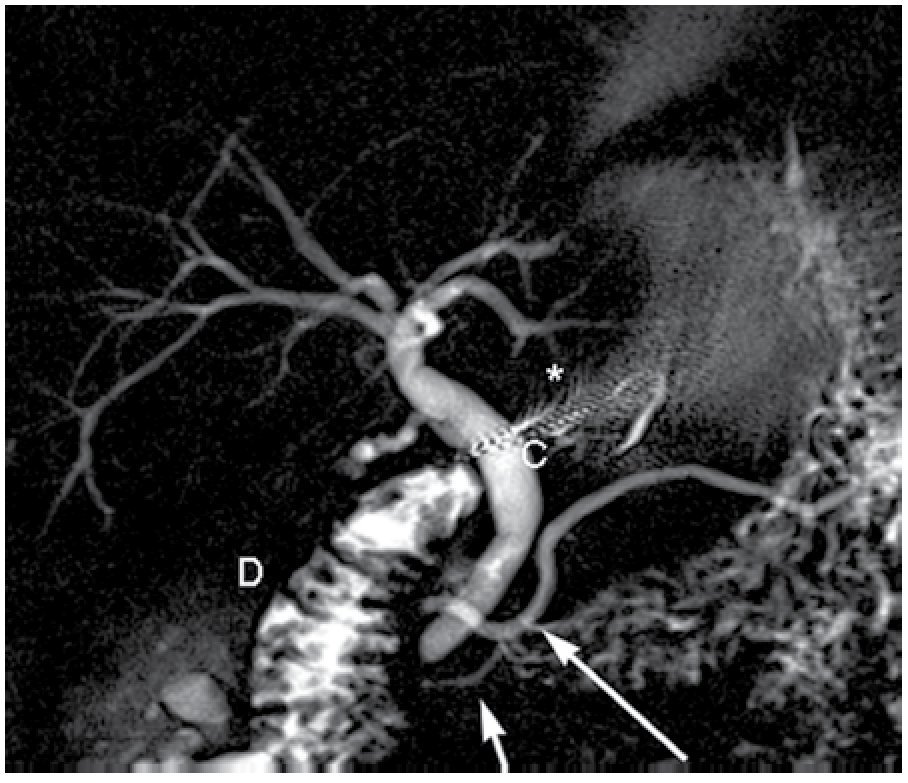
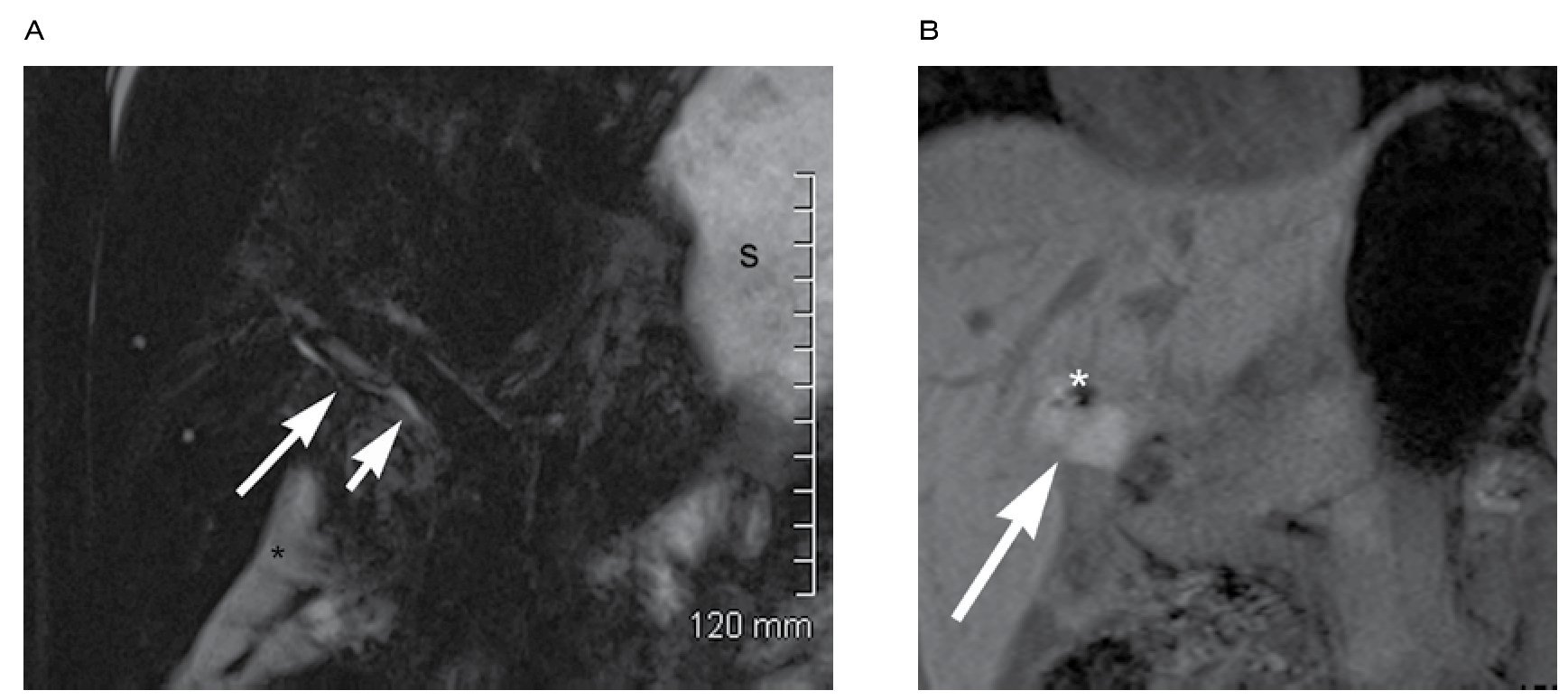
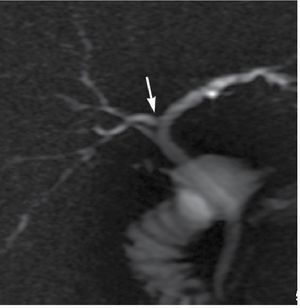
MRCP is very sensitive and specific showing noncomunicating dorsal and ventral ducts, independent drainage sites and a dominant dorsal pancreatic duct (Figure 4).13-15
| Figure 4. Oblique coronal thick slab image in a patient with pancreas divisum. Note the dorsal pancreatic duct (large white arrow) and the ventral pancreatic duct (short arrow) without any communication. A small focus of metallic susceptibility artifact from prior cholecystectomy is noted (*), common bile duct (C), duodenum (D).
Annular pancreas
Annular pancreas is rare congenital pancreatic ductal anomaly in which rotation of the ventral anlage leads to a segment of pancreas encircling the second part of the duodenum. The prevalence is one in 2 000 and occurs either as an isolated finding or other congenital anomalies. In one of the symptomatic patients it manifests in the neonate with gastrointestinal obstruction of biliary duct obstruction. In adults in may manifest with "peptic ulcer disease", duodenal obstruction or pancreatitis.
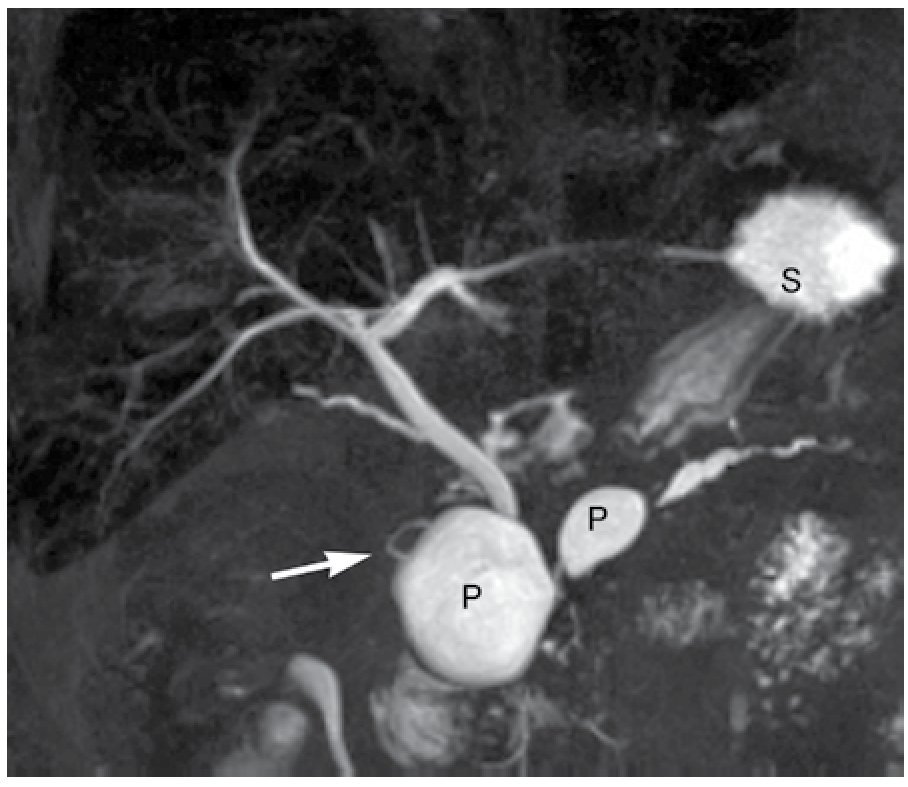
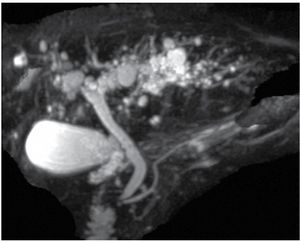
Two types of annular pancreas have been described: intramural and extramural types. In the intramural type the pancreatic tissue is intermingled with muscular fibers of the duodenal wall with small ducts draining into the duodenum whereas in the extra-mural type the ventral duct encircles de duodenum to join the main pancreatic duct (Figure 5).15
| Figure 5.Extramural type annular pancreas in a patient with recurrent pancreatitis and two pseudocysts (P), including one within the pancreatic parenchyma encircling the duodenum and common bile duct. Note the ventral pancreatic duct (short arrow) right to the common bile duct and pseudocyst and the dorsal pancreatic duct (large arrow).
Gallbladder disease
Non-malignant disease of the gallbladder is usually evaluated with ultrasound (US). The normal appearance of the gallbladder on T2 weighted sequences is a low signal intensity wall with high signal intensity bile. The signal intensity of the bile depends on the water, cholesterol and biliary salts concentrations. In the fasting state, water can be reabsorbed leading to a more concentrated content of cholesterol and bile salts appearing with a T1 and T2 hyper-intense.5
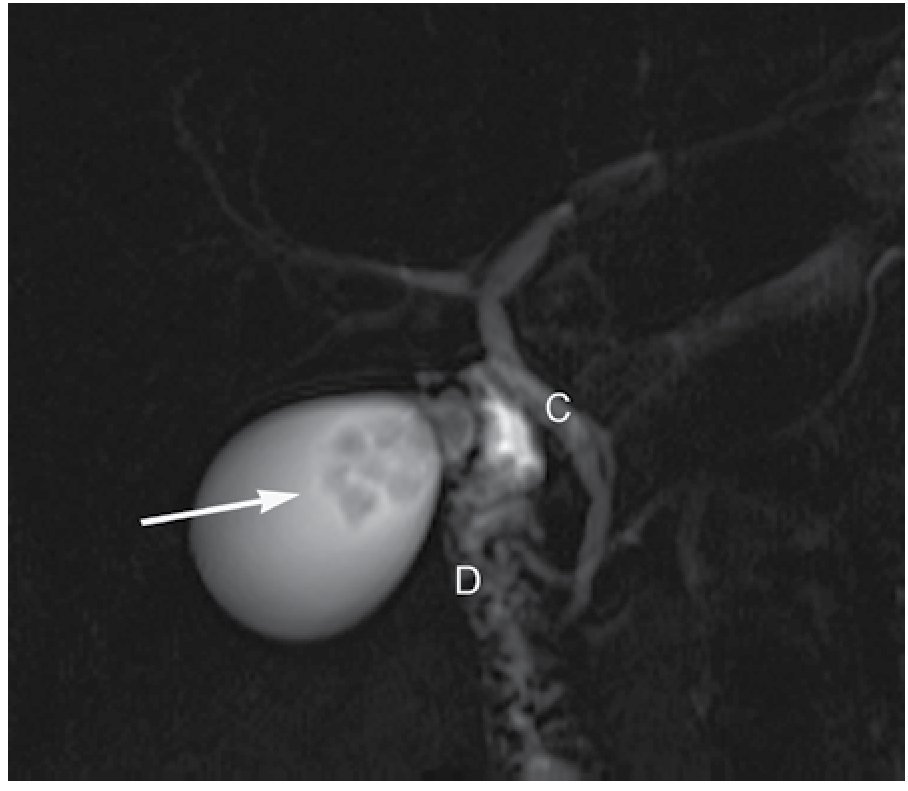
Gallstones are easily identified as signal voids in a T2 hyper-intense background. Pitfalls in the recognition of gallstones include: air bubbles, hemorrhage and debris. Some clues to differentiate gallstones from pitfalls are location, appearance on T1 and in and out of phase sequences. Air bubbles are located in the non-dependent portion usually creating air-fluid level. Blood clots and hemorrhage appear hyper-intense on T1 sequences (Figure 6).
|Figure 6. Multiple flow voids within the gallbladder consistent with gallstones (arrow), common bile duct (C), duodenum (D).
Cholecystitis is usually diagnosed with US, however in certain equivocal situations, MR imaging can be useful identifying cystic and gallbladder neck calculi. A hyper-intense thick and edematous wall with pericholecystic fluid is seen on T2 sequences.4,5
Choledocolithiasis
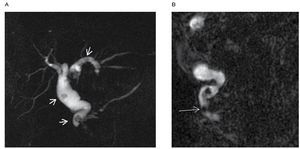
Intraductal stones are depicted as biconcave signal voids within the ducts. Even with thin slices stones smaller than 3 mm can be missed. It is always useful to evaluate stones using thick (Figure 7A) and thin MRCP images as well as in the axial sequences (Figure 7B).
| Figure 7. A) Thick slab oblique coronal showing multiple calculi within the common bile duct and intrahepatic ducts (arrows), note that distal to the most distal calculus common bile duct remains dilated. B) Thin slab oblique coronal. In addition to the the multiple biliary calculi seen on the thick slab image (Figure 7A) a small calculus is seen just cephalad to the ampulla.
The overall prevalence of common bile duct (CBD) stones in patients with cholelithiasis is between 8%-15%. In the acute setting endoscopic stone extraction followed by papillotomy with subsequent cholecystectomy remains a preferred approach. In more stable patients, open or laparoscopic cholecystectomy with CBD exploration can also be an alternative.
MRCP is being used frequently to image patients for treatment planning before surgery to predict if biliary exploration will be needed during surgery or ERCP before surgical intervention.4,5,16
Primary sclerosing cholangitis (PSC)
PSC is associated with inflammatory bowel disease in 75% of patients. Diffuse fibrosing inflammation of the small, medium and large intra and extra-hepatic biliary ducts is found in PSC. ERCP remains the gold standard for PSC, however it is invasive and is associated with complications that are often seen with a higher rate. MRCP has been shown to be equivalent to ERCP in the diagnosis of PSC. ERCP is usually reserved for therapeutic interventions.5,17
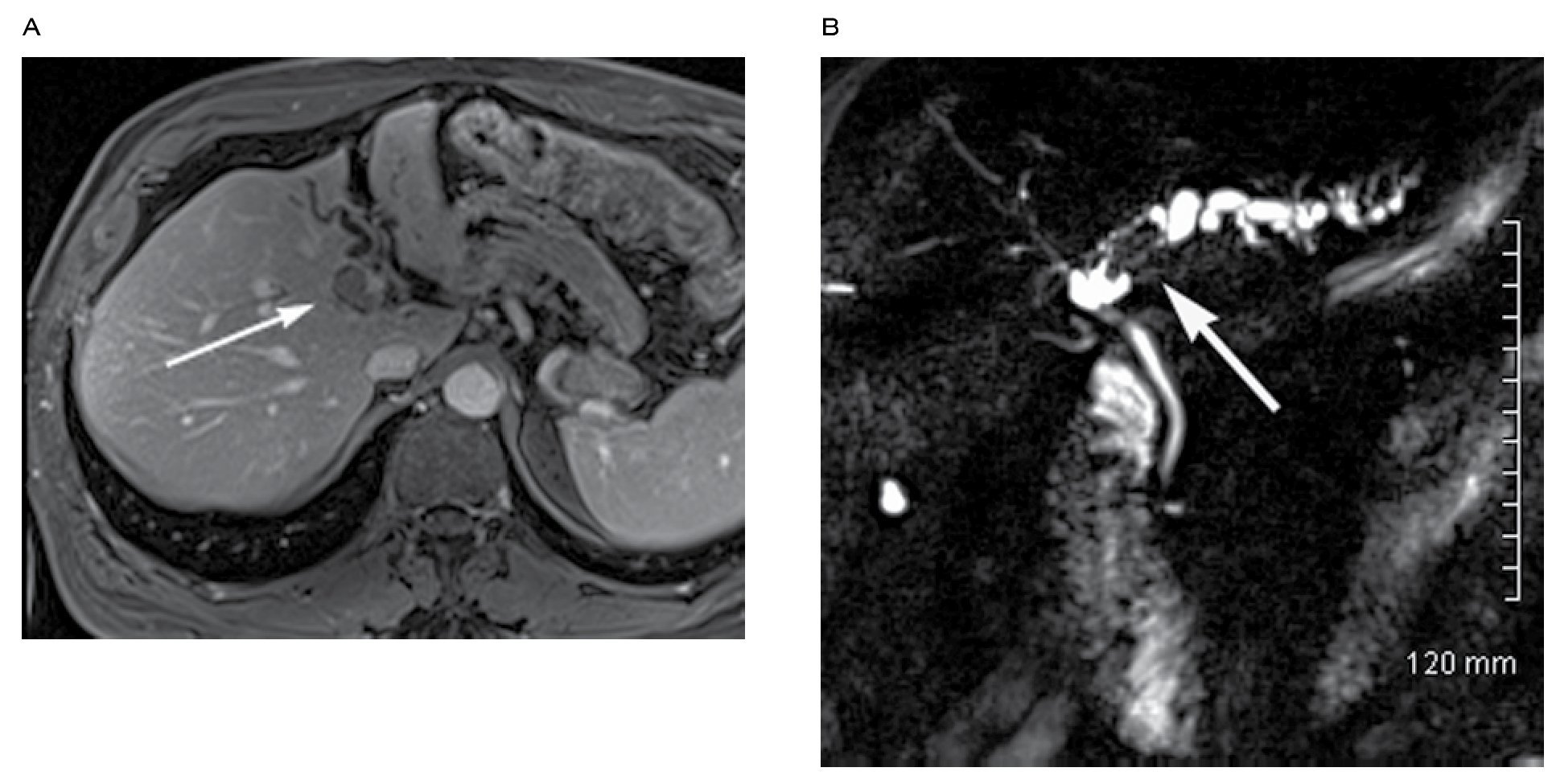
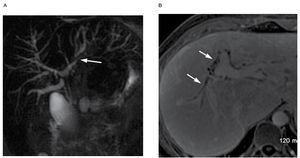
The classic MR findings include multifocal dilation of biliary segments alternating with segments of stricture, peripheral wedge shaped areas of T2 signal of the liver parenchyma, ductal calculi, and the visualization of biliary ducts extending to the edge of the liver parenchyma, which are not normally seen. The use of intravenous contrast is very helpful not only for the diagnosis but also to evaluate disease progression and monitoring the treatment (Figure 8).
| Figure 8. A) Multiple low grade stenoses of the intrahepatic bile ducts with a more severe stenosis on the left intrahepatic duct (arrow). There is also diffuse beaded appearance. B) Axial T1 fat sat with gadolinium in a different patient than Figure 8A showing contrast.enhancement of dilated bile ducts in a patient with PSC. Note also the beaded appareance of the ducts.
An advantage of MRCP over ERCP as that it can also evaluate the liver parenchyma.
Twenty percent of patients with PSC die of cholangiocarcinoma. MR with contrast is helpful assessing the size, location and extension of the tumor.5,18,19
Benign and malignant strictures
Benign strictures are seen as smooth-walled tubular narrowing of the bile ducts, sometimes associated with mild displacement of the duct due to adjacent fibrosis.
The degree of stenosis is best depicted on thin-slab images. Thick slab and maximum intensity projection (MIP) tend to overestimate the degree of stenosis.
Abrupt stenoses with prestenotic dilatation often have a malignant cause. Intraductal and mass forming cholangiocarcinoma can be evaluated with MR imaging. The site of obstruction and relation relative to the common hepatic ducts and bifurcation can be evaluated with MRCP. Intraductal lesions from cholangiocarcinoma can also be assessed on MRCP sequences. Other non-MRCP sequences can be important for a comprehensive evaluation. Subtle cases can present only with increased signal surrounding a mildly dilated biliary tree which may be even more difficult to diagnose but most be suspected in a patient with PSC.4,5
Cholangiocarcinoma
Hilar cholangiocarcinoma is the most common manifestation of cholangiocarcinoma and is depicted as a high-grade stricture of the confluence of the right and left hepatic ducts. MRCP has become an important tool in the evaluation the location and extension of the disease. In hilar cholangiocarcinoma MRCP demonstrates marked narrowing of the proximal extrahepatic bile duct, extension to the right and left hepatic ducts and dilatation proximal to the obstruction.20,21
Relative to the liver parenchyma, mass forming cholangiocarcinoma can be hypo to isointense and variable hyperintense on T2 weighted sequences. On T1 post-contrast images minimal or incomplete enhancement is seen in the periphery on early images whereas progressive enhancement is seen in delayed phases. These pattern of enhancement is explained by neoplastic cells located in the periphery of the lesion with central areas of fibrosis and desmoplastic response (Figure 9).22
| Figure 9. A) Axial T1 fat sat with gadolinium showing an intraductal cholangiocarcinoma at the level of the intrahepatic ducts confluence extending to the LHD. Note that there is mild enhancement of the lesion. B) Thick slab oblique coronal, same patient as Figure 9A. Showing the intraductal cholangiocarcinoma (arrow) of the intrahepatic ductal confluence extending to the LHD.
Cholangiocarcinoma involving the extra-hepatic duct distal to the confluence are often referred to as the distal duct type and are often seen as strictures or intraductal polypoid masses resulting in biliary obstruction on both MRCP and ERCP.23
Pancreatic carcinoma
MRCP can not only identify the ductal dilatation that occurs as the result of pancreatic carcinoma but also depicts the malignant ductal strictures themselves and localizes the neoplastic process to the pancreas.
The characteristic imaging findings are stenosis or obstruction of either the common bile duct or the pancreatic duct or both resulting in the "double sign duct". While the double dict sign in often seen in association with pancreatic head carcinoma, it is nonspecific and can occur in benign and malignant processes involving the pancreatic head. If the carcinoma involves the body or tail the dilatation of the pancreatic duct is limited to the portion of the duct proximal to the obstruction.
MR angiography in conjunction w ith MRCP allows for evaluation of resectability. T1 and T2 fat sat sequences are useful in depicting small tumors. Usually pancreatic adenocarcinoma is hypointense relative to the pancreatic parenchyma
Conventional MR is also helpful to evaluate for liver metastasis and nodal involvement.24-26
Intraductal papillary mucinous neoplasm of the pancreas
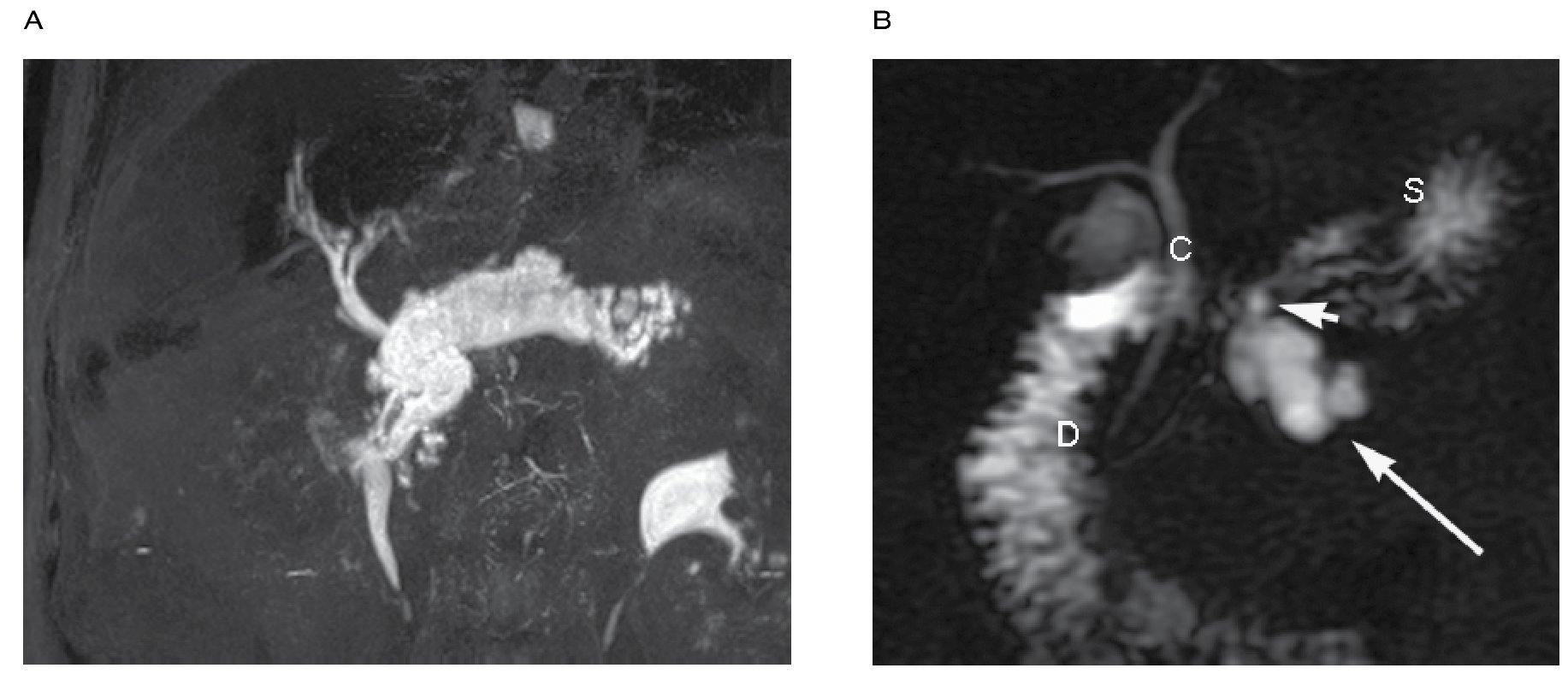
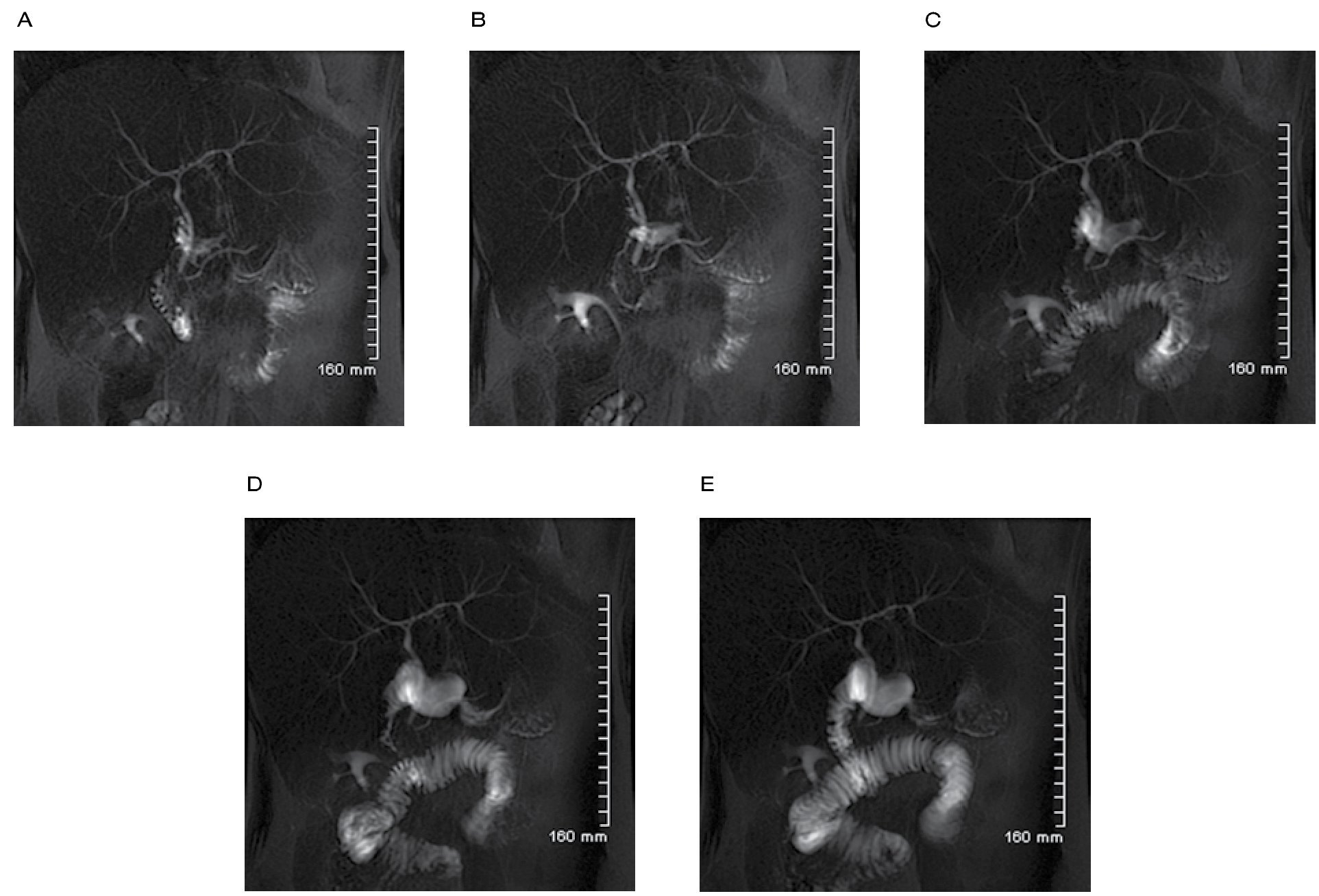
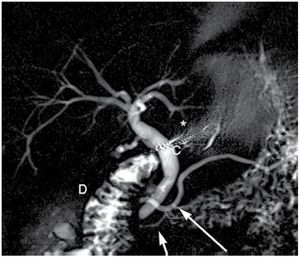
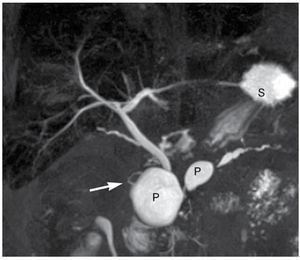
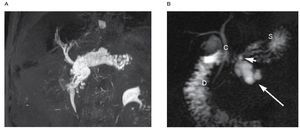
Intraductal papil lary mucinous neoplasms (IPMNs) are categorized as main duct type and branch duct type depending on the duct of origin. IPMNs are well evaluated with MR and MRCP because the mucin content which is depicted as hyperintense signal on T2 weighted sequences. The whole spectrum of IPMNs can be evaluated with MRCP consisting of: main duct dilatation, cyst dilatation of side branches, nodules, septa and intraductal filling defects. It is also to see the communication between the lesion and the pancreatic ducts (Figure 10). Intraductal filling defects and diffuse dilatation of the main pancreatic duct greater than 15 mm in main duct tumors are strongly associated to malignancy.25,27,28
|Figure 10. A) Thick slab oblique coronal showing a main duct intraductal papillary mucinous neoplasm. B) Thick slab oblique coronal in a patient with side branch intraductal papillary mucinous neoplasm (large arrow), a small communication with main pancreatic duct is noted (small arrow). The stomach (S) is partially overlaying the pancreas. Common bile duct (C). Duodenum (D).
Contrast enhanced MR cholangiography
MR cholangiography can also be performed with contrast agents that are specifically excreted into the bile. These contrast agents include gadobenate dimeglumina (Gd-BOPTA®) (Multihance, Bracco Diagnostics), gadoxetic acid disodium (gadoxetate disodium, or Gd-EOB-DTPA) (Eovists or Primovist®; Bayer Healthcare, Leverkusen, Germany) and mangafodipir trisodium (Mn-DPDP®) (Teslascan; Nycomed, Zurich, Switzerland) (not availabe in US). When this contrast media are used T1 fat-saturated sequences are obtained. These agents shorten the T1 relaxation time of bile, resulting in high signal intensity bile at T1 sequences (Figure 11).
|Figure 11. A) Axial T1 fat sat after the administration of Eovist (Gd-EOB-DTPA; Bayer Healthcare, Leverkusen, Germany). Bright signal is noted in the common bile duct (arrow) due to the biliary excretion of the contrast media. B) Coronal MIP reformat obtain from the same patient as Figure 11A, showing bright signal along the intra and extrahepatic biliary ducts.
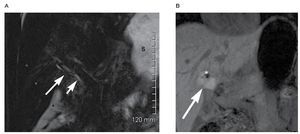
These agents are used frequently in contrast enhanced liver MR to characterize lesions and also as direct cholangiography in conjunction with MRCP studies for bile duct anatomic mapping before surgery or to evaluate biliary leaks after surgery (Figure 12).7,29
|Figure 12. A) Thin slab 3D oblique coronal MRCP in a post-cholecystectomy patient presenting with worsening abdominal pain. Note the anatomical variant consistent with a low insertion of the posterior right hepatic duct (large arrow) in the common bile duct (short arrow). Perihepatic biloma (*), stomach (S). B) Coronal T1 fat sat obtained 2 hours after the intravenous administra
tion of Eovist (Gd-EOB-DTPA; Bayer Healthcare, Leverkusen, Germany), showing contrast media within the perihepatic biloma.MRCP with secretin stimulation
Secretin is a polypeptide hormone secreted by duodenal m in response to increased luminal acidity. It induces pancreatic secretion of water and bicarbonate. In the first 3-5 minutes after the administration, the tone of sphincter of Oddi is increased. These effects result in the temporary distention of the pancreatic ducts. Synthetic human secretin (ChiRhoS-tim®, ChiRhoClin, INC, Burtonsville, Maryland) is intravenously injected over one minute to avoid potential abdominal pain.
An adult dose of 16 ug (0.2 ug/Kg body weight) is used.
Before the injection a baseline coronal oblique SSFSE image (same sequences as thick-slab MRCP) is obtained. After the injection sequential images are obtained every 30 seconds over a period of 10 minutes. Each image takes only two seconds to be acquired.
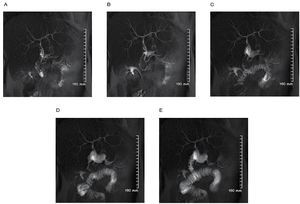
Secretin is valuable in the evaluation of complex pancreatic ductal anomalies, such as annular pancreas and anomalous pancreaticobiliary junction (Figure 13).26,30
|Figure 13. A) to E). MRCP with secretin stimulation at one, three, five, seven, nine minutes after the secretin administration, showing normal pancreatic and common bile duct caliber without abnormal dilatation after secretin stimulation. Note the progressive filling of the duodenum with pancreatic and gastric juices.
Conclusion
MRCP is a valuable non-invasive imaging modality that can provide important information. It will never replace the therapeutic capabilities of ERCP however, it has been extremely useful to evaluate the biliary tree, liver, pancreas and adjacent organs. In many cases it can the only diagnostic study needed to provide and appropriate diagnosis. With the use of newer 3T scanners the image quality is much better compared to less powerful scanners.
Conflict of interest
The author declare no conflict of interest.
Funding
No financial support was provided.
Correspondence:
Radiology Department, Froedtert Memorial Lutheran Hospital, Medical College of Wiscosin.
9200 W. Wisconsin Ave Milwaukee WI. Z.P. 53226.
E-mail: antonsosaloz@yahoo.com.mx