Introducción: Se han realizado numerosos estudios, que describen los diferentes factores de riesgo de complicaciones post-CPRE. Se realizó un estudio prospectivo para determinar la frecuencia y factores de riesgo, asociados a complicaciones post-CPRE.
Material y métodos: Se evaluaron los siguientes datos: la indicación y la duración del procedimiento, el número de intentos de canulación, el uso de precorte o esfinterotomía, la canulación del conducto pancreático y la pancreatografía, datos demográficos del paciente, incluyendo edad, sexo, estatura, peso e índice de masa corporal. Las complicaciones fueron evaluadas durante y después del procedimiento. La mortalidad a los 30 días se evaluó mediante un seguimiento clínico. Se utilizó estadística descriptiva, así como el análisis uni y multivariado.
Resultados: Se incluyeron 215 pacientes, n=70 (32.4%) eran varones, con una media ± DE de edad de 51 ± 20 años. La duración del procedimiento fue de 36 ± 20 min. Se realizó esfinterotomía en 113 (52.6%) casos. Se realizó precorte en 18 (8.3%) pacientes. Se observaron complications en 10 pacientes (4.7%). En el análisis multivariado, la obesidad y la duración del procedimiento, fueron factores asociados con el desarrollo de complicaciones.
Conclusión: La obesidad y estudios prolongados son factores asociados con el desarrollo de complicaciones post-CPRE.
Introduction: There have been numerous studies describing different risk factors for complications after ERCP. A prospective study to determine the frequency and associated risk factors for complications after ERCP was performed in our center.
Material and methods: The following data were recorded prospectively: indication and duration of the procedure, number of cannulation attempts, use of precut or sphincterotomy, pancreatic duct cannulation and pancreatography; patient demographics, including age, gender, height, weight and body mass index we also noted. ERCP complications were evaluated during and after the procedure. Mortality at 30 days was evaluated by clinical follow-up or records. Descriptive statistics as well as univariate and multivariate analysis were performed.
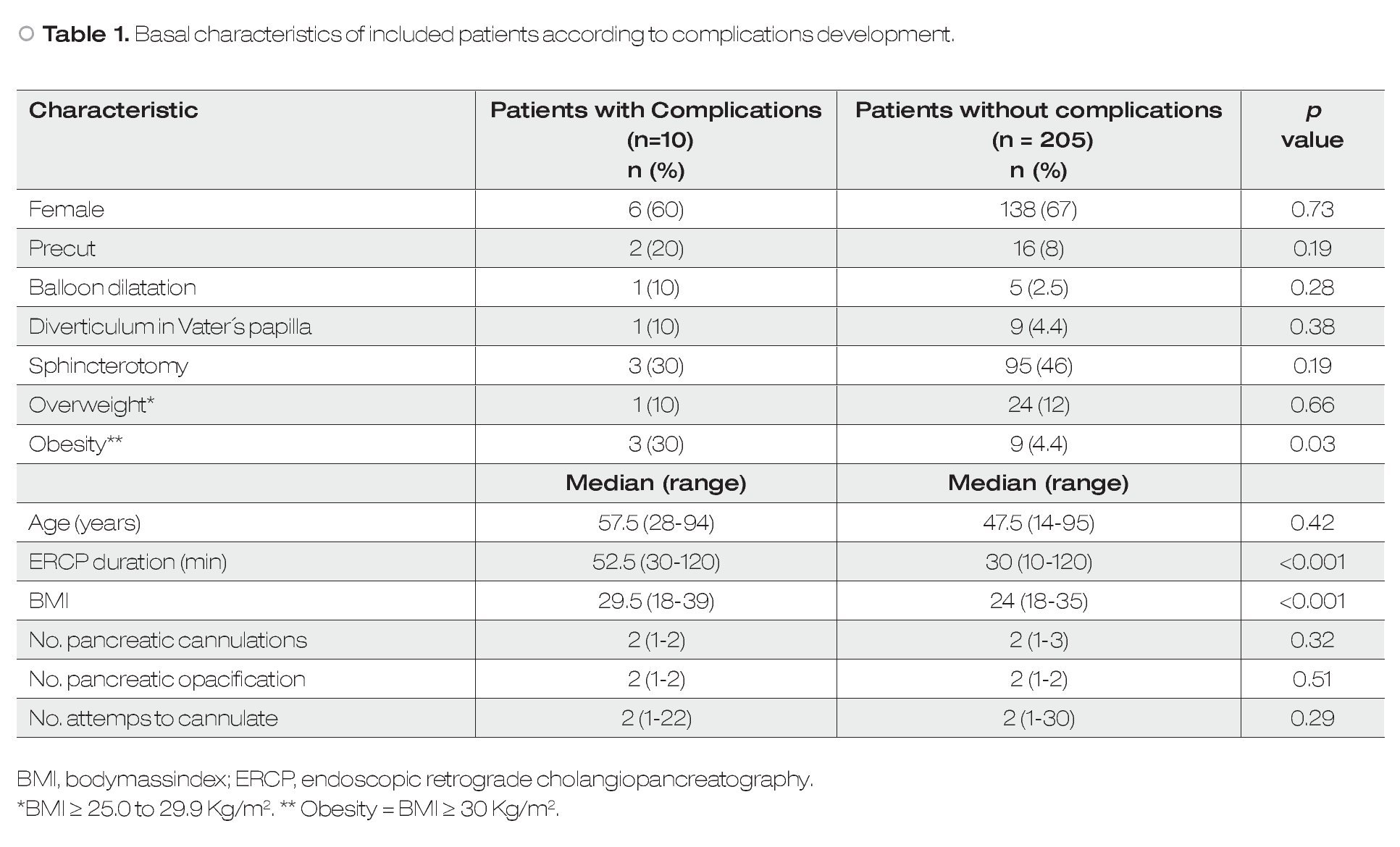
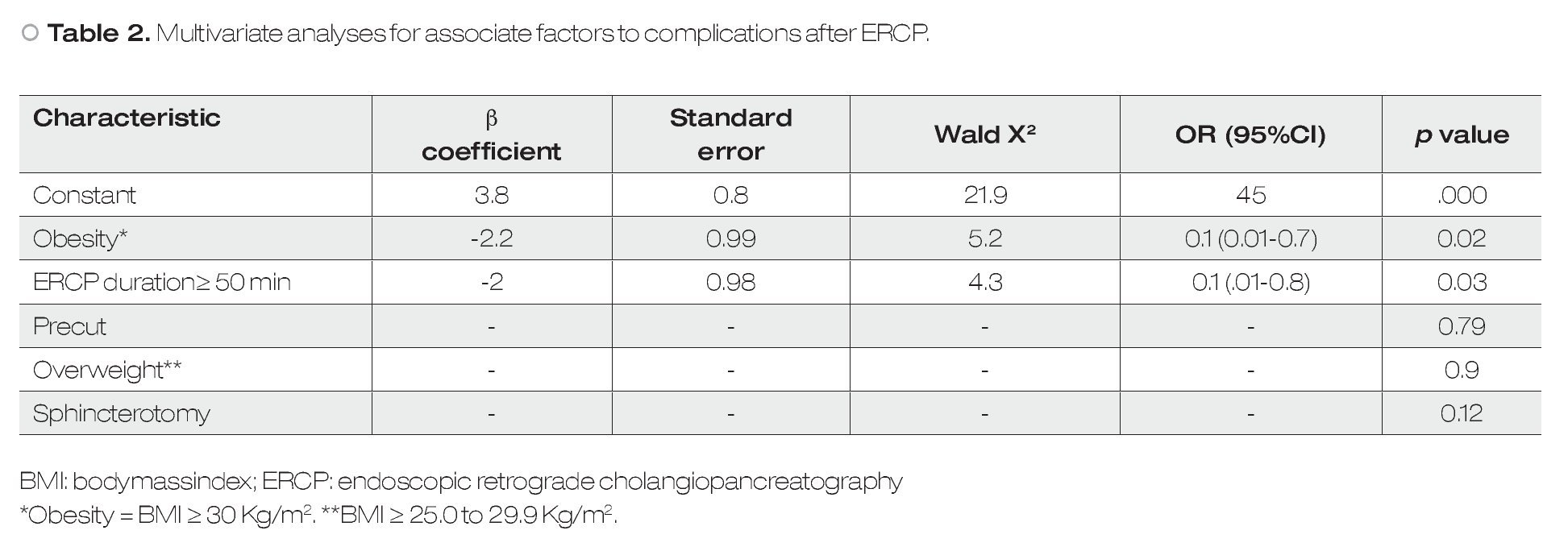
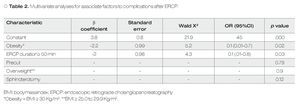
Results: A total of 215 patients were included, n=70 (32.4%) were male; mean ± SD age was 51 ± 20 years. The mean ± SD procedure duration was 36±20 min. Sphincterotomy was performed in 113 (52.6%) cases. Precut was performed in 18 (8.3%) patients. Complications were observed in n=10 patients (4.7%). On multivariate analysis, obesity and duration of the procedure were significant factors associated to development of complications.
Conclusion: Obesity and lenghty procedures are factors associated with development of post-ERCP complications in our studied population.
Introduction
The risk of serious complications associated to endoscopic retrograde cholangiopancreatography (ERCP) is well known. Published case series have reported variable complication rates for cholangitis (0% to 14%), hemobilia (0% to 3%), bile leak (1%) and pancreatitis (0% to 7%), related to ERCP.1
Noninvasive imaging such as MRCP and EUS have largely superseded diagnostic ERCP, and the safety profile of surgery has greatly improved. These facts should reduce the complication rate of ERCP to a minimal level, by ensuring that procedures are performed only when really indicated. Efforts to do identify and understand the factors that make complications more or less likely, have contributed greatly towards this aim. Several studies document the complications of ERCP and analyze various risk factors as well as predictors.2-4
The aim of this study was to determine the frequency of complications after ERCP in our center and evaluate the associate factors.
Material and methods
We conduct a prospective study of all ERCP procedures performed in our center from March 2010 to August 2010. We included all procedures performed in our institution for any indication and excluded patients in whom the procedure could not performed or declined to participate. In every case, before the first procedure, complete blood count, INR, and prothrombin time were obtained to minimize the risk of bleeding. An experienced ERCP endoscopist performed all cases. Written informed consent was obtained for each patient and all procedures were performed under deep sedation with Midazolam, Propofol and Phentanyl by an anesthesiologist.
Demographic, clinical and endoscopic data were collected; weight and height were extracted from the medical records before the study. An investigator recorded prospectively the following variables during endoscopy; indication and duration of procedure, number of attempts, use of precut, sphincterotomy, cannulation of pancreatic duct and pancreatography. ERCP complications were evaluated during and after the procedure. Mortality at 30 days was evaluated by clinical follow-up and records. ERCP was performed with standard duodenoscopes: TJF-160F, TJF-160VF (Olympus®, American Corp., Melville, NY, USA). Contrast media for cannulation was used at the discretion of each physician (Ioditrast M60®, Justesa, Imagen Mexicana, Mexico city, México). All patients were hospitalized for at least two hours after the procedure for surveillance of possible complications.
Body mass index was obtained as follows: weight/(height)2. Overweight and obesity was defined as follows: overweight = BMI ≥ 25.0 to 29.9 Kg/m2, Obesity = BMI ≥30 Kg/m2, Obesity Class I = BMI of 30.0 to 34.9 Kg/m2, Obesity Class II = BMI of 35.0 to 39.9 Kg/m2, Obesity Class III — BMI ≥40 Kg/ m2. ERCP complications were defined as described in previous papers as follows:
- Perforation: Mild: If there was the possibility or only a very leak of fluid or contrast dye; treatable with I.V. fluids and suction for ≤ three days.
Moderate: any perforation treated medically for four to 10 days.
Severe: medical treatment for more than 10 days or intervention (percutaneous or surgical).
- Pancreatitis: Mild: Clinical pancreatitis; amylase at least three times normal at more than 24 h after the procedure requiring admission for two to three days.
Moderate: Pancreatitis requiring hospitalization of four to 10 days.
Severe: Pancreatitis requiring hospitalization for more than 10 days, or hemorrhagic pancreatitis, phlegmon or pseudocyst, or intervention (percutaneous drainage or surgery).
- Bleeding: Mild: Clinical evidence of bleeding (ie, not just endoscopic); Hb level drop < 3 g; no need for transfusion.
Moderate: Transfusion: ≤ 4 units; no angiographic intervention or surgery.
Severe: Transfusion: ≥ 5 units or intervention (angiographic or surgical)
We excluded all patients with insufficient or incomplete data.
Statistical analyses
Descriptive statistics were used for demographic variables. Results are expressed as mean ± range. Comparison of quantitative data was performed using the Mann-Whitney U test. The difference in proportions of categorical data was analyzed with the Fisher exact test when the expected number of subjects was less than five, and by the Chi-square test when the number of subjects in each cell was five or more. Variables with p<0.2 probability of being associated to complications after ERCP in univariate analysis were included in the multivariate analyses. Logistic regression was used, with a p-value <0.05 considered as statistically significant. All statistical analyses were conducted using the statistics program SPSS/PC version 12.0 (Chicago, IL, USA).
Results
A total of 215 patients were included, n=70 (32.4%) were male; mean ± SD age was 51 ± 20 years. The main indications of ERCP were: choledocholithiasis in n=67 (31%), change of biliary stent n=32 (14.8%), cholangitis and biliary duct dilation n=21 (9.7%), malignant stenosis n=16 (7.4%), and acute pancreatitis with cholangitis n=4 (1.9%). Seventy-five patients had more than one indication for the procedure.
The mean ± SD of procedure duration was 36±20 min. The papilla of Vater was naive in 96/215 (44.4%). Sphincterotomy was performed in 113 (52.6%) cases. Seventeen cases were sphincterotomy extension. Precut was performed in 18 (8.3%) patients after a median of two attempts (range 1 to 30) of cannulation with sphinterotome without success.
Biliary duct was cannulated in n=191 (88.8%) patients and pancreatic duct in n=42 (19.9%) patients.
Complications were observed in n=10 patients (4.7%). The differences between patients whom developed complications and patients whom did not are shown in Table 1. Pancreatitis presented in five patients (1.9%), bleeding in three (1.4%) and perforation in two (0.9%). The multivariate analysis is shown in Table 2. No mortality was observed at 30 days.
Discussion
In this study, we observed that patients with obesity (but not overweight patients) and those in which the procedure had a longer duration (> 50 min) were more likely to present post-ERCP complications.
There are numerous previous studies in which the risk-factors associated with development of post-ERCP complications have been studied, mainly post-ERCP pancreatitis. Some of the factors commonly reported include: needle-knife sphincterotomy or precut, the number of attempts at cannulating the papilla, the number of cannulations of the main pancreatic duct (MPD), the injection of contrast medium into the MPD and the extent of MPD opacification, among others.5-8 Specifically, regarding the development of postERCP pancreatitis, the initial studies identify repeatedly precut as the most important factor. Subsequent papers however, have casted doubts on this assertion.9,10 It should be noted that initial studies were retrospective and in contrast, more recent ones are of prospective design. In our work, as well as other prospective studies, we found no evidence that performing precut had any implication related to complications. According to our data, the length of the procedure is a more important factor for the development of complications. As it is well known, most procedures in whom sphincterotomy is performed, are tend to be of longer duration, but this is not always synonymous. We believe that the association with the duration of the procedure relates to the number of attempts at cannulation of the papilla (and subsequent trauma). Our data as well as previous one support this opinion.5,6
Regarding the association with obesity found by us, this disease has been associated with multiple deleterious consequences in humans, however, there are scarce previous studies that report this association.2 Recent literature suggests that the presence of obesity may serve as an additional predictor of poor outcome from non-ERCP induced acute pancreatitis because of the increased risk of developing pancreatic necrosis and other systemic complications.11-13 Specific association between obesity and post-ERCP complications has been evaluated in two previous studies with conflicting results.2,14 The mechanism by which obesity could represent a risk factor for developing complications is unclear.
Some limitations of our study are the sample number and the observational design. Studies with larger samples and a randomized design (early vs late precut in patients with and without obesity) could help confirm our initial data. Finally, in this study all complications were considered.
In conclusion, obesity and lengthy procedures are factors associated with development of post-ERCP complications, including pancreatitis.
Financial Disclosure
All authors declare no financial disclosures.
Correspondence: Félix I Téllez-Ávila.
Department of Gastrointestinal Endoscopy, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán. Vasco de Quiroga #15. Col. Sección XVI. Del. Tlalpan. Z.P. 14000. Mexico City, Mexico.
Phone: (+5255) 5487 0900, ext: 2150.
E-mail: felixtelleza@gmail.com