Endoscopic retrograde cholangiopancreatography is a very common therapeutic procedure for a variety of biliary and pancreatic duct diseases. Procedure related complications are more frequent than in other endoscopic procedures. The most common reported complications are pancreatitis, bleeding, perforation, and infection. Subcapsular hepatic hematoma secondary to endoscopic retrograde cholangiopancreatography is a rare complication, but is potentially life-threating. The case is presented of a 25 year old patient with choledocholithiasis and cholelithiasis, who developed a subcapsular hepatic hematoma. The patient presented with an acute rupture of Glisson's capsule, which was successfully managed with surgical treatment. A review of the literature is presented, which consists of 30 cases.
La colangiopancreatografía retrógrada endoscópica es actualmente un procedimiento terapéutico muy común para el manejo de enfermedades biliopancreáticas. Las complicaciones secundarias a este procedimiento son más frecuentes que en otros procedimientos endoscópicos, dentro de las cuales la pancreatitis, hemorragia, perforación e infección son las que se presentan más a menudo. El hematoma hepático subcapsular secundario a colangiopancreatografía retrógrada endoscópica es una complicación muy rara, sin embargo esta puede poner en peligro la vida del paciente. Presentamos el caso de una paciente de 25 años con coledocolitiasis y colelitiasis que desarrolló un hematoma hepático subcapsular poscolangiopancreatografía retrógrada endoscópica con abdomen agudo y ruptura de la cápsula de Glisson que fue manejada exitosamente con tratamiento quirúrgico, así como una revisión de la literatura de 30 casos.
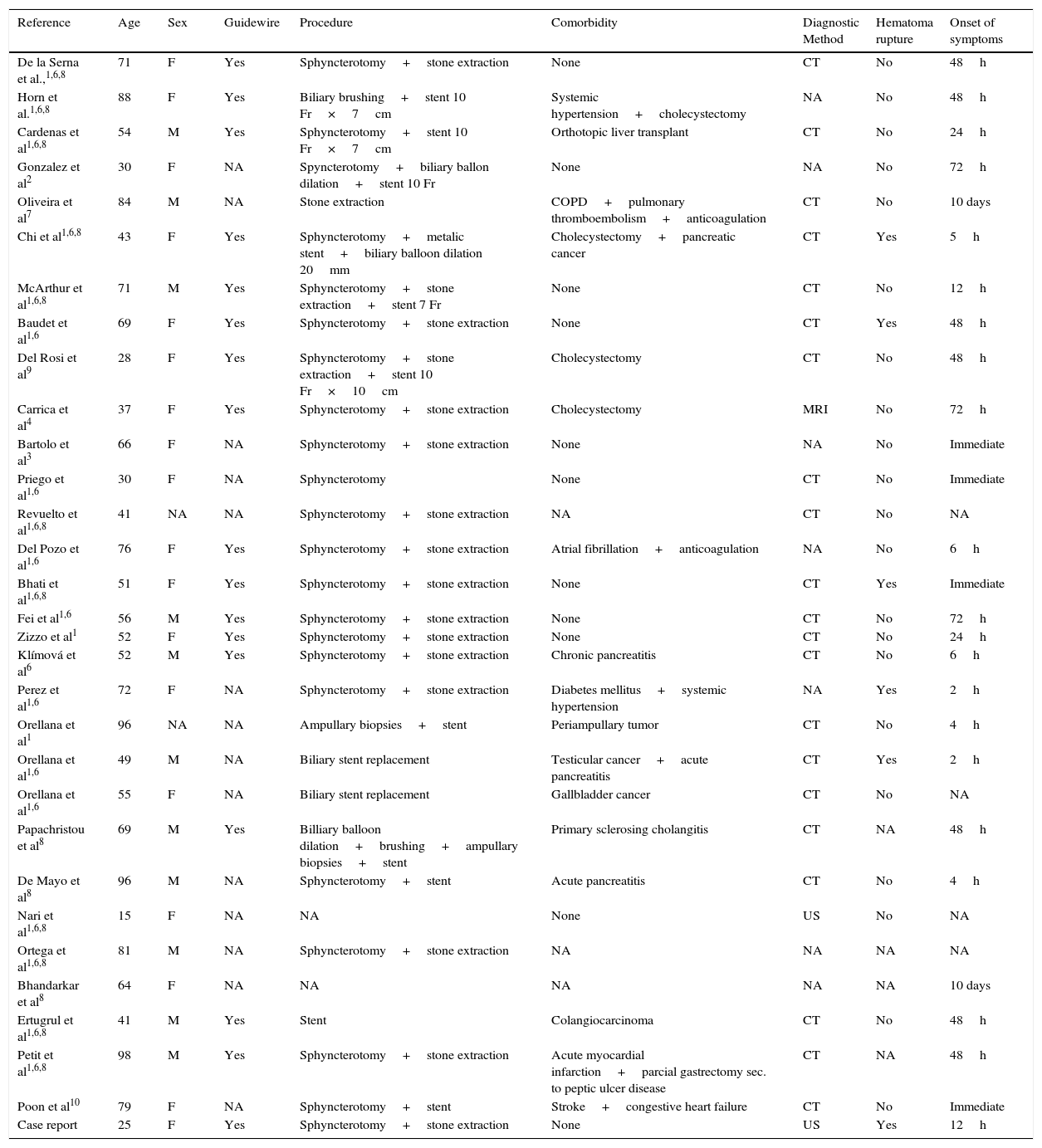
Endoscopic retrograde cholangiopancreatography (ERCP) is widely available in most hospitals and is one of the most frequently performed procedures in the treatment of biliary–pancreatic diseases. Even in centers with a high-volume of patients that present with biliary and pancreatic pathology and are subsequently treated, serious complications from therapeutic ERCP can occur in 2.5–8% of cases, with mortality ranging from 0.5% to 1.0%.1,2 Acute pancreatitis, cholangitis, hemorrhage, and perforation, the leading complications in 1–7%, 1.4%, 1%, and 1% of patients treated via ERCP respectively.2,3 Subcapsular hepatic hematoma is a rare complication following ERCP and can be life-threatening in some cases.4 The purpose of our study is to present a case of post-ERCP subcapsular hepatic hematoma which evolved with hypovolemic shock and required surgical intervention; we also review the possible pathophysiological mechanisms underlying such complication and analyze the sum of the contemporary available literature (Table 1).
Hepatic subcapsular hematoma after ERCP summary of cases.
| Reference | Age | Sex | Guidewire | Procedure | Comorbidity | Diagnostic Method | Hematoma rupture | Onset of symptoms |
|---|---|---|---|---|---|---|---|---|
| De la Serna et al.,1,6,8 | 71 | F | Yes | Sphyncterotomy+stone extraction | None | CT | No | 48h |
| Horn et al.1,6,8 | 88 | F | Yes | Biliary brushing+stent 10 Fr×7cm | Systemic hypertension+cholecystectomy | NA | No | 48h |
| Cardenas et al1,6,8 | 54 | M | Yes | Sphyncterotomy+stent 10 Fr×7cm | Orthotopic liver transplant | CT | No | 24h |
| Gonzalez et al2 | 30 | F | NA | Spyncterotomy+biliary ballon dilation+stent 10 Fr | None | NA | No | 72h |
| Oliveira et al7 | 84 | M | NA | Stone extraction | COPD+pulmonary thromboembolism+anticoagulation | CT | No | 10 days |
| Chi et al1,6,8 | 43 | F | Yes | Sphyncterotomy+metalic stent+biliary balloon dilation 20mm | Cholecystectomy+pancreatic cancer | CT | Yes | 5h |
| McArthur et al1,6,8 | 71 | M | Yes | Sphyncterotomy+stone extraction+stent 7 Fr | None | CT | No | 12h |
| Baudet et al1,6 | 69 | F | Yes | Sphyncterotomy+stone extraction | None | CT | Yes | 48h |
| Del Rosi et al9 | 28 | F | Yes | Sphyncterotomy+stone extraction+stent 10 Fr×10cm | Cholecystectomy | CT | No | 48h |
| Carrica et al4 | 37 | F | Yes | Sphyncterotomy+stone extraction | Cholecystectomy | MRI | No | 72h |
| Bartolo et al3 | 66 | F | NA | Sphyncterotomy+stone extraction | None | NA | No | Immediate |
| Priego et al1,6 | 30 | F | NA | Sphyncterotomy | None | CT | No | Immediate |
| Revuelto et al1,6,8 | 41 | NA | NA | Sphyncterotomy+stone extraction | NA | CT | No | NA |
| Del Pozo et al1,6 | 76 | F | Yes | Sphyncterotomy+stone extraction | Atrial fibrillation+anticoagulation | NA | No | 6h |
| Bhati et al1,6,8 | 51 | F | Yes | Sphyncterotomy+stone extraction | None | CT | Yes | Immediate |
| Fei et al1,6 | 56 | M | Yes | Sphyncterotomy+stone extraction | None | CT | No | 72h |
| Zizzo et al1 | 52 | F | Yes | Sphyncterotomy+stone extraction | None | CT | No | 24h |
| Klímová et al6 | 52 | M | Yes | Sphyncterotomy+stone extraction | Chronic pancreatitis | CT | No | 6h |
| Perez et al1,6 | 72 | F | NA | Sphyncterotomy+stone extraction | Diabetes mellitus+systemic hypertension | NA | Yes | 2h |
| Orellana et al1 | 96 | NA | NA | Ampullary biopsies+stent | Periampullary tumor | CT | No | 4h |
| Orellana et al1,6 | 49 | M | NA | Biliary stent replacement | Testicular cancer+acute pancreatitis | CT | Yes | 2h |
| Orellana et al1,6 | 55 | F | NA | Biliary stent replacement | Gallbladder cancer | CT | No | NA |
| Papachristou et al8 | 69 | M | Yes | Billiary balloon dilation+brushing+ampullary biopsies+stent | Primary sclerosing cholangitis | CT | NA | 48h |
| De Mayo et al8 | 96 | M | NA | Sphyncterotomy+stent | Acute pancreatitis | CT | No | 4h |
| Nari et al1,6,8 | 15 | F | NA | NA | None | US | No | NA |
| Ortega et al1,6,8 | 81 | M | NA | Sphyncterotomy+stone extraction | NA | NA | NA | NA |
| Bhandarkar et al8 | 64 | F | NA | NA | NA | NA | NA | 10 days |
| Ertugrul et al1,6,8 | 41 | M | Yes | Stent | Colangiocarcinoma | CT | No | 48h |
| Petit et al1,6,8 | 98 | M | Yes | Sphyncterotomy+stone extraction | Acute myocardial infarction+parcial gastrectomy sec. to peptic ulcer disease | CT | NA | 48h |
| Poon et al10 | 79 | F | NA | Sphyncterotomy+stent | Stroke+congestive heart failure | CT | No | Immediate |
| Case report | 25 | F | Yes | Sphyncterotomy+stone extraction | None | US | Yes | 12h |
| Reference | Age | Sex | Clinical manifestacions | Treatment | Antibiotics | Hemoglobin decrease (g/dL) | Death |
|---|---|---|---|---|---|---|---|
| De la Serna et al.,1,6,8 | 71 | F | RUC pain | Conservative | Yes | NA | No |
| Horn et al.1,6,8 | 88 | F | RUC pain+anemia | Conservative | Yes | NA | No |
| Cardenas et al1,6,8 | 54 | M | Mesogastric abdominal pain | Conservative | Yes | 3.2g/dL | No |
| Gonzalez et al2 | 30 | F | RUC pain | Surgery | Yes | NA | Yes |
| Oliveira et al7 | 84 | M | RUC pain | Percutaneous drainage | Yes | 3.3g/dL | Yes |
| Chi et al1,6,8 | 43 | F | RUC pain+anemia | Embolization | Yes | NA | No |
| McArthur et al1,6,8 | 71 | M | RUC pain | Conservative | Yes | NA | No |
| Baudet et al1,6 | 69 | F | RUC pain+fever | Embolization+surgery | Yes CF | 7.3g/dL | No |
| Del Rosi et al9 | 28 | F | RUC pain | Conservative | Yes | 7.3g/dL | No |
| Carrica et al4 | 37 | F | RUC pain | Percutaneous drainage | Yes CF | 1.3g/dL | No |
| Bartolo et al3 | 66 | F | Hypotension+tachycardia | Surgery | No | 10.3g/dL | Yes |
| Priego et al1,6 | 30 | F | RUC pain | Surgery | Yes | NA | No |
| Revuelto et al1,6,8 | 41 | NA | Anemia | Conservative | Yes | NA | No |
| Del Pozo et al1,6 | 76 | F | RUC pain | Conservative | Yes | NA | No |
| Bhati et al1,6,8 | 51 | F | RUC pain+hypotension | Percutaneous drainage | NA | NA | No |
| Fei et al1,6 | 56 | M | RUC pain | Percutaneous drainage | Yes | NA | No |
| Zizzo et al1 | 52 | F | Epigastric pain | Embolization | Yes | 3.3g/dL | No |
| Klímová et al6 | 52 | M | RUC pain | Embolization | Yes | 6g/dL | No |
| Perez et al1,6 | 72 | F | RUC pain | Surgery | NA | NA | No |
| Orellana et al1 | 96 | NA | Right omalgia | Conservative | Yes | NA | No |
| Orellana et al1,6 | 49 | M | RUC pain | Embolization | NA | NA | No |
| Orellana et al1,6 | 55 | F | RUC pain+right omalgia | Conservative | NA | NA | No |
| Papachristou et al8 | 69 | M | RUC pain+right omalgia+anemia | Conservative | NA | 3.5g/dL | NA |
| De Mayo et al8 | 96 | M | Right omalgia | Conservative | Yes | NA | No |
| Nari et al1,6,8 | 15 | F | RUC pain+right omalgia+hypotension | Conservative | Yes | NA | No |
| Ortega et al1,6,8 | 81 | M | RUC pain | Percutaneous drainage | Yes | NA | NA |
| Bhandarkar et al8 | 64 | F | RUC pain+fever+anemia | Percutaneous drainage | NA | NA | NA |
| Ertugrul et al1,6,8 | 41 | M | RUC pain+fever | Conservative | Yes | NA | No |
| Petit et al1,6,8 | 98 | M | RUC pain+asthenia | Percutaneous drainage | NA | NA | NA |
| Poon et al10 | 79 | F | RUC pain+hypotension | Conservative | NA | 5g/dL | No |
| Case report | 25 | F | RUC pain+anemia | Surgery | Yes | 4.2g/dL | No |
F – female, M – male, COPD – Chronic Obstructive Pulmonary Disease, RUC – right upper cuadrant, CT – computed tomography, US – ultrasound, MRI – magnetic resonance image, NA – not available, CF – Citrobacter freundii.
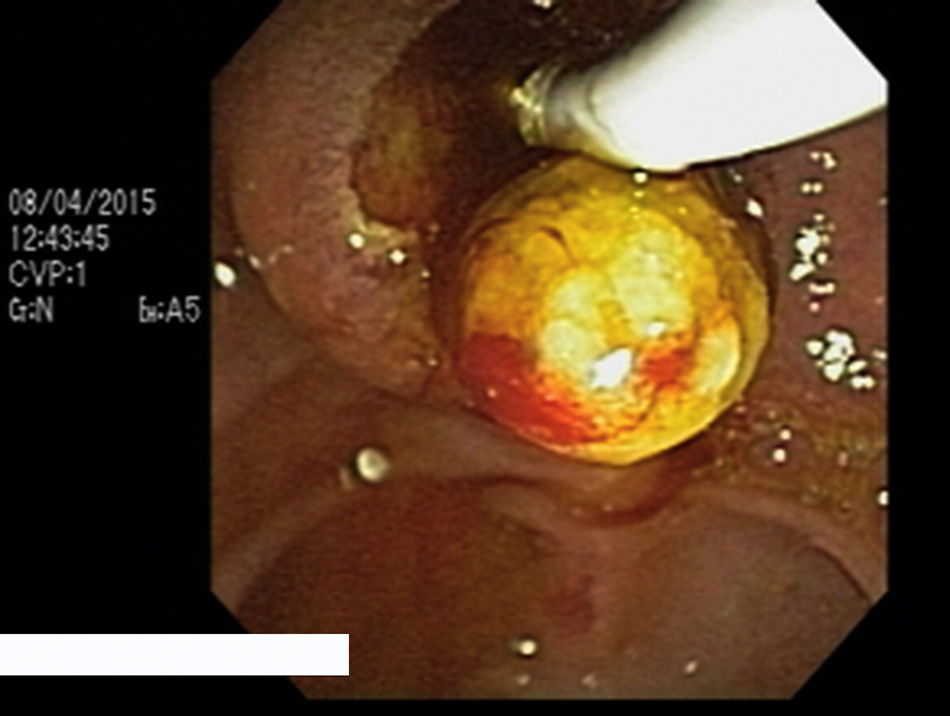
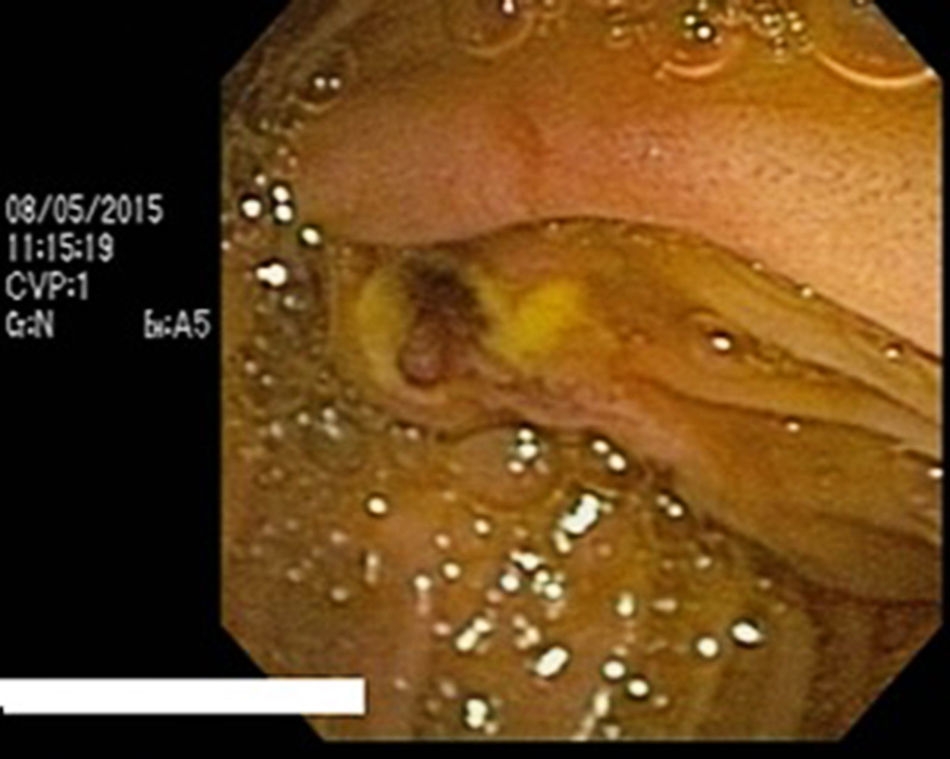
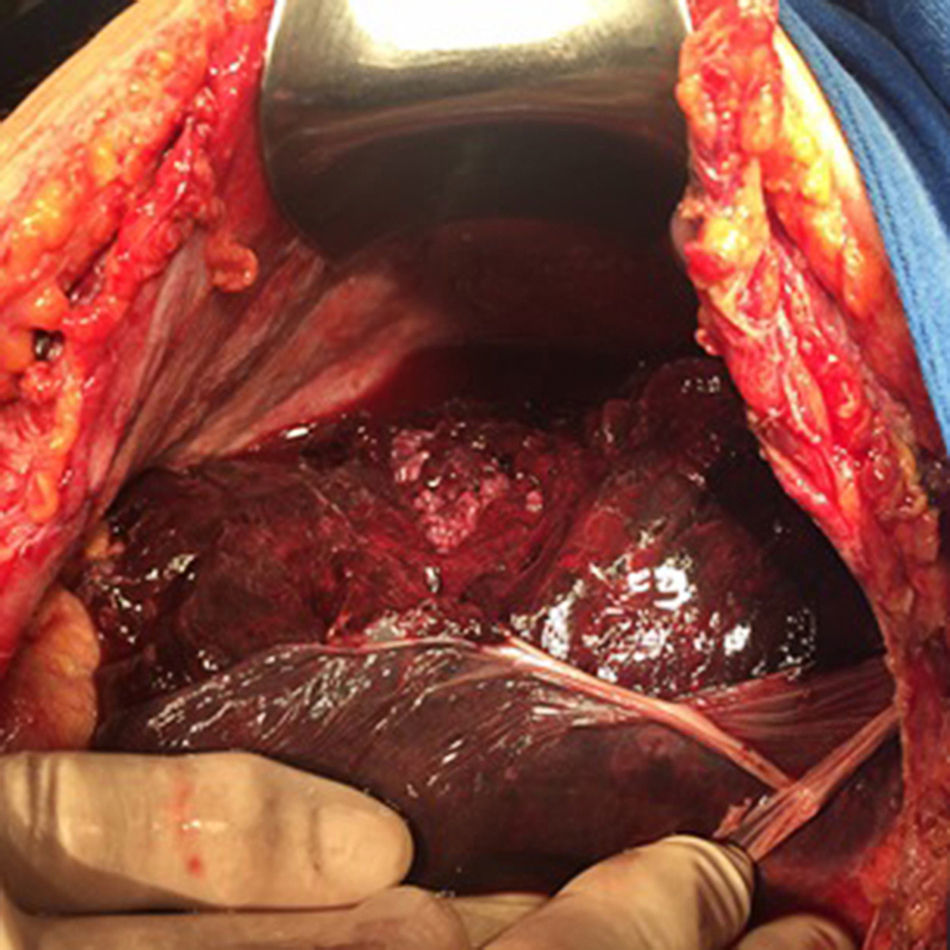
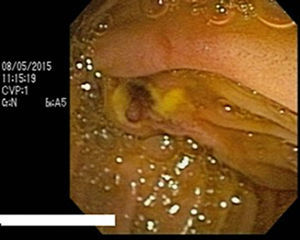
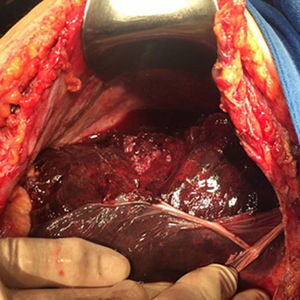
A 25-year-old female with a history of pregnancy and C section 7 months prior to admission presented with recurrent abdominal pain in the upper right quadrant 15 days prior admission, the pain was accompanied by nausea, vomititing, and jaundice. Laboratory report showed the following: WBC 5.51×1.000/μL, Hemoglobin 11.5g/dL, platellet count of 310×1.000/μL, prothrombin time ratio 13.3, international normalized ratio 1.16, aspartate aminotransferase 128U/L, alanine aminotransferase 125U/L, Total Bilirubin 3.57mg/dL, Direct Bilirubin 2.96mg/dL, alkaline phosphatase 928U/L. An MRCP revealed intra and extrahepatic bile duct dilation with a defect in the distal portion of the common bile duct. ERCP with biliary sphincterotomy over a 0.035-inch diameter guidewire was performed, cannulation of the papilla on a first attempt without difficulty following the insertion of a 16mm stone extraction balloon catheter (Shaili Endoscopy®) obtaining one yellow round bile duct stone of 5mm of diameter (Fig. 1), control cholangiography showed no residual defects and the procedure was finished without evident complications such as bleeding or injury. 12h post procedure the patient developed right upper quadrant abdominal pain, hemoglobin dropped 4g/dL (Hb 7.3g/dL), amylase spiked to 162U/L and lipase also showed a rise to 213U/L. There was no clinical evidence of gastrointestinal bleeding. An upper endoscopy was performed with a frontal video endoscope and a duodenoscope without evidence of gastrointestinal bleeding or post-sphyncterotomy bleeding (Fig. 2). Three packed red blood cells (PRBCs) were transfused, and a 12h post transfusional hemoglobin was obtained which reported 10.3g/dL. Hemoglobin declined to 5.3g/dL 3 days after ERCP. The patient developed grade 4 hypovolemic shock with acute abdomen and positive Blumberg sign. An urgent abdominal ultrasound revealed free fluid in the abdominal cavity. Two more PRBCs were transfused and an urgent laparotomy was performed observing rupture of Glisson's capsule (Fig. 3) and approximately 3000ml of blood in the peritoneal cavity was found. Abdominal packing was performed and two more PRBCs were transfused during surgery. The patient was admitted to the Intensive Care Unit (ICU) where she had to have assisted breathing via endotracheal tube. There was no need for vasoactive support. 48h later a second laparotomy was performed to unpack the abdomen. The patient was extubated 6 days after the first laparotomy and was discharged from the ICU. The patient evolved well, maintaining hemoglobin levels at 10.9g/dL and was discharged from the hospital 16 days after the ERCP procedure. One month later a follow-up MRI demonstrated a remanent heterogenic subcapsular hepatic hematoma of 15.2×10.4×3.6cm in the right hepatic lobe (Fig. 4). Currently, the patient is (3 months post ERCP) generally well and reports slight abdominal discomfort, patient surveillance will continue until complete resolution of the hematoma is observed.
Bleeding related to an ERCP procedure is usually due to endoscopic sphincterotomy. Bleeding seen endoscopically during or immediately after sphincterotomy is not uncommon, but is generally not considered an adverse event unless there is significant blood loss, which is manifested as evident hypovolemia and/or that has a need for transfusion. When applying clinical criteria such as melena, hematemesis, a drop greater than 2g/dL in hemoglobin level, or requirement for secondary intervention such as endoscopy or blood transfusion, the overall incidence of bleeding is around 0.1–2% even in experienced hands.5 Subcapsular hepatic hematoma is a rare and exceptional event, of which only 30 cases have been reported since 2000. The pathophysiologic mechanism underlying the development of the hematoma is not clearly defined, however various authors agree that vascular injury of small-caliber intrahepatic vessels secondary to guidewire use may be the cause, which may also explain the presence of free air and development of infections in some of the cases.1,6
Patient factorsWe found that the median age of presentation is 59 (15–98) years, with 58% female and 35% male distribution. Only 2 (6.4%) patients had a history of anticoagulation therapy prior to the procedure. Almost half of the patients (48.3%) presented clinical manifestations in the first 24h post-ERCP. The most common manifestation was abdominal pain in 87%; in some case reports fever was mentioned to be one of the primary manifestations, but we found that right omalgia and clinical manifestations of hypovolemic shock (tachycardia or hypotension) were present more often 9.6% vs 16.1% vs 12.9%.
Procedure factorIn 17 (54.8%) cases the use of a guide wire was reported, but we cannot exclude its use on the other 14 cases. The literature on these 14 cases does not mention the use of a guide wire.
In most of the cases, 67.7%, diagnosis was performed by CT, but the use of US and MRI was also described in 2 and 1 cases respectively. In our case report abdominal US was performed searching for free fluid in the abdominal cavity, because of the development of an acute abdomen. In almost half of the patients (45.1%) no invasive treatment was required. Percutaneous drainage was performed in 7 (22.5%), surgery in 6 (19.3%), and embolization in 4 (12.9%) patients. Only 2 case reports described the pathogen found in the hematoma culture, both found Citrobacter freundii, which is a facultative aerobic gram-negative bacilli of the Enterobacteriaceae family, commonly found in the gastrointestinal tract. In 22 (70.9%) patients antibiotics where used, either as a prophylactic measure or as treatment for infection, 8 (25.8%) did not specify whether they used antibiotics or not. Only 11 case reports mention a decrease in hemoglobin that went between 1.3g/dL to 10.3g/dL, and from those cases, the majority, 63%, required some kind of intervention (embolization, percutaneous drainage or surgery), concluding that hemoglobin decrease is a good predictor for requiring intervention, no association was found between hemoglobin drop and the need of a specific kind of intervention. 3 (9.6%) deaths were reported, 2 patients who required surgery and one in whom percutaneous drainage was performed.
Because of the mortality rate found in the literature it is important to consider this as a life-threatening adverse event. Another rare complication following ERCP that can have a similar presentation as described in the case report is injury to the spleen causing intraperitoneal hemorrhage with a few cases being reported in the literature. Symptoms often include localized peritoneal irritation in the left upper quadrant progressing with time to generalized peritonitis, along with referred pain to the left shoulder. Changes in vital signs including tachycardia and orthostatic changes in blood pressure are frequent.
ConclusionsSubcapsular hepatic hematoma is a rare condition associated to ERCP that must be suspected when abdominal pain is present after the procedure, it may have a fatal course if it is not diagnosed and treated early. Further publications of case reports will help establish risk factors and appropriate treatment.
FinancingNo funding was received for this work.
Conflict of interestsAuthors declare no conflict of interests for this article.
Endoscopy magazine is the only magazine in which the work under review is published.