We present the case of an obese 47-year-old woman from the Dominican Republic, living in Spain since 2003. She came to our outpatient department reporting a 15-day-history of painful nodules and ulcerations on the abdomen that had been treated by her general practitioner with amoxicilin/clavulanate 875/125mg t.i.d. for 7 days with no improvement. She mentioned that 8 weeks previously, during a vacation trip to her country, she had undergone a mesotherapy session with injections of a liquid formula containing phosphatidylcholine to reduce the fat from her abdomen.
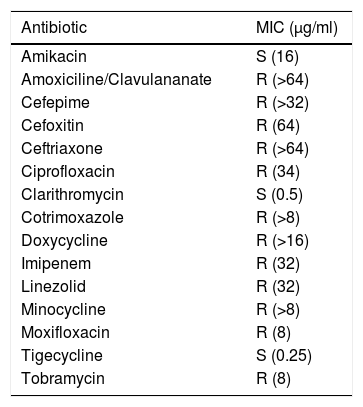
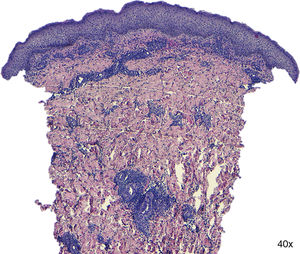
On physical examination redness, swelling, drainage and ulceration were seen at the sites of mesotherapy injection (Fig. 1). Ultrasound imaging revealed subcutaneous edema, but no signs of deep abscessification, and MRI (T2) showed fat necrosis at the sites of injection. A punch biopsy was performed. Histopathologic examination revealed only mild dermoepidermal edema and a mixed infiltrate on the dermis without granulomas (Fig. 2). Periodic-Acid Schiff (PAS) and silver staining were negative as well as Ziehl-Neelsen. Mycobacterium abscessus was identified on skin cultures. Antibiogram is shown in Table 1.
Drug susceptibility testing assay: antibiogram and minimal inhibitory concentration (μg/ml).
| Antibiotic | MIC (μg/ml) |
|---|---|
| Amikacin | S (16) |
| Amoxiciline/Clavulananate | R (>64) |
| Cefepime | R (>32) |
| Cefoxitin | R (64) |
| Ceftriaxone | R (>64) |
| Ciprofloxacin | R (34) |
| Clarithromycin | S (0.5) |
| Cotrimoxazole | R (>8) |
| Doxycycline | R (>16) |
| Imipenem | R (32) |
| Linezolid | R (32) |
| Minocycline | R (>8) |
| Moxifloxacin | R (8) |
| Tigecycline | S (0.25) |
| Tobramycin | R (8) |
The patient began treatment with doxycycline 100mg b.i.d and clarithromycin 500mg b.i.d for 2 months. Although identification of Mycobacterium abscessus subspecies was not provided, drug susceptibility testing assay showed a pattern of multidrug resistance except for clarithromycin. Therefore, doxycycline was stopped, and clarithromycin was administered 1g b.i.d during the following 4 months. The patient completed a six-month course of antibiotics with complete resolution of the swelling, drainage and ulceration, but the lesions resolved with hypertrophic scars. Some of the scars were surgically excised to get a better esthetic result and to discard the possibility of persisting infection. Cultures and PCR for mycobacterium of the samples were negative, confirming the cure of the infection.
CommentaryMesotherapy is a treatment involving local subcutaneous injections of minute quantities of various substances for cosmetic purposes (non-steroidal anti-inflammatory medications, enzymes, nutrients, antibiotics, hormones, vitamins or plant extracts). Mesotherapy may be used to aid weight loss in conjunction with dietary modification, hormone replacement therapy, exercise and nutritional supplements. Both infectious and noninfectious complications of mesotherapy have been described previously. However, injection-site infections with non-tuberculous mycobacteria are often reported.
Mycobacterium abscessus is an atypical fast-growing mycobacterium, ubiquitous in the environment that can be found in water, soil and dust. Several outbreaks of M. abscessus skin and soft tissue infections have been reported1 mostly associated with medical procedures,2 cosmetic surgery,3 acupuncture and tattoos.4
The skin infection typically presents as nodules, recurrent abscesses or non-healing ulcers. Multiple lesions may be observed at the same time.5 The diagnosis is confirmed by positive cultures from drainage material, surgical debridement or skin biopsy. However, the isolation of M. abscessus is very difficult. Therefore, PCR, a rapid diagnostic method that allows both diagnosis and species identification, can be performed. Differential diagnosis is broad and bacterial and fungal infections, granulomatous and tumoral diseases must be ruled out.5,6 However, mycobacterium infection secondary to mesotherapy must be suspected when lesions appear in a geometrical pattern or match the sites of mesotherapy injections.
Infections due to M. abscessus are difficult to treat because these mycobacteria are intrinsically resistant not only to the classic anti-tuberculous drugs, but also to most of the antibiotics that are currently available.6,7M. abscessus can be divided into at least three subspecies: M. abscessus abscessus, M. abscessus massiliense, and M. abscessus bolletii which is rarely isolated. The 2 major subspecies, M. abscessus abscessus and M. abscessus massiliense, have different erm(41) gene patterns, which provides M. abscessus abscessus intrinsic resistance to macrolides. For this reason, an individualized therapeutic approach, based on a combination of minimum 2 antibiotics is usually recommended. Surgical management of atypical mycobacterial is sometimes required.8,9
To minimize the risk of infectious complications from mesotherapy, providers should adhere to recommended standard precautions, and follow safe-injection practices with appropriate aseptic techniques, although there are currently no FDA-approved injectable drugs for fat elimination.