Clostridium difficile infection (CDI), the leading cause of nosocomial diarrhoea, is associated with increased patient mortality and healthcare costs.1,2 In addition, it has been observed that 12–18% of patients may progress to serious disease and 20% may have recurrences.3 Given these significant percentages, it is necessary to gain insight into which patients have CDI that is likely to follow a poor clinical course in order to select a suitable treatment and prevent mortality. Various risk factors for predicting the infection's seriousness, mortality and recurrence have been examined; however, no consensus has been reached. At present, the clinical criteria that are collected during the CDI episode are insufficient to predict the course of the infectious episode.4 Therefore, prior studies have assessed microbiological data so as to improve the prognosis and clinical course of CDI.5,6 These data include the link between the real-time PCR cycle threshold (Ct) and mortality,7 which would constitute an objective and early method.
The goal of this study was to evaluate the role of PCR Ct with a prognosis of clinical severity as a potential predictive marker of a poor clinical course for CDI.
We conducted a retrospective study at our hospital in 62 patients with microbiological detection of C. difficile (CD) in faeces using the Xpert®C. difficile system (GeneXpert, Cepheid, Sunnyvale, CA, United States) between January 2015 and December 2016. To this end, we enrolled in the study patients with samples of diarrhoeal faeces with suspected CDI that had been processed according to the established protocol (3-step algorithm) based on glutamate dehydrogenase immunochromatography (Wampole® C. DIFF QUIK CHEK®, Alere), toxin detection (Wampole® TOX A/B QUIK CHEK®, Alere) and real-time PCR (XpertTMC. difficile) the same day they arrived at the microbiology department, having been stored at 2–8°C until they were processed. Samples were collected in a sterile bottle with no transport medium.
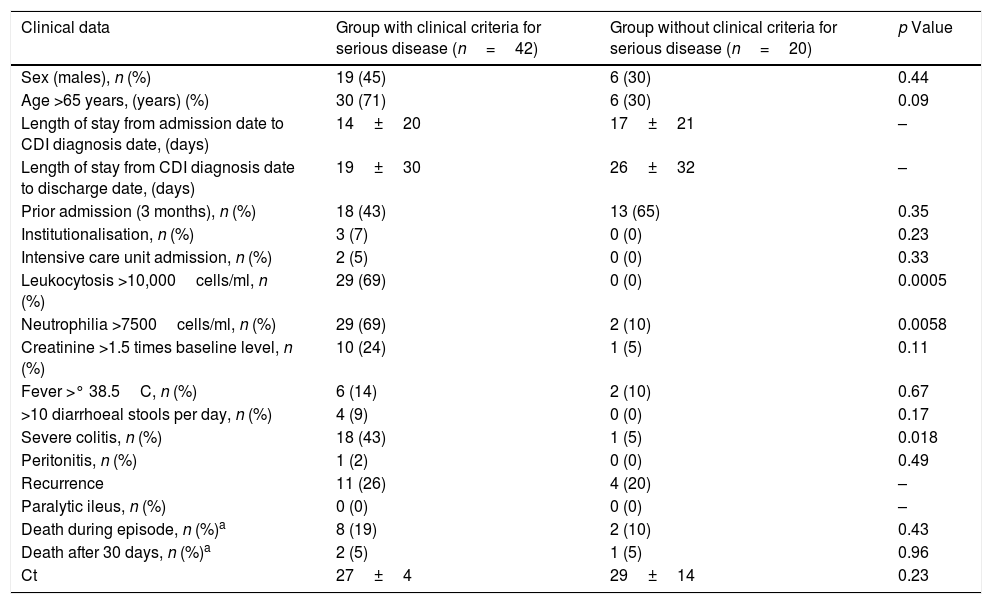
Serious CDI was defined, according to the criteria of the SHEA-IDSA, as the presence of at least 2 of the following factors: signs and symptoms of serious colitis due to CD, admission to an intensive care unit, age >65 years, leukocytosis in excess of 10,000cells/mm3, neutrophilia >7500cells/ml, increased creatinine ≥1.5 times the baseline value, temperature >38.5°C, >10 diarrhoeal stools per day, paralytic ileus, peritonitis and colitis on examination through a computed tomography scan. These seriousness factors were those that were subsequently linked to the Ct. Other variables were also analysed: sex, length of stay from admission to CDI diagnosis, length of stay from CDI diagnosis to discharge, admission in the 3 months prior to CDI, institutionalisation, death during the current episode, death after 30 days and recurrence. Next, patients were divided into 2 categories: those with clinical criteria for serious CDI and those without criteria for serious CDI. The results are shown in Table 1.
Clinical and epidemiological data for the groups studied.
| Clinical data | Group with clinical criteria for serious disease (n=42) | Group without clinical criteria for serious disease (n=20) | p Value |
|---|---|---|---|
| Sex (males), n (%) | 19 (45) | 6 (30) | 0.44 |
| Age >65 years, (years) (%) | 30 (71) | 6 (30) | 0.09 |
| Length of stay from admission date to CDI diagnosis date, (days) | 14±20 | 17±21 | – |
| Length of stay from CDI diagnosis date to discharge date, (days) | 19±30 | 26±32 | – |
| Prior admission (3 months), n (%) | 18 (43) | 13 (65) | 0.35 |
| Institutionalisation, n (%) | 3 (7) | 0 (0) | 0.23 |
| Intensive care unit admission, n (%) | 2 (5) | 0 (0) | 0.33 |
| Leukocytosis >10,000cells/ml, n (%) | 29 (69) | 0 (0) | 0.0005 |
| Neutrophilia >7500cells/ml, n (%) | 29 (69) | 2 (10) | 0.0058 |
| Creatinine >1.5 times baseline level, n (%) | 10 (24) | 1 (5) | 0.11 |
| Fever >° 38.5C, n (%) | 6 (14) | 2 (10) | 0.67 |
| >10 diarrhoeal stools per day, n (%) | 4 (9) | 0 (0) | 0.17 |
| Severe colitis, n (%) | 18 (43) | 1 (5) | 0.018 |
| Peritonitis, n (%) | 1 (2) | 0 (0) | 0.49 |
| Recurrence | 11 (26) | 4 (20) | – |
| Paralytic ileus, n (%) | 0 (0) | 0 (0) | – |
| Death during episode, n (%)a | 8 (19) | 2 (10) | 0.43 |
| Death after 30 days, n (%)a | 2 (5) | 1 (5) | 0.96 |
| Ct | 27±4 | 29±14 | 0.23 |
CDI: Clostridium difficile infection; Ct: threshold cycle.
Among the seriousness criteria studied, we found significant differences (p<0.05) between the two groups with respect to leukocytosis >10,000cells/ml, neutrophilia >7500cells/ml and serious colitis. The Ct obtained was 12±13 in patients with recurrence and 27±13 in patients with related mortality.
Although the Ct in patients with serious CDI was lower, we were unable to demonstrate any significant differences between the two groups. Similarly, a recent study by Rao et al.8 found no correlation between Ct values and severe CDI or mortality. However, a recent study by Reigadas et al.3 evaluated Ct values for PCR amplification as a prognostic factor. It should be noted that our study did not have the same methodology as the above-mentioned studies. One notable limitation of our study was its limited number of samples.
Nevertheless, we wish to stress that it is important to conduct more studies to determine whether the Ct could be a good predictor of recurrence, seriousness and/or mortality in episodes of CDI, since this would be a simple, objective marker available at the time of diagnosis.
Please cite this article as: Sante L, Pedroso Y, Castro B, Lecuona M. ¿Existe relación entre el ciclo umbral de la reacción en cadena de la polimerasa y el riesgo de infección grave por Clostridium difficile? Enferm Infecc Microbiol Clin. 2018;36:600–601.