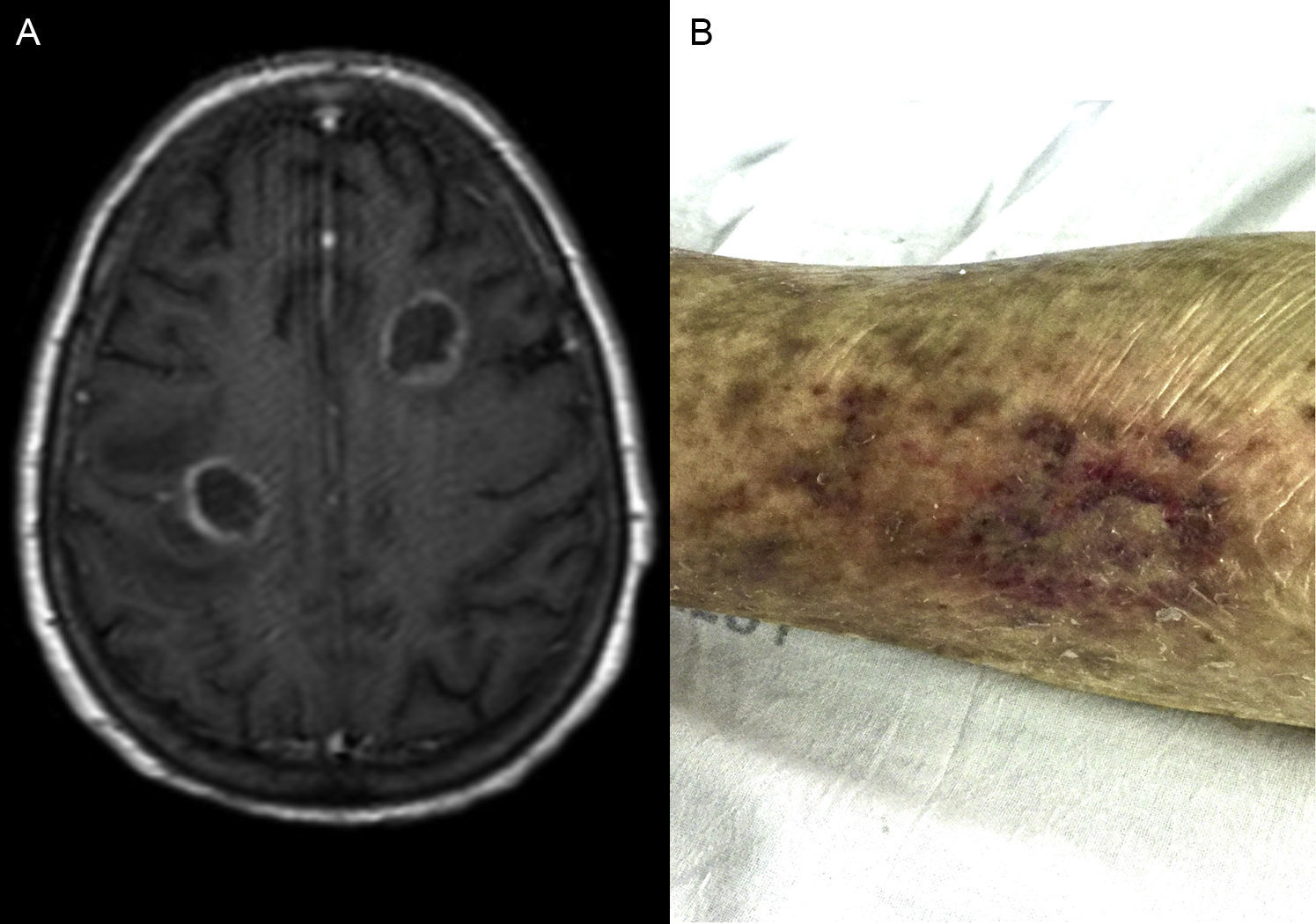
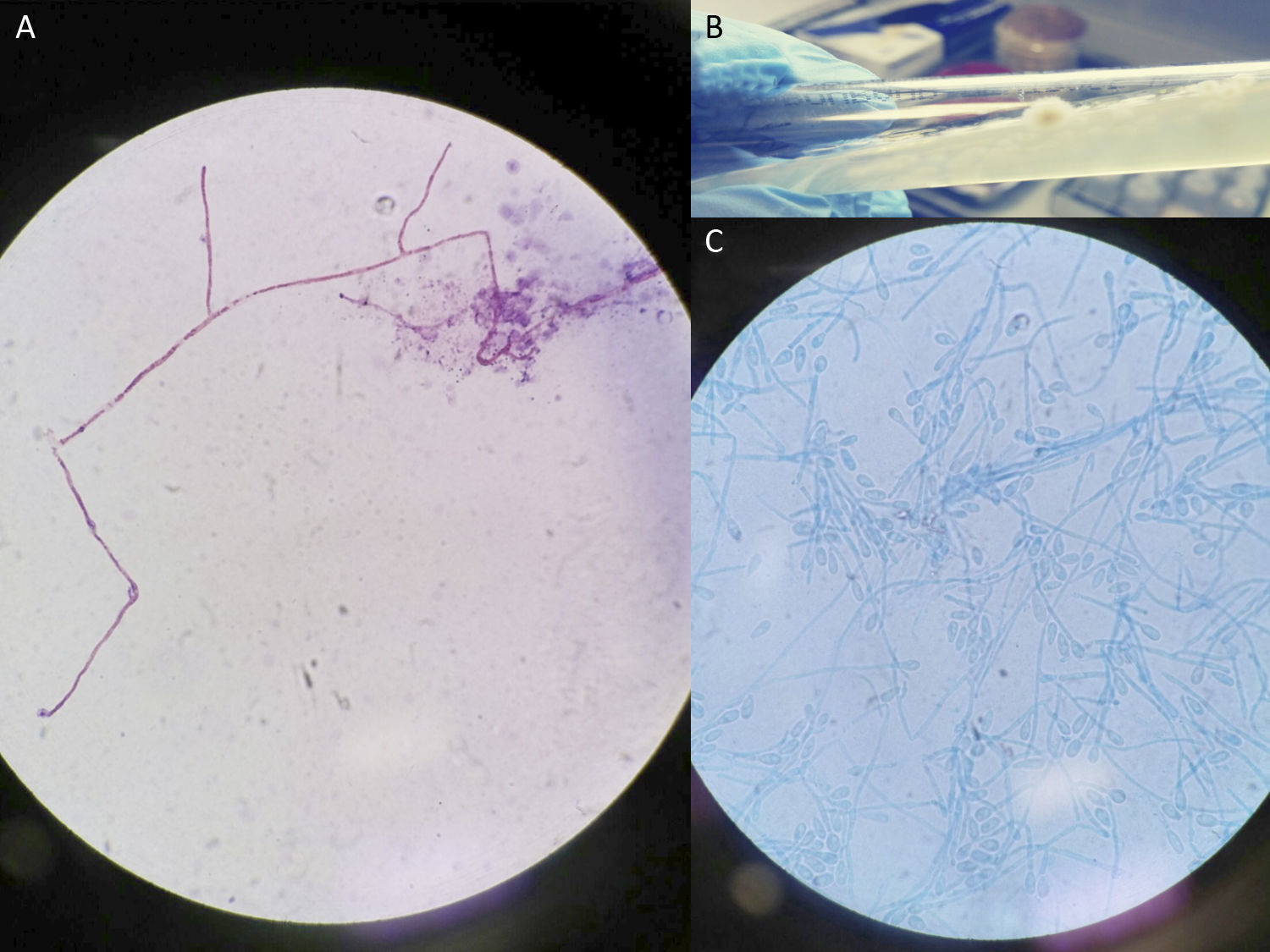
A 75-year-old kidney transplant patient developed left hemiparesis and hemihypesthesia and nodular cutaneous lesions on day +72 after transplantation. Her medical history was remarkable for hypertension, hypothyroidism, steroid-induced diabetes mellitus, permanent atrial fibrillation and a myocardial infarction. In September 2015, she received a deceased-donor kidney transplantation. After induction with thymoglobulin 250mg, she was on tacrolimus 3mg/day, mycophenolate mofetil 4000mg/day, prednisone 30mg/day and prophylactic valganciclovir and trimethoprim/sulfamethoxazole. Seven weeks after transplantation she was admitted for ultrasound-guided drainage of a 8.1cm×6.2cm lymphocele compressing the urinary tract; all microbiological cultures of the liquid drained were negative. On the day +72 after transplantation, she developed left hand paresis and hypoesthesia. An urgent brain CT-scan was informed as suggestive of subacute middle cerebral artery stroke; anticoagulation was then restored. An echocardiogram was negative for endocarditis. The following days she developed left hemiparesis and hemihypesthesia and stupor. A cerebral magnetic resonance was performed (Fig. 1A) showing multiple supratentorial space-occupying-lesions with peripheral contrast enhancement surrounded by edema. Two 0.5cm diameter nodular abscessified cutaneous lesions were noted in her left thigh (Fig. 1B). Aspergillus and cryptococcal antigen test in serum were both negative. Empiric treatment was then initiated with meropenem, linezolid, amphotericin B and trimethoprim/sulfamethoxazole and her immunosuppressive treatment was cut down to prednisone. A cutaneous biopsy of a left thigh lesion showed septal panniculitis; no bacteria nor fungi were seen on histology. A Gram stain from the material drained was performed (Fig. 2A). Two days later, some colonies started to grow on the Sabouraud Medium (Fig. 2B and C). What is your diagnosis?
Cutaneous and cerebral abscesses caused by Scedosporium apiospermum.
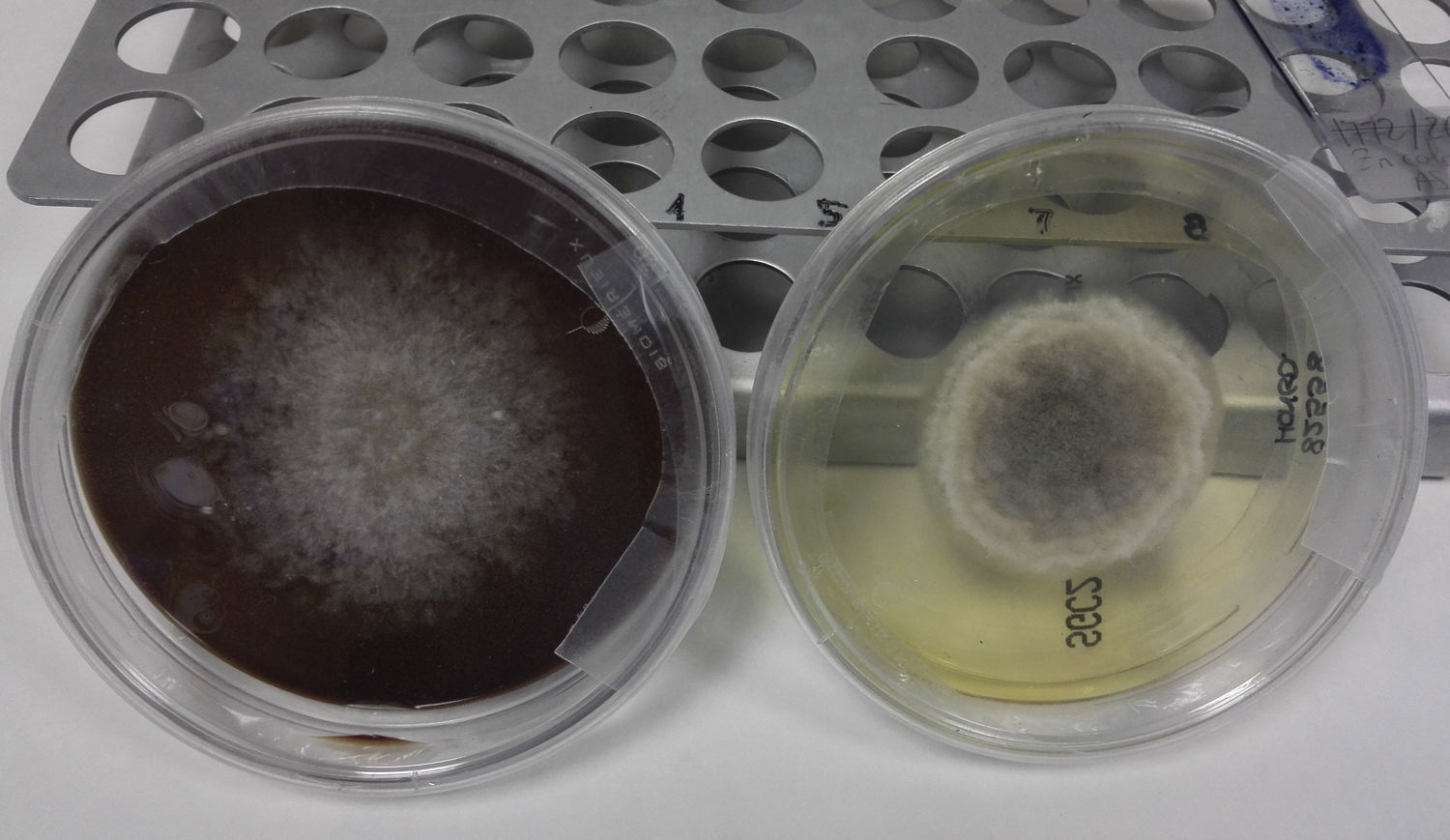
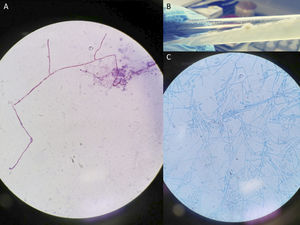
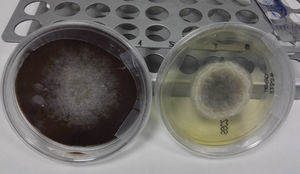
ProgressSkin abscess Gram stain showed hyphae (Fig. 2A) and in solid and liquid culture medium grew fungal colonies (Fig. 2B) that, when stained with lactophenol cotton blue, revealed typical ovoid conidia suggestive of Scedosporium spp. (Fig. 2C). It was preliminarily identified by Maldi-TOF as S. apiospermum (score=1.5); antifungal therapy was then changed to voriconazole and terbinafine. Two days later, a stereotaxic biopsy and drainage of a cerebral abscess was performed; cultures also grew S. apiospermum (Fig. 3). A PCR done at the Mycology Reference Laboratory of the National Center for Microbiology confirmed gender and specie identification. Antifungal susceptibility tests showed MIC of 4μg/ml to amphotericin B, 2μg/ml to voriconazol, 0.03μg/ml to miconazole and anidulafungin, >16μg/ml to terbinafine and >8μg/ml to itraconazole and posaconazole. Antifungal therapy was changed to voriconazole plus anidulafungin. Adjunctive neurosurgical intervention was dismissed. Patient's level of consciousness progressively deteriorated, cerebral abscesses progressed, she developed several complications and passed away 25 days after the diagnosis.
DiscussionS. apiospermum is an ubiquitous filamentous fungus present in soil, sewage and polluted waters.1 Human infection often results from inhalation of spores or through direct inoculation. Transmission from nearly-drowned donors to solid organ allografts has been reported.2 In our case, the donor died of a penetrating ocular traumatism with a wooden stick; all donor routine cultures were reviewed and confirmed to be negative for fungal pathogens. Main risk factor for scedosporiosis is neoplasia, especially hematological malignancies with prolonged persistent neutropenia.3 Scedosporiosis represents approximately 25% of all non-Aspergillus mold infections in solid organ transplant (SOT) recipients, affecting more frequently lung transplant recipients.4 Central nervous system involvement is present in 30% of cases and associated with higher mortality5,6; it usually presents as brain abscesses although spinal pachymeningitis, acute or chronic meningitis, intraventricular device-related ventriculitis or epidural abscesses have also been described.7,8 Microbiological diagnosis is difficult but can be facilitated by the use of real-time PCR assays.9 Scedosporiosis overall mortality is 54–73% in SOT and goes up to 87.5% in disseminated disease.5,6 A correct antifungal treatment, surgical debridement and a strong tailored reduction in immunosuppressant drugs are key to success.3,5Scedosporium spp. are usually amphotericin B resistant; identification to species level is key to direct treatment, as there are species-specific differences in antifungal specificity.10 The use of prophylaxis or preemptive treatment in high-risk colonized patients or receptors of grafts from nearly-drowned donors, the optimal combination antifungal therapy or the need for secondary chemoprophylaxis are unresolved questions.
In conclusion, physicians should consider Scedosporium spp. as a possible cause of brain abscesses in SOT recipients, especially in those more heavily immunosuppressed and combined antifungal therapy must be promptly started.
FundingNone declared.
Conflict of interestAll authors declare no competing interests.
We are in debt with our colleagues from the Intensive Care Unit, Neurosurgery and Nephrology Department for their invaluable collaboration in this case. We want to especially thank Dr. Mar Masiá, from the Infectious Diseases Department who took care of the patient and contributed significantly to this manuscript. We also want to thank Dr. Pilar López García, from the Microbiology Department, for assistance with the microbiological techniques and for her comments that greatly improved this manuscript.