Delayed haemolytic anaemia is one of the more frequent events after treatment with intravenous artesunate in patients with severe malaria. Little is known about its frequency and the outcomes of patients with this condition.
MethodsA retrospective study was conducted to describe the incidence of delayed haemolysis in a cohort of patients with severe malaria by Plasmodium falciparum treated with artesunate between August 2013 and July 2015.
ResultsThe study included 52 patients with malaria due to Plasmodium falciparum, with 21 having severe malaria. The majority were male (66.7%), and the median age was 43 years. Four patients (19%) presented post-artesunate delayed haemolysis 11–13 days from the initiation of treatment. Two patients required hospital admission and red blood cell transfusion.
ConclusionPost-artesunate delayed haemolysis is frequent in patients with severe malaria treated with intravenous artemisinins. These patients should be monitored for 4 weeks after treatment is started.
La anemia hemolítica diferida es uno de los acontecimientos más frecuentes tras el tratamiento con artesunato intravenoso en pacientes con malaria grave. Se desconocen con exactitud la frecuencia y evolución de los pacientes que la presentan.
MétodosEstudio retrospectivo sobre la incidencia de hemólisis diferida en una cohorte de pacientes con malaria grave por Plasmodium falciparum tratados con artesunato intravenoso entre agosto de 2013 y julio de 2015.
ResultadosDe 52 pacientes con malaria por Plasmodium falciparum, 21 cumplían criterios de gravedad. La mayoría eran hombres (66,7%) y la mediana de edad era de 43 años. Cuatro pacientes (19%) presentaron hemólisis diferida post-artesunato, de 11 a 13 días tras el inicio del tratamiento. Dos pacientes requirieron hospitalización y transfusión de hematíes.
ConclusiónLa hemólisis diferida post-artesunato es frecuente en los pacientes con malaria grave tratados con artesunato intravenoso. Estos pacientes deben ser monitorizados al menos 4 semanas tras el tratamiento.
Artesunate is currently the drug of choice for patients with severe malaria by Plasmodium falciparum.1 Although the main evidence of parenteral artesunate's superiority is supported by clinical trials performed in endemic settings,2,3 retrospective series in Europe suggest that it is more efficient than quinine.4 It provides a rapid parasite clearance, with a 90% decrease of the initial parasite burden in less than 24hours.5
Large clinical trials conducted in Southeast Asia and Africa failed to detect haemolytic anaemia as an artesunate-related event, partially due to the short follow-up period. However, in the last years, with the increasing use of artesunate for severe malaria, especially in non-endemic settings, cases of post-artesunate delayed haemolysis (PADH) have been reported.6 These patients presented a decrease of haemoglobin with haemolytic markers between 7 and 21 days after artesunate was initiated. Generally, these patients did not have other complications derived from haemolysis, although some needed hospital admission and red blood cell (RBC) transfusions.
We aim to describe the frequency of PADH in a cohort of patients with severe malaria, after treatment with artesunate.
MethodsRetrospective study including patients with severe malaria by Plasmodium falciparum treated with intravenous artesunate between August 2013 and July 2015 in Hospital Clínic, Barcelona. The main objective of the study was to evaluate the experience with artesunate therapy in patients with severe malaria, defined following the criteria of the Spanish Society of Tropical Medicine and International Health.7 This study has been approved by the Ethics Committee of Hospital Clínic.
In Hospital Clínic, patients with severe malaria are admitted at the Intensive Care Unit and, after stabilization, transferred to a ward. Treatment is currently done with intravenous artesunate 2.4mg/kg/day (0, 12 and 24hours and then every 24hours until parasite clearance), followed by a 3-day course of atovaquone/proguanil 1000/400mg. After discharge, follow-up is carried out in the outpatient clinic of Tropical Medicine Department.
As part of this study, the incidence of PADH was evaluated, defined as a haemoglobin decrease and the appearance or reappearance of haemolysis markers between 7 and 21 days after artesunate initiation. The descriptive statistics were performed with Stata 13.1 (Stata Corporation, Texas, USA). Categorical and continuous variables are described as counts and percentages and median and interquartilic range (IQR), respectively.
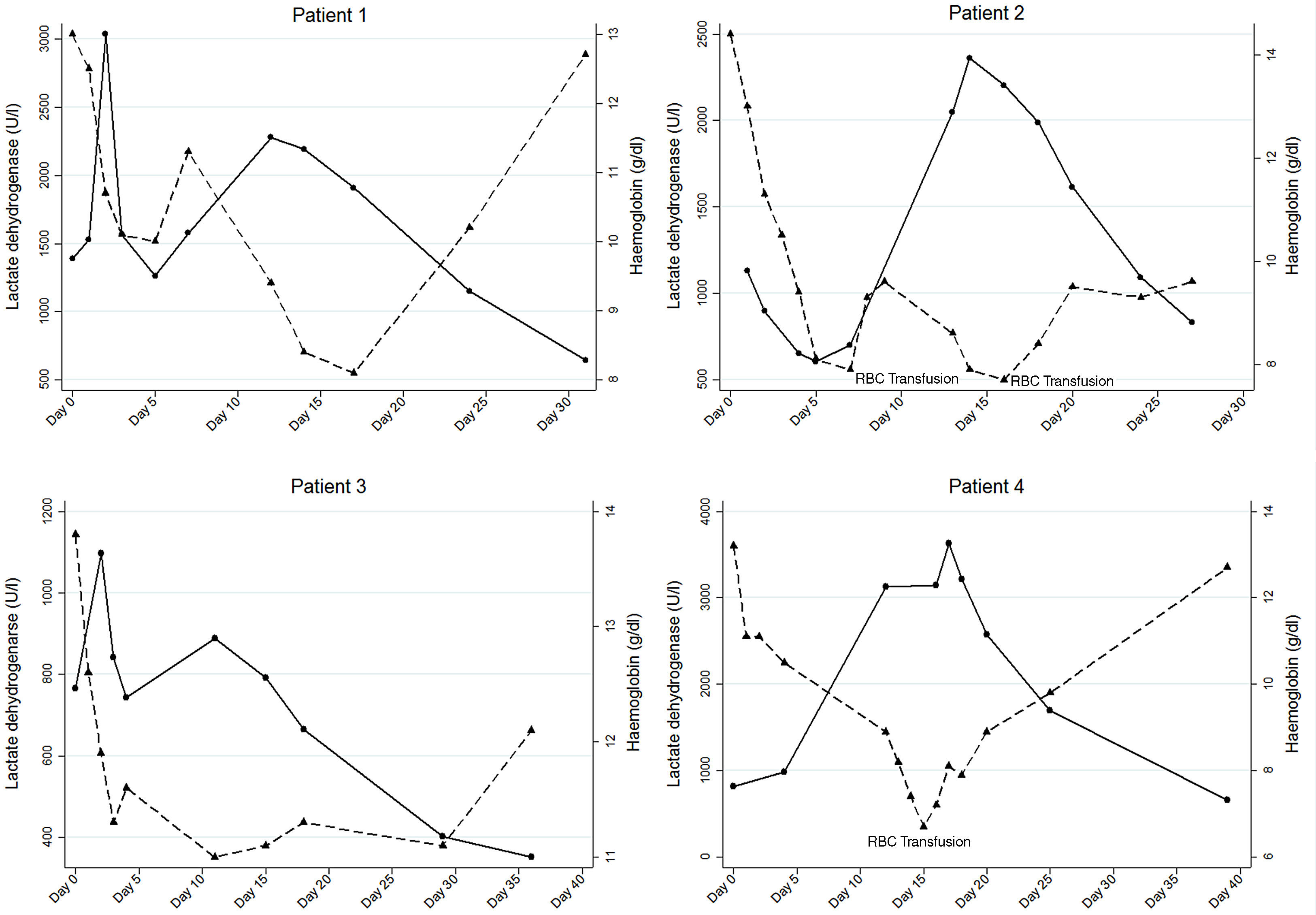
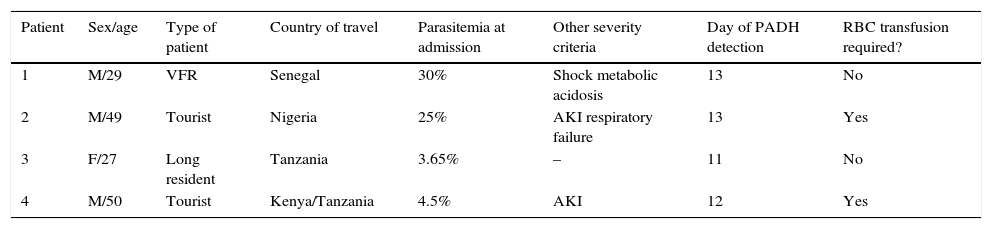
ResultsBetween August 2013 and July 2015, 52 patients had Plasmodium falciparum malaria, of which 21 (40.4%) had severe malaria. Median age was 43 years (IQR 33–50) and 66.7% were male. Four patients presented with PADH (19%). The main characteristics of these patients are summarized in Table 1. Fig. 1 illustrates the evolution of blood haemoglobin (normal values 12–17g/dl) and lactate dehydrogenase (normal values 250–450U/l) of these patients, after the first dose of artesunate.
Characteristics of 4 patients with Plasmodium falciparum severe malaria who presented post-artesunate delayed haemolysis.
| Patient | Sex/age | Type of patient | Country of travel | Parasitemia at admission | Other severity criteria | Day of PADH detection | RBC transfusion required? |
|---|---|---|---|---|---|---|---|
| 1 | M/29 | VFR | Senegal | 30% | Shock metabolic acidosis | 13 | No |
| 2 | M/49 | Tourist | Nigeria | 25% | AKI respiratory failure | 13 | Yes |
| 3 | F/27 | Long resident | Tanzania | 3.65% | – | 11 | No |
| 4 | M/50 | Tourist | Kenya/Tanzania | 4.5% | AKI | 12 | Yes |
Age is expressed in years. PADH: Post-artesunate delayed haemolysis; RBC: red blood cell; M: male; F: female; VFR: visiting friends and relatives; AKI: acute kidney injury.
A 29-year old male patient from Senegal, who had been living in Spain for 10 years, was admitted because of severe P. falciparum malaria. He had been in his country to visit friends and relatives for 3 weeks, without taking chemoprophylaxis. Upon admission, he had a parasitemia of 30%, shock, metabolic acidosis and prostration. He rapidly improved with artesunate, clearing parasitemia and being discharged without complications.
On day 13 post-artesunate, he was asymptomatic apart from mild asthenia, but his blood test showed haemoglobin 9.4g/dl and LDH 2279U/l (upon discharge on day 8, haemoglobin 11.3g/dl and LDH 1577U/l). Thus, PADH was suspected and the patient was closely monitored, but he did not require RBC transfusion, with full recovery of blood disorders (haemoglobin 12.7g/l and LDH 644U/l on day 31).
Patient 2A 49-year old male patient, who had travelled to Nigeria without chemoprophylaxis, was admitted for severe malaria by P. falciparum. He had an initial parasitemia of 25%, acute kidney injury (AKI) and respiratory failure. He was treated with artesunate and required RBC exchange, as his parasite count did not decrease more than 25% compared to baseline after 8hours since artesunate, according to the hospital's protocol. On day 7 post-artesunate, there was a reduction in haemoglobin without a substantial increase in LDH, which was attributed to malaria and the patient received RBC transfusion. The patient followed a correct clinical course and was discharged.
On day 13 post-artesunate, the patient presented with asthenia and mucocutaneous pallor. Blood tests showed a one-point decrease in haemoglobin (8.6g/dl) compared to discharge on day 9, with marked increase in LDH (2050U/l) and reticulocyte count. PADH was suspected and the patient was admitted for monitoring, requiring RBC transfusion for further haemoglobin decrease. The patient improved and haemoglobin progressively increased (9.6g/dl at last available check-up on day 27).
Patient 3A 27-year old female patient was admitted with severe P. falciparum malaria with initial parasitemia of 3.65%, as the only severity criteria. She was living in Tanzania for a year without chemoprophylaxis. She followed a mild course and could be discharged 4 days after treatment with artesunate.
On day 11, she was evaluated at the outpatient clinic and her blood tests showed a decrease of haemoglobin to 11g/dl from 11.6g/dl on day 4, with LDH increase from 744U/l on day 5 to 889U/l, apart from other haemolysis markers. PADH was then suspected. She was closely monitored without requiring RBC transfusion and haemoglobin and LDH normalized (12.1g/dl and 352U/l at last check-up on day 36, respectively).
Patient 4A 50-year old patient, who had travelled to Kenya and Tanzania without chemoprophylaxis, was admitted with severe malaria by P. falciparum. He had an initial parasitemia of 4.5% and AKI. He was successfully treated with artesunate, with complete parasite clearance and recovery of the renal function, being discharged on day 7 post-artesunate.
On day 12, he presented only asthenia and a haemoglobin reduction (8.9g/dl) and LDH increase (3130U/l) were found in his blood tests. The patient was admitted on suspicion of PADH and required RBC transfusion, as his haemoglobin dropped to 6.7g/dl. He then followed a good clinical course without further complications, with improvement of haemoglobin and LDH (12.7g/dl and 661U/l on day 39, respectively).
DiscussionDespite the small sample size, this study suggests that the incidence of PADH in patients with severe malaria is high. Although two patients needed hospital admission and RBC transfusion, none of them presented severe complications.
Although other authors have suggested PADH definitions which quantify the decrease of haemoglobin and the increase of LDH,8 we aimed to use a more sensible definition of PADH. Our definition may have prevented us from missing any case of PADH, therefore, providing an estimate of the maximum potential incidence of this event in our cohort.
In recent years, as artesunate is commonly administered for severe malaria, especially in travellers, PADH has been recognized as a frequent event in these patients.5,9 It has also been reported after oral artemisinin treatment in patients with severe malaria.10 A prospective study in France reported that 27% of those treated with intravenous artesunate presented PADH.11 However, only 3 of them, out of 21, had haemoglobin values below 7g/dl during follow-up.
PADH occurs after parasite clearance and usually 1–3 weeks after the initiation of artesunate, improving 1–3 weeks after. A high parasitaemia at admission has been identified as the main risk factor.12 The physiopathological mechanism is not clear and different hypotheses have been suggested. The main is based on the mechanism of action of artesunate, as parasites exposed to the drug are expelled from RBC in the spleen, a process known as pitting.13,14 Once-infected RBC are returned to systemic circulation, without parasite, but with a reduced lifespan.
Jauréguiberry et al. tested this hypothesis in a group of individuals with severe malaria treated with artesunate and evaluated the kinetics of once-infected RBC.15 They described that those with PADH had a higher concentration of once-infected RBC in the first week post-artesunate, compared to those without PADH. The number of once-infected RBC dropped 2–3 weeks after artesunate initiation, simultaneously with the greatest reduction of haemoglobin. These findings suggest that once-infected RBC are eliminated days or weeks after parasite clearance, contributing to PADH.
PADH is generally well tolerated, although some patients can present with severe anaemia and require RBC transfusion. There are no data about other treatments like steroids, although the probable non-immune mechanism make them unlikely to play a role. Currently, it is recommended that patients with severe malaria should be monitored during 4 weeks after treatment with intravenous artesunate, with weekly blood tests to detect PADH.7
In conclusion, this study suggests that PADH is frequent. This would be related probably to the therapeutic effect of parenteral artemisinins. Complications are rare and it is important to follow patients with severe malaria during 4 weeks after being treated with artesunate.
Conflict of interestsNone declared.