To determine the activity of fluoroquinolones (FQ) and the selection of FQ-resistant mutants in a macrophage experimental infection model (MEIM).
Material and methodsCanine macrophages were inoculated with Brucella melitensis ATCC 23457 (WT), achieving intracellular counts of around 105CFU/mL. Cell cultures were incubated in the presence of ciprofloxacin (CIP), levofloxacin (LEV), moxifloxacin (MOX), and doxycycline (DOX). After cell lysis, surviving microorganisms were plated for count purposes, and plated onto antibiotics-containing media for mutant selection. Topoisomerases mutations were detected by PCR and sequencing.
ResultsBacterial counts after cell lysis were 14.3% (CIP), 65.3% (LEV), and 75% (MOX) lower compared to the control. Quinolone-resistant mutants emerged in cell cultures containing CIP and LEV with a frequency of around 0.5×10−3. All mutants showed an Ala87Val change in GyrA. Mutants had FQs MICs around 10×WT. The ability of these mutants for infecting new macrophages and the intracellular lysis after antibiotic exposure did not change significantly. No 2nd step FQ-resistant mutants were selected from 1st step mutants.
ConclusionsIntracellular activity of FQs is low against WT and gyrA-mutant Brucella. FQs easily select gyrA mutants in MEIM. The ability of mutants for infecting new macrophages remains unchanged. In this MEIM, 2nd step mutants do not emerge.
Conocer la actividad de fluoroquinolonas (FQ) y la selección de mutantes resistentes (MR) a FQ en un modelo experimental de infección en macrófagos.
Material y métodosSe inocularon macrófagos de origen canino con la cepa tipo Brucella melitensis ATCC 23457 (CT) hasta alcanzar recuentos intracelulares de aproximadamente 105UFC/mL. Los cultivos celulares fueron incubados en presencia de ciprofloxacino, levofloxacino, moxifloxacino y doxiciclina. Una vez lisadas las células, los microorganismos supervivientes fueron sembrados en placas sin antibiótico para recuento, y en medios de cultivo conteniendo antimicrobianos para selección de MR. Los MR a topoisomerasas se caracterizaron mediante PCR y secuenciación.
ResultadosLos recuentos de microorganismos supervivientes tras el tratamiento con FQ y la lisis celular fueron: 14,3% ciprofloxacino, 65,3% levofloxacino y 75% moxifloxacino con respecto al control. Se seleccionaron MR a FQ en los cultivos celulares que contenían ciprofloxacino y levofloxacino, con una frecuencia en torno a 0,5×10−3. Todos los MR seleccionados portaban un cambio Ala87Val en gyrA, y mostraban CIM de FQ en torno a 10x la de la CT. La capacidad de estos MR para infectar nuevos macrófagos y su lisis intracelular tras tratamiento antibiótico no se modificaron de manera significativa con respecto a la CT. Usando la misma metodología, no se seleccionaron MR de segundo nivel a partir de los MR de primer nivel obtenidos.
ConclusionesLa actividad intracelular de FQ frente a Brucella es baja, tanto frente a la CT como frente a mutantes con cambios en gyrA. Las FQ seleccionan con facilidad mutantes con cambios en gyrA en este modelo experimental de infección en macrófagos. La capacidad de estos mutantes para infectar nuevos macrófagos permanece intacta. En este modelo experimental de infección en macrófagos no se observó la selección de mutantes de segundo nivel.
Brucellosis remains an important problem in many geographic areas, including the Mediterranean basin. Usually recommended treatments, such as doxycycline plus rifampicin or doxycycline plus streptomycin, are efficacious but they are not free of side effects and need to be administered for several weeks.1–4
When systemic fluoroquinolones (FQs) began to be available, they were considered a possible alternative for the treatment of brucellosis because of their activity against Gram-negative rods, good tissue levels and intracellular activity.5 Nevertheless, further clinical studies showed therapeutic failures and relapse rates of ca. 25% compared with <10% for conventional rifampicin or streptomycin plus doxycycline treatments.6
Some studies have suggested that these poor results might be associated with the reduced activity of FQs in an acidic environment. Brucellae are intracellular pathogens whose pathogenicity is mainly associated to their capacity to survive into cells, especially into phagolysosomes, where the acidic environment might impair FQ activity.7–9 Nevertheless, the involvement of topoisomerases mutations as a cause of FQ resistance has been seldom studied. The similarity between Brucella and Escherichia coli gyrA is only 70%, and the position equivalent to the serine 83 in E. coli is an alanine residue in Brucella. These differences between Brucella GyrA and the GyrA protein from other Gram negative bacteria more susceptible to FQs, such as enterobacteria, might explain the relatively high MIC (around 0.2–0.5mg/L) of CIP against wild-type Brucella. Studies on human pathogens harboring a GyrA protein similar to Brucella, such as Rickettsia and Bartonella, show MICs of CIP around 0.5–1mg/L, and MICs of 0.1–0.5mg/l for other generally more active FQs such as sparfloxacin.10,11
Turkmani et al.12 obtained recently FQ-resistant mutants in vitro from Brucella abortus and B. melitensis by growing them in the presence of antibiotics on antibiotic gradient plates. We also published recently the emergence of Ala71 to Ser gyrA mutants from B. melitensis ATCC 23457.13
The role of intracellular environment and FQ-resistant mutants emergence in Brucella survival has not been studied in macrophage infection models. We have studied intraphagocytic survival of Brucella in presence of extracellular inhibitory concentrations of FQs, FQ-resistant mutants selection under these conditions, and capacity of FQ-resistant mutants selected for newly infecting phagocytes and for surviving inside them.
Material and methodsThe strain used was B. melitensis biotype 2, strain 63/9 ATCC 23457. The microorganism was grown for 48h, on chocolate PolivitexR agar (bioMérieux, Le Balme Les Grottes, France), at 37°C in a 5% CO2 atmosphere.
The FQs tested were norfloxacin (NOR) (Merck, Sharp&Dohme, Whitehouse Station, NJ, USA), ciprofloxacin (CIP) (Bayer AG, Leverkusen, Germany), levofloxacin (LEV) (GlaxoSmithKline, Coraopolis, PA, USA) and moxifloxacin (MOX) (Bayer AG, Leverkusen, Germany), which were kindly provided by their respective manufacturers. MICs were determined by the agar-dilution method and by the E-test method, according CLSI (Clinical and Laboratory Standards Institute) general guidelines. The MICs of the antibiotics against B. melitensis ATCC 23457 were as follows: NOR, 1μg/mL; CIP, 0.25μg/mL; LEV, 0.12μg/mL; and MOX, 0.25μg/mL.
Doxycycline (DOX) (Pfizer, New York, USA) was kindly provided by the manufacturer. Gentamicin was purchased from Sigma–Aldrich (St. Louis, MO, USA).
Antibiotic susceptibility was determined following previously described methods12 and the general recommendations contained in the CLSI guidelines.14
Cell lines used were canine peritoneal macrophages (ATCC CRL-10389 DH82, Vircell, Granada, Spain). The cell culture medium used was Earle’ balanced salt solution (Sigma–Aldrich, St. Louis, MO, USA) with 15% fetal calf serum (Sigma–Aldrich, St. Louis, MO, USA) and glutamine 2mM (Sigma–Aldrich, St. Louis, MO, USA). The cell suspensions were placed in 25-cm2 tissue-culture flasks (Costar, Cambridge, MA, USA), and macrophages were allowed to adhere for 24h in a humidified CO2 5% incubator at 37°C. Non-adhering cells were then washed off. Adhering cells were washed three times with 3ml of complete medium. The adhering cells were then incubated in 3ml of complete medium for 2h. The number and viability of macrophages obtained by this procedure were determined by morphological examination and Trypan blue exclusion15.
B. melitensis biovar 2, ATCC 23457 from overnight cultures were opsonized at 37°C for 60min in ascitic fluid, previously sterilized by filtration (0.22 Sterivex-GP Millex-GV), containing a subagglutinating dilution (1 in 200 in complete RPMI 1640) of the mouse monoclonal antibody BmE 10-5 with specificity against the lipopolysaccharide (S-LPS) of Brucella spp.16 Bacterial suspensions were added to ascitic fluid and in the volume necessary for reaching the number of opsonized CFUs required. Opsonized bacteria were then centrifuged, washed and diluted in complete medium.
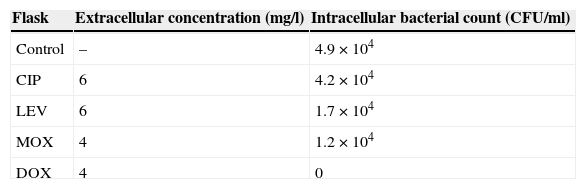
To infect macrophages, around 1×105CFU/mL of opsonized B. melitensis biovar 2, ATCC 23457 in complete medium was added (bacteria/macrophage rate was around 100:1), and incubated for 90min in a humidified CO2 5% incubator at 37°C, to allow opsonized bacteria penetration into the macrophages. Non-phagocytosed bacteria were washed off. Then, 3ml of complete medium containing gentamicin (100μg/mL) were added to the macrophages to kill any remaining extracellular bacteria.17 One flask was added only with gentamicin (control flask), while the remaining flasks were also added with CIP, LEV, MOX or DOX, at concentrations similar to serum concentrations reached at the usual dosage (6μg/mL of CIP and LEV, 4μg/mL of MOX and DOX).18
The macrophages were cultured for 2h at 37°C in a CO2 5% v/v incubator, and washed three times with complete medium. Complete medium from washing was then plated on chocolate PolivitexR agar to check the absence of extracellular microorganisms.
Cell cultures were then added with 5ml of 0.5% Tween 20 (Sigma–Aldrich, St. Louis, MO, USA) sterilized by filtration, and incubated for 30min at room temperature to lysate macrophages. The supernatant was collected, and 1ml of supernatant, and of 1:10 and 1:100 dilutions of it in complete medium, were plated onto chocolate PolivitexR agar plates in order to count colonies forming units (CFUs) obtained, which would reflect the number of intracellular B. melitensis in the cell culture.
1ml of supernatant, and of 1:10 and 1:100 dilutions of it in complete medium, were plated onto chocolate PolivitexR agar containing CIP, MOX and LEV at concentrations 4× their respective MICs for the ATCC 23457 strain, in order to detect hypothetical resistant mutants generated in the cell culture. MICs of the three FQs for the presumptive resistant mutants selected were checked by the agar dilution method. The mutant emergence rate was calculated and the quotient between the number of presumptive mutants detected on 4× MIC plates and the whole intracellular bacterial count in absence of FQs (bacterial count in control flask).
Then, the same mutants selection process was developed for obtaining 2nd step resistant mutants, using as infecting microorganisms the 1st step resistant mutants previously obtained. Chocolate PolivitexR agar plates inoculated for selecting 2nd step mutants contained CIP, LEV and MOX at 4× the 1st step mutants respective MICs.
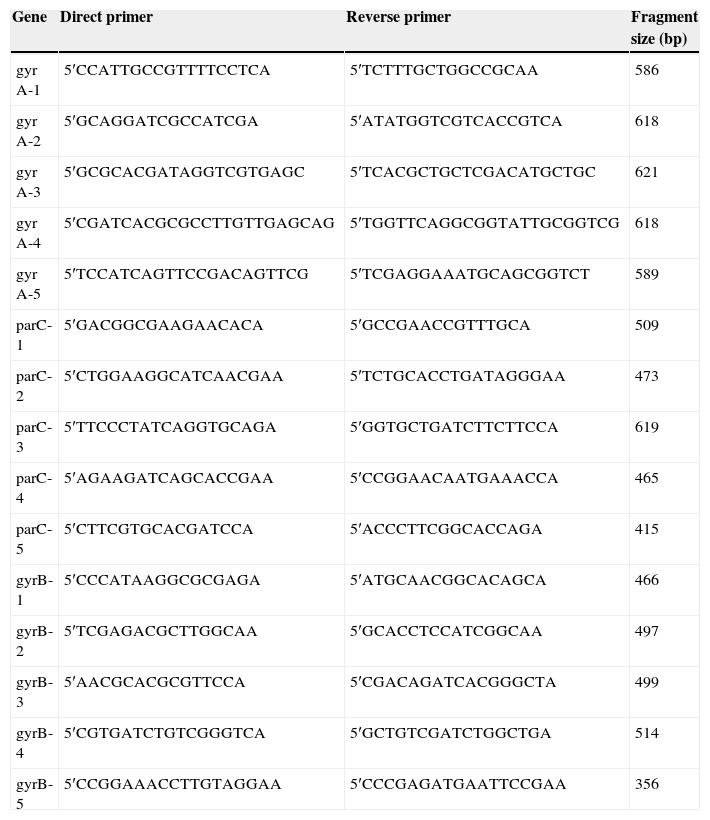
DNA was obtained from resistant mutants by conventional methods and purified using ExoSAP-IT (GE Healthcare, Piscataway, NJ, USA). Polymerase chain reaction (PCR) for the whole gyrA, gyrB and parC genes was performed in an Eppendorf Mastercycler® (Eppendorf AG, Hamburg, Germany) using PCR Master Mix (Promega Corp., Madison, WI, USA). The primers used are shown in Table 1. The primers were designed on the basis of gyrA, gyrB and parC sequences of B. melitensis biovar 3 strain NI, chromosome I (Accession No. CP002931). The amplification protocol used was as follows: initial denaturation at 94°C for 10min; 30 cycles of denaturation at 94°C for 1min, annealing for 1min at 48°C (parC-1, parC-3, parC-4 and parC-5), 50°C (gyrA-1, gyrA-2, parC-2), 53°C (gyrB-1, gyrB-2, gyrB-3, gyrB-5), 54°C (gyrB-4) and 62°C (gyrA-3, gyrA-4, gyrA-5), and extension at 72°C for 1min; followed by a final extension at 72°C for 3min.
Primers used for amplifying and sequencing topoisomerase Brucella genes.
| Gene | Direct primer | Reverse primer | Fragment size (bp) |
|---|---|---|---|
| gyr A-1 | 5′CCATTGCCGTTTTCCTCA | 5′TCTTTGCTGGCCGCAA | 586 |
| gyr A-2 | 5′GCAGGATCGCCATCGA | 5′ATATGGTCGTCACCGTCA | 618 |
| gyr A-3 | 5′GCGCACGATAGGTCGTGAGC | 5′TCACGCTGCTCGACATGCTGC | 621 |
| gyr A-4 | 5′CGATCACGCGCCTTGTTGAGCAG | 5′TGGTTCAGGCGGTATTGCGGTCG | 618 |
| gyr A-5 | 5′TCCATCAGTTCCGACAGTTCG | 5′TCGAGGAAATGCAGCGGTCT | 589 |
| parC-1 | 5′GACGGCGAAGAACACA | 5′GCCGAACCGTTTGCA | 509 |
| parC-2 | 5′CTGGAAGGCATCAACGAA | 5′TCTGCACCTGATAGGGAA | 473 |
| parC-3 | 5′TTCCCTATCAGGTGCAGA | 5′GGTGCTGATCTTCTTCCA | 619 |
| parC-4 | 5′AGAAGATCAGCACCGAA | 5′CCGGAACAATGAAACCA | 465 |
| parC-5 | 5′CTTCGTGCACGATCCA | 5′ACCCTTCGGCACCAGA | 415 |
| gyrB-1 | 5′CCCATAAGGCGCGAGA | 5′ATGCAACGGCACAGCA | 466 |
| gyrB-2 | 5′TCGAGACGCTTGGCAA | 5′GCACCTCCATCGGCAA | 497 |
| gyrB-3 | 5′AACGCACGCGTTCCA | 5′CGACAGATCACGGGCTA | 499 |
| gyrB-4 | 5′CGTGATCTGTCGGGTCA | 5′GCTGTCGATCTGGCTGA | 514 |
| gyrB-5 | 5′CCGGAAACCTTGTAGGAA | 5′CCCGAGATGAATTCCGAA | 356 |
Amplified products were purified with ExoSAP-IT and sequenced. Sequences were aligned and compared with gyrA, gyrB and parC sequences of B. melitensis biovar 3 strain NI, chromosome I using BLAST software (National Center for Biotechnology Information, Bethesda, MD, USA).
ResultsIntracellular counts of Brucella in absence of FQs and after FQs or DOX addition appear in Table 2. These results show that, after 2h of incubation with CIP, intracellular bacterial count was similar to the control. LEV and MOX reduce the original bacterial count to 1/3–1/4, while DOX eradicated the whole intracellular bacterial population.
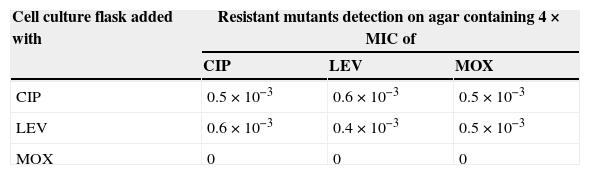
When FQ-resistant mutants emergence was determined among the intraphagocytic surviving populations, mutants were detected in the flaks treated with CIP and LEV, as appears in Table 3, while no mutants were obtained from the flask containing MOX, and from the flask that had been added only with gentamicin. FQ-resistant mutants selection rate with CIP and LEV was high, around 0.5×10−3 in all the cases when mutants were found.
FQ-resistant mutants obtained from B. melitensis ATCC23457 on chocolate agar plates added with FQs at 4×MIC concentrations.
| Cell culture flask added with | Resistant mutants detection on agar containing 4×MIC of | ||
|---|---|---|---|
| CIP | LEV | MOX | |
| CIP | 0.5×10−3 | 0.6×10−3 | 0.5×10−3 |
| LEV | 0.6×10−3 | 0.4×10−3 | 0.5×10−3 |
| MOX | 0 | 0 | 0 |
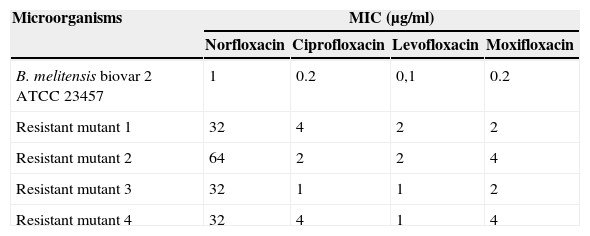
Three to five colonies were picked from each plate for susceptibility and molecular study. Four susceptibility profiles were found, though MICs were similar for all mutants selected (Table 4), and further molecular analysis showed that all of them harbored the same topoisomerases mutations.
MIC (μg/mL) of FQs for B. melitensis ATCC 23457 and for mutants obtained.
| Microorganisms | MIC (μg/ml) | |||
|---|---|---|---|---|
| Norfloxacin | Ciprofloxacin | Levofloxacin | Moxifloxacin | |
| B. melitensis biovar 2 ATCC 23457 | 1 | 0.2 | 0,1 | 0.2 |
| Resistant mutant 1 | 32 | 4 | 2 | 2 |
| Resistant mutant 2 | 64 | 2 | 2 | 4 |
| Resistant mutant 3 | 32 | 1 | 1 | 2 |
| Resistant mutant 4 | 32 | 4 | 1 | 4 |
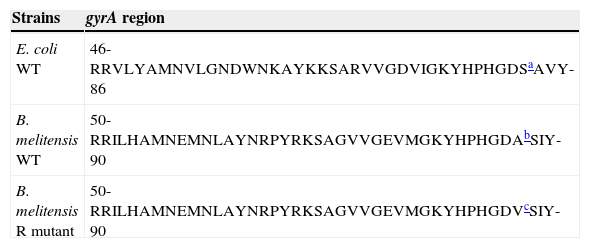
All the resistant mutants obtained in macrophage cultures had a C to T mutation in the position 260 of gyrA gene, leading to a Ala (GCT) 87 to Val (GTT) change. Position 87 of GyrA from B. melitensis corresponds to position 83 of GyrA from E. coli (Accession No. X06373). This position corresponds to a Ser residue in wild-type E. coli gyrase subunit A, and is the main mutation point in topoisomerase-resistant E. coli (Table 5).
gyrA mutations observed in intracellular FQ-resistant mutants obtained from B. melitensis ATCC 23457.
No significant changes were observed in gyrB and parC genes, as compared to wild-type strain.
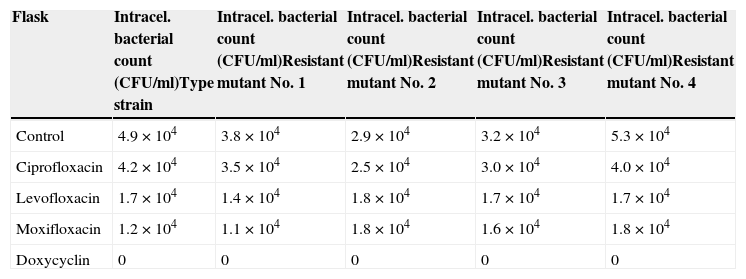
Results obtained when the experiment of macrophage penetration was repeated using mutants obtained, instead of wild-type B. melitensis ATCC 2457, appear in Table 6.
Intracellular counts of FQ-resistant mutant B. melitensis obtained in the control flask and in the flask added with FQs and DOX.
| Flask | Intracel. bacterial count (CFU/ml)Type strain | Intracel. bacterial count (CFU/ml)Resistant mutant No. 1 | Intracel. bacterial count (CFU/ml)Resistant mutant No. 2 | Intracel. bacterial count (CFU/ml)Resistant mutant No. 3 | Intracel. bacterial count (CFU/ml)Resistant mutant No. 4 |
|---|---|---|---|---|---|
| Control | 4.9×104 | 3.8×104 | 2.9×104 | 3.2×104 | 5.3×104 |
| Ciprofloxacin | 4.2×104 | 3.5×104 | 2.5×104 | 3.0×104 | 4.0×104 |
| Levofloxacin | 1.7×104 | 1.4×104 | 1.8×104 | 1.7×104 | 1.7×104 |
| Moxifloxacin | 1.2×104 | 1.1×104 | 1.8×104 | 1.6×104 | 1.8×104 |
| Doxycyclin | 0 | 0 | 0 | 0 | 0 |
No differences were observed in comparison to the behavior of the wild-type strain. Intracellular bacterial count, in absence of antibiotics, ranged from 2.8×104 to 5.3×104CFU/mL; thus, the capacity of FQ-resistant mutants to penetrate into the phagocytes seems to remain unchanged. CIP led to very modest bacterial count reductions, while LEV and MOX reduced bacterial count to 1/3–1/4, and DOX cleared all the intraphagocytic microorganisms, as also happened when type strain was used.
When emergence of resistant mutants was determined among the intraphagocytic surviving populations, no 2nd step mutants were detected in any flask.
DiscussionResults obtained in the first experiment suggest that antibacterial activity of FQs against intraphagocytic Brucellae is moderate to low, much lower than DOX. Bacterial counts hardly decreased when cell cultures are treated with CIP, and decrease to 1/3–1/4 with LEV and MOX, while DOX eradicated all the intracellular Brucellae. That may explain the failures of FQs in the treatment of brucellosis, independently of the emergence of resistant mutants. This behavior may be due to the low pH, as has been suggested previously,7–9 or might be associated to more complex factors. One important factor is probably the fact that Brucella, as happens to other microorganisms with GyrA proteins harboring significant differences with respect to conventional GyrA proteins found in enterobacteria,10,11 have a lower susceptibility to FQs. This way, B. melitensis ATCC 23457 has MICs of CIP, LEV and MOX of 0.1–0.2mg/L, while expected MIC ranges of CIP and LEV against E. coli ATCC 25922 are 0.004–0.015mg/L and 0.008–0.06mg/L, respectively.14 Otherwise, this behavior enables one only 1st step gyrA mutation to be enough to get full resistance, as happens in this study if we consider the break points accepted for most Gram negative bacteria.
Moreover, the contact between B. melitensis and FQs inside the macrophage generates, at a high selection rate (around 0.5×10−3), FQ-resistant mutants harboring gyrA mutations. The mutant selection rate was similar for CIP and LEV, and the gyrA mutation found was also the same. MOX did not select any mutant, but mutants selected by CIP and LEV were also MOX-resistant, MOX MIC increasing, as compared to wild-type strain, in a proportion similar to LEV and CIP (8–16 fold). We do not have a convincing explanation for the lack of mutants emergence in the presence of MOX. It does not seem to be associated to a higher intracellular activity, since bacterial count reduction in presence of MOX and LEV are similar. Otherwise, Ala-87-Val mutants selected in the presence of CIP or LEV increase their MIC of MOX in a similar way as they increase CIP and LEV MICs (8–16×). Thus, should these mutants emerge in the presence of MOX, it should have been detected. We can consider two possibilities: mutant emergence rate may be much lower in the presence of MOX than in the presence of CIP or LEV. This macrophage infection model may not be sensitive enough for low mutants emergence rates. Otherwise, MOX might select for other type of mutants with a more modest MIC increase, which might have been overlooked with the method used. Anyway, conventional in vitro selection studies with MOX might contribute to clarify this aspect.
The mutant selection rate is high in comparison to other microorganisms, and to other studies on Brucella. Previous studies13 show that, in conventional mutant selection experiments, 1st step FQ-resistant mutant selection rate would be around 1×10−6, while in this study the frequency is around 0.5×10−3. The different selection rates might be associated to the methods of study. In conventional mutant selection experiments, mutants spontaneously emerging in a broth culture are selected by plating a broth aliquot on culture plates added with a selecting antibiotic at concentrations higher than the MIC of the original strain. In this experiment, the original strain underwent intracellular contact with different FQs for 2hours, before being plated on antibiotic culture plates. This previous contact probably may promote resistant mutant generation, leading to a higher FQ-resistant mutant selection rate. Otherwise, in previous studies13 the selecting FQ used was norfloxacin, instead of CIP, LEV and MOX; thus, the results might not be exactly comparable.
There was no FQ-resistant mutants selection from the MOX-containing flasks. This result may probably be a bias associated to the number of Brucella CFUs inoculated in cell cultures. Since proportions Brucella/macrophages higher than 100:1 could not be used, because this damaged the cell culture, the inoculum had to be lower than that in conventional mutant selection experiments, and mutant selection rates lower than 5×10−4 may have remained undetected.
Though MICs of FQs for the mutants obtained were not identical, differences were small, and quinolone resistance-associated mutations found were the same for all the QR mutants selected. The Ala87Val mutation has been previously described by Turkmani et al.12 These authors describe the selection in vitro of four FQ-resistant mutants, harboring mutations leading to Asp91Tyr, Asp91Asn and Ala87Val substitutions in GyrA. Asp91 corresponds to Asp87 in E. coli, the second most frequent gyrA hot point for mutations in FQ-resistant E. coli, after Ser83. Asp87 would correspond to Ser83 in E. coli, the most frequently mutated position found in this species.19
Other studies have found different FQ resistance-associated mutations, such as GyrA Ala71Ser, corresponding to Ala67 in E. coli, and GyrA Ala340 insertion.13
When these mutants were used as the initial inoculum for infecting macrophages, both the intracellular microorganisms count in the control flask and the microorganisms count after FQs addition were similar to the first experiment, suggesting that the capacity of FQ-resistant mutant for infecting macrophages, and for surviving inside them in the presence of FQs, are not significantly modified in comparison to wild-type strain.
In this study, no further FQ-resistant mutants were obtained when macrophages were infected with the 1st step mutant. Previous studies have shown that further 2nd and 3rd step FQ-resistant mutants can be selected in Brucella. These mutants showed higher MICs of norfloxacin and CIP the most hydrophilic FQs tested, but did not show any further mutation in gyrA, gyrB or parC genes, suggesting a role for efflux pumps in this resistance. These mutants were obtained at a low selection rate (8×10−7 and 3×10−8, respectively); thus, the lower inoculum allowed for the study on macrophage cultures may have prevented the selection of these further mutants.
Conflict of interestThe authors declare no conflict of interest.
FundingThis study has been financed by a grant from the Plan Regional de Investigación, Junta de Castilla y León, Spain (Grant HUS-4-04).
We gratefully acknowledge Dr. Nieves Vizcaino for providing us with the BmE 10-5 antibody against Brucella lipopolysaccharide.