Population movements during the last few decades have resulted in a progressively increasing interest in certain infectious diseases. Eosinophilia is a common finding in immigrants and travellers. One of the most common causes of eosinophilia is helminth infection, and some intestinal protozoa.
The aim of this paper is to describe the epidemiological characteristics of cases with eosinophilia and its association with the presence of parasites in the REDIVI data network.
This is a multicentre prospective observational study that includes patients diagnosed with eosinophilia registered in the cooperative network for the study of infectious diseases imported by travellers and immigrants (+REDIVI) from January 2009 to December 2012.
A total of 5255 episodes were registered in the network during the study period, and eosinophilia was observed in 8.1–31.3% of cases (depending on the immigration group). Some 60.2% were male, with a median age of 31.0 years, 72.4% were immigrants and 81.2% were asymptomatic. The most commonly identified parasites were S. stercoralis (34.4%), Schistosoma sp. (11.0%), and hookworm (8.6%). The relationship between eosinophilia and parasite infection was significant for all helminths (except for cutaneous larva migrans). The symptoms and duration of the journey did not significantly determine the presence of eosinophilia.
In the case of eosinophilia in a person who has lived in helminth endemic areas, it is advisable to carry out targeted studies to diagnose the infection, regardless of immigration type, length of stay, or the presence of symptoms.
Algunas enfermedades infecciosas han adquirido más relevancia por el aumento de los movimientos poblacionales. La eosinofilia es un hallazgo frecuente en inmigrantes y en viajeros. Una de las causas más frecuentes de eosinofilia es la infección por helmintos y algunos protozoos intestinales.
El objetivo de este trabajo es describir las características epidemiológicas de los casos con eosinofilia y su asociación con la presencia de parásitos en la red de datos REDIVI.
Se trata de un estudio observacional multicéntrico prospectivo, donde se incluyen los casos diagnosticados de eosinofilia registrados en la Red cooperativa para el estudio de las infecciones importadas por viajeros e inmigrantes (+REDIVI) desde enero de 2009 hasta diciembre de 2012.
Se registraron en la red un total de 5.255 episodios durante el periodo de estudio, y la eosinofilia fue un hallazgo en el 8,1 al 31,3% de los casos (dependiendo del tipo migratorio). Fueron hombres el 60,2%, con una mediana de 31,0años, inmigrantes el 72,4% y asintomáticos el 81,2%. Los parásitos más frecuentemente identificados fueron S.stercoralis (34,4%), Schistosoma sp. (11,0%) y uncinarias (8,6%). Existía asociación entre eosinofilia y presencia de parásitos para todos los helmintos (excepto para larva migrans cutánea). La sintomatología y la duración del viaje no determinaron significativamente la presencia de eosinofilia.
Ante una eosinofilia en una persona que ha vivido en zonas endémicas de helmintiasis es aconsejable realizar estudios dirigidos para su diagnóstico, independientemente del tipo migratorio, la duración de la estancia o la presencia de sintomatología.
In recent years, certain infectious diseases have gained more relevance because of the increase in population movements. According to data from the National Institute of Statistics of Spain, during the first quarter of 2015, there were 2,758,000 trips abroad by Spaniards, with 46% for tourism, 27% for visiting family members and 23% for work or business.1 In addition, impoverished financial conditions or war in certain countries lead to a global increase in migratory movements towards more fortunate countries. The Spanish national survey on immigration estimated that in 2013 a total of 5,118,112 people living in Spain (11% of the population) were born abroad.2
The eosinophil counts that define eosinophilia can vary from one study to another, but are normally ≥450–600 eosinophils/mm3.3–5 A high eosinophil count is a common finding in immigrants; from 12% to 27% depending on the publication.5–8 In travellers, the prevalence of eosinophilia is somewhat lower, ranging from 5% to 9%.9,10 One of the most common causes of eosinophilia, particularly in the immigrant population, is helminth infection and infection from certain intestinal protozoa (Dientamoeba fragilis and Cystoisospora belli).4
Helminths are parasites which are prevalent throughout the world, but they particularly affect the impoverished areas of the planet, especially in the tropics. The most common are the geohelminths: Ascaris lumbricoides, Trichuris trichiura and hookworms (Ancylostoma duodenale and Necator americanus). People infected by these helminths often remain asymptomatic. However, in children, infection can affect growth and cognitive development.11 Strongyloidiasis is another important helminthiasis that can persist for years in the host because of its capacity for autoinfection and multiplication. Although it does not normally cause symptoms, it can become life-threatening in the case of hyperinfestation in immunosuppressed patients.12 Another serious helminthiasis is schistosomiasis. Untreated, urinary schistosomiasis can lead to the development of squamous cell carcinoma and intestinal schistosomiasis, to hepatosplenomegaly and portal hypertension.11 Yet another significant helminth infection is filariasis, although its prevalence seems to have decreased since the introduction of mass treatment programmes.13
The aim of this paper is to describe the epidemiological characteristics of cases with eosinophilia and its association with the presence of parasites in the REDIVI data network.
Material and methodsThis is a multicentre prospective observational study which includes patients diagnosed with eosinophilia registered in the cooperative network for the study of infectious diseases imported by travellers and immigrants (+REDIVI) from January 2009 to December 2012. This network collects data in a number of Spanish centres that enables us to identify and quantify the imported conditions, their geographical origin, the type of patient affected and the temporal patterns involved. These data cannot be linked to an individual because they are coded and each centre can only decrypt the information from the database for its own cases. The network was set up in January 2009 and is coordinated from Hospital Ramón y Cajal. In December 2012, it had 17 participating centres.
The variables to be studied were: gender, date of birth, country of birth, type of migration, country of origin/destination, date of arrival from the migration/travel process, duration of the trip, date of visit, reason for consultation and diagnosis. These data are mandatory for registration in the database, in addition to data on the clinical, epidemiological and disease process, according to a standardised protocol. Four forms of population movement were considered: immigrants; immigrants established in Spain visiting their country of birth (VFR: visiting friends and relatives); travellers; and VFR-travellers (children or spouses of immigrants born in Spain travelling to the country of their parents/partners). The definition of eosinophilia was that used at each of the participating centres to establish the diagnosis. This was because there is no standard definition for eosinophilia, and the range of parameters considered normal may vary from one centre to another. In addition, the reference figures used in Spanish hospitals do not conform to the biological parameters of certain populations (e.g. Sub-Saharan Africans). In general, the most commonly used figures were an absolute eosinophil count greater than 500/mm3 or, in relative terms, greater than 7%.
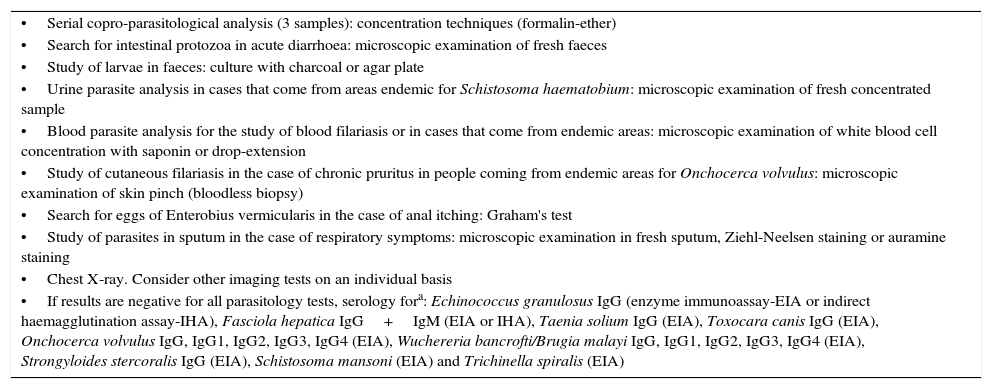
The parasites responsible for eosinophilia were considered to be helminths and the protozoa D. fragilis and C. belli. The most commonly used protocol for the study of eosinophilia is shown in Table 1. Microscopic or serological techniques may vary from one centre to another depending on the available resources and the experience of each laboratory.
Protocol for the study of parasitic eosinophilia.
| •Serial copro-parasitological analysis (3 samples): concentration techniques (formalin-ether) |
| •Search for intestinal protozoa in acute diarrhoea: microscopic examination of fresh faeces |
| •Study of larvae in faeces: culture with charcoal or agar plate |
| •Urine parasite analysis in cases that come from areas endemic for Schistosoma haematobium: microscopic examination of fresh concentrated sample |
| •Blood parasite analysis for the study of blood filariasis or in cases that come from endemic areas: microscopic examination of white blood cell concentration with saponin or drop-extension |
| •Study of cutaneous filariasis in the case of chronic pruritus in people coming from endemic areas for Onchocerca volvulus: microscopic examination of skin pinch (bloodless biopsy) |
| •Search for eggs of Enterobius vermicularis in the case of anal itching: Graham's test |
| •Study of parasites in sputum in the case of respiratory symptoms: microscopic examination in fresh sputum, Ziehl-Neelsen staining or auramine staining |
| •Chest X-ray. Consider other imaging tests on an individual basis |
| •If results are negative for all parasitology tests, serology fora: Echinococcus granulosus IgG (enzyme immunoassay-EIA or indirect haemagglutination assay-IHA), Fasciola hepatica IgG+IgM (EIA or IHA), Taenia solium IgG (EIA), Toxocara canis IgG (EIA), Onchocerca volvulus IgG, IgG1, IgG2, IgG3, IgG4 (EIA), Wuchereria bancrofti/Brugia malayi IgG, IgG1, IgG2, IgG3, IgG4 (EIA), Strongyloides stercoralis IgG (EIA), Schistosoma mansoni (EIA) and Trichinella spiralis (EIA) |
The study was approved by the ethics committee (IEC) of the Hospital Vall d’Hebron in Barcelona and was managed according to good clinical practice guidelines.
For the description of the data we used distribution measures, central tendency (mean or median if the standard deviation was >20%) and dispersion (standard deviation and interquartile range). Qualitative variables were compared using the chi-square test or Fisher's exact test for small samples. The risk analysis was calculated with prevalence ratios and their 95% confidence interval. Student's t test was used to compare continuous variables. SPSS version 21.00® software was used to conduct the statistical analysis.
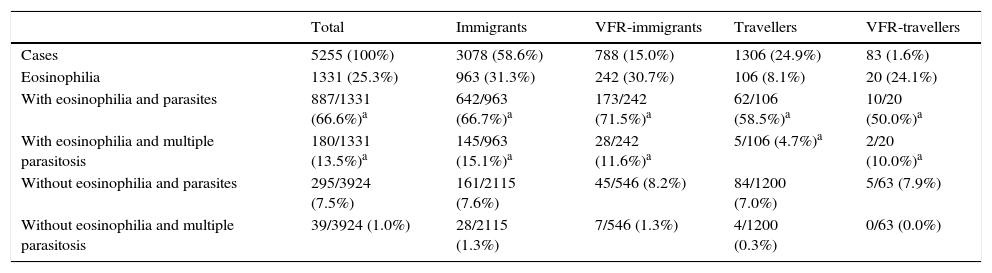
ResultsA total of 5255 cases were registered in the REDIVI network during the study period, and eosinophilia was an analytical finding in 1331 (25.3%).
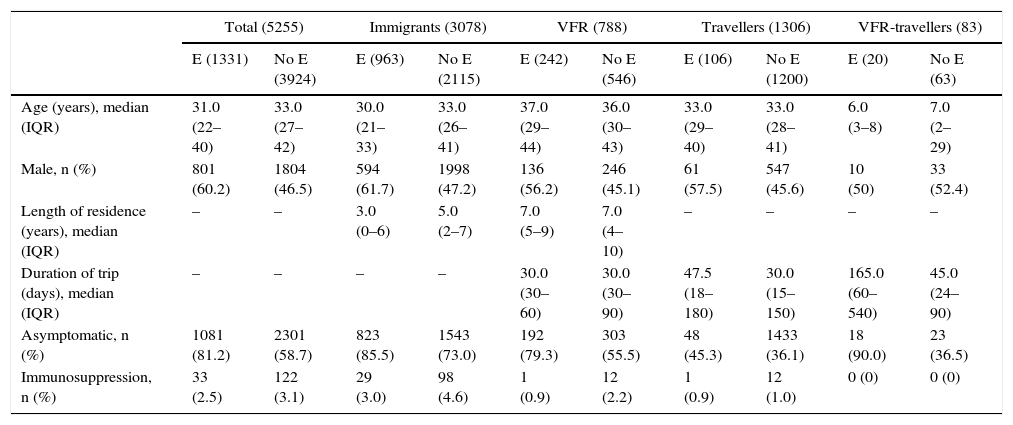
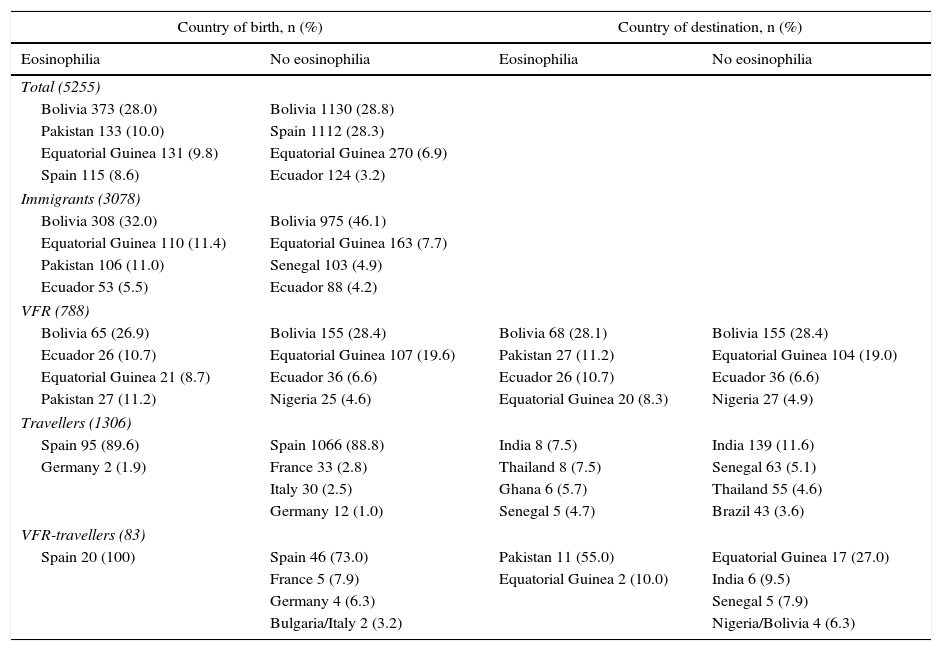
Of the 1331 cases with eosinophilia, 801 were male (60.2%), with a median age of 31.0 years (IQR: 22.0–40.0), 963 were immigrants (72.4%) and 1081 asymptomatic (81.2%). Immunosuppression was found in 33 (2.5%); as a consequence of HIV in 30 (90.9%), drugs in one (3.0%) and for other reasons in two (6.1%) (Tables 2 and 3). They had been born in the following geographical areas: America (589; 44.3%); Africa (375; 28.2%); Asia (238; 17.9%); and Europe (129; 9.7%). The most common countries of birth were: Bolivia (373; 28.0%); Pakistan (133; 10.0%); Equatorial Guinea (131; 9.8%); and Spain (115; 8.6%) (Table 4).
Eosinophilia distribution according to the type of migration.
| Total | Immigrants | VFR-immigrants | Travellers | VFR-travellers | |
|---|---|---|---|---|---|
| Cases | 5255 (100%) | 3078 (58.6%) | 788 (15.0%) | 1306 (24.9%) | 83 (1.6%) |
| Eosinophilia | 1331 (25.3%) | 963 (31.3%) | 242 (30.7%) | 106 (8.1%) | 20 (24.1%) |
| With eosinophilia and parasites | 887/1331 (66.6%)a | 642/963 (66.7%)a | 173/242 (71.5%)a | 62/106 (58.5%)a | 10/20 (50.0%)a |
| With eosinophilia and multiple parasitosis | 180/1331 (13.5%)a | 145/963 (15.1%)a | 28/242 (11.6%)a | 5/106 (4.7%)a | 2/20 (10.0%)a |
| Without eosinophilia and parasites | 295/3924 (7.5%) | 161/2115 (7.6%) | 45/546 (8.2%) | 84/1200 (7.0%) | 5/63 (7.9%) |
| Without eosinophilia and multiple parasitosis | 39/3924 (1.0%) | 28/2115 (1.3%) | 7/546 (1.3%) | 4/1200 (0.3%) | 0/63 (0.0%) |
VFR: immigrants established in Spain who visit their country of birth; VFR-travellers: children or spouses of immigrants, born in Spain, who travel to the country of their parents/partners.
Comparison of epidemiological and clinical characteristics according to the presence of eosinophilia.
| Total (5255) | Immigrants (3078) | VFR (788) | Travellers (1306) | VFR-travellers (83) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| E (1331) | No E (3924) | E (963) | No E (2115) | E (242) | No E (546) | E (106) | No E (1200) | E (20) | No E (63) | |
| Age (years), median (IQR) | 31.0 (22–40) | 33.0 (27–42) | 30.0 (21–33) | 33.0 (26–41) | 37.0 (29–44) | 36.0 (30–43) | 33.0 (29–40) | 33.0 (28–41) | 6.0 (3–8) | 7.0 (2–29) |
| Male, n (%) | 801 (60.2) | 1804 (46.5) | 594 (61.7) | 1998 (47.2) | 136 (56.2) | 246 (45.1) | 61 (57.5) | 547 (45.6) | 10 (50) | 33 (52.4) |
| Length of residence (years), median (IQR) | – | – | 3.0 (0–6) | 5.0 (2–7) | 7.0 (5–9) | 7.0 (4–10) | – | – | – | – |
| Duration of trip (days), median (IQR) | – | – | – | – | 30.0 (30–60) | 30.0 (30–90) | 47.5 (18–180) | 30.0 (15–150) | 165.0 (60–540) | 45.0 (24–90) |
| Asymptomatic, n (%) | 1081 (81.2) | 2301 (58.7) | 823 (85.5) | 1543 (73.0) | 192 (79.3) | 303 (55.5) | 48 (45.3) | 1433 (36.1) | 18 (90.0) | 23 (36.5) |
| Immunosuppression, n (%) | 33 (2.5) | 122 (3.1) | 29 (3.0) | 98 (4.6) | 1 (0.9) | 12 (2.2) | 1 (0.9) | 12 (1.0) | 0 (0) | 0 (0) |
E: eosinophilia; VFR: immigrants established in Spain who visit their country of birth; VFR-travellers: children or spouses of immigrants, born in Spain, who travel to the country of their parents/partners.
Most common countries of birth and origin of the cases according to the presence of eosinophilia.
| Country of birth, n (%) | Country of destination, n (%) | ||
|---|---|---|---|
| Eosinophilia | No eosinophilia | Eosinophilia | No eosinophilia |
| Total (5255) | |||
| Bolivia 373 (28.0) | Bolivia 1130 (28.8) | ||
| Pakistan 133 (10.0) | Spain 1112 (28.3) | ||
| Equatorial Guinea 131 (9.8) | Equatorial Guinea 270 (6.9) | ||
| Spain 115 (8.6) | Ecuador 124 (3.2) | ||
| Immigrants (3078) | |||
| Bolivia 308 (32.0) | Bolivia 975 (46.1) | ||
| Equatorial Guinea 110 (11.4) | Equatorial Guinea 163 (7.7) | ||
| Pakistan 106 (11.0) | Senegal 103 (4.9) | ||
| Ecuador 53 (5.5) | Ecuador 88 (4.2) | ||
| VFR (788) | |||
| Bolivia 65 (26.9) | Bolivia 155 (28.4) | Bolivia 68 (28.1) | Bolivia 155 (28.4) |
| Ecuador 26 (10.7) | Equatorial Guinea 107 (19.6) | Pakistan 27 (11.2) | Equatorial Guinea 104 (19.0) |
| Equatorial Guinea 21 (8.7) | Ecuador 36 (6.6) | Ecuador 26 (10.7) | Ecuador 36 (6.6) |
| Pakistan 27 (11.2) | Nigeria 25 (4.6) | Equatorial Guinea 20 (8.3) | Nigeria 27 (4.9) |
| Travellers (1306) | |||
| Spain 95 (89.6) | Spain 1066 (88.8) | India 8 (7.5) | India 139 (11.6) |
| Germany 2 (1.9) | France 33 (2.8) | Thailand 8 (7.5) | Senegal 63 (5.1) |
| Italy 30 (2.5) | Ghana 6 (5.7) | Thailand 55 (4.6) | |
| Germany 12 (1.0) | Senegal 5 (4.7) | Brazil 43 (3.6) | |
| VFR-travellers (83) | |||
| Spain 20 (100) | Spain 46 (73.0) | Pakistan 11 (55.0) | Equatorial Guinea 17 (27.0) |
| France 5 (7.9) | Equatorial Guinea 2 (10.0) | India 6 (9.5) | |
| Germany 4 (6.3) | Senegal 5 (7.9) | ||
| Bulgaria/Italy 2 (3.2) | Nigeria/Bolivia 4 (6.3) | ||
VFR: immigrants established in Spain who visit their country of birth; VFR-travellers: children or spouses of immigrants, born in Spain, who travel to the country of their parents/partners.
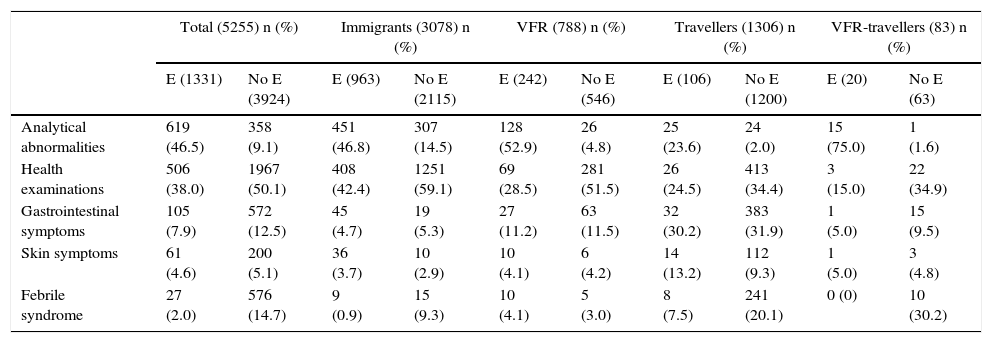
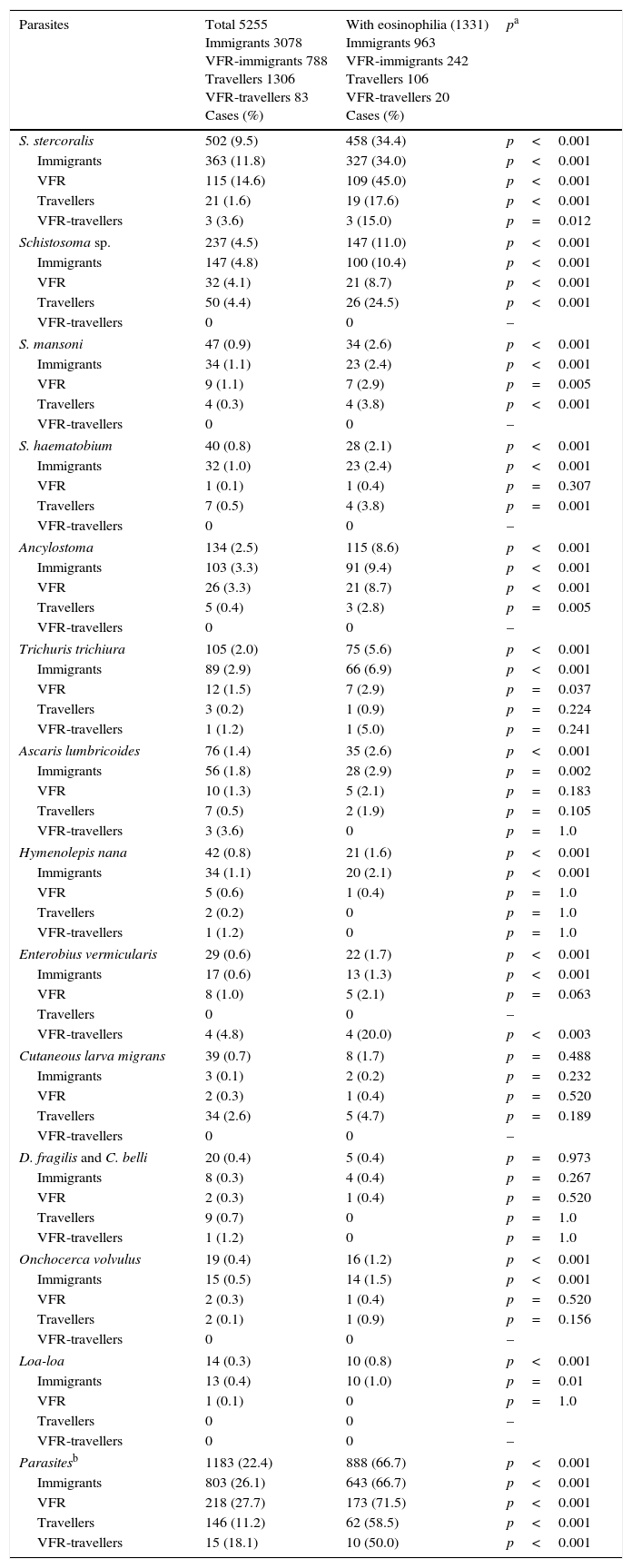
The majority of patients with eosinophilia had no symptoms (1081; 81.2%) and gave more than one reason for consulting (66; 5.0%). The most common reasons for consulting were: analytical abnormalities (619; 46.5%); health examination (506; 38.0%); gastrointestinal symptoms (105; 7.9%); skin symptoms (61; 4.6%); and febrile syndrome (27; 2.0%) (Table 5). Parasitic disease was diagnosed in 887 (66.6%) and infection by more than one parasite in 180 (13.5%). The most commonly identified parasites were: S. stercoralis (458; 34.4%); Schistosoma sp. (147; 11.0%); hookworm (115; 8.6%); visceral larva migrans (94; 7.1%), T. trichiura (75; 5.6%); A. lumbricoides (35; 2.6%); E. vermicularis (22; 1.7%); H. nana (21; 1.6%); O. volvulus (16; 1.2%); Loa-loa (10; 0.8%); and cutaneous larva migrans (CLM) (8; 0.6%). There was an association between eosinophilia and presence of parasites (p<0.05), except for CLM (p=0.488) and D. fragilis (p=0.973) (Table 6). The duration of the trip was longer in the cases with eosinophilia, especially among VFR-travellers, but the differences were not statistically significant (VFR, p=0.468; travellers, p=0.663; VFR-travellers, p=0.627). There was an association between the length of residence and eosinophilia in the immigrants (immigrants, p<0.001; VFR, p=0.164).
Reasons for consultation according to the presence of eosinophilia.
| Total (5255) n (%) | Immigrants (3078) n (%) | VFR (788) n (%) | Travellers (1306) n (%) | VFR-travellers (83) n (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| E (1331) | No E (3924) | E (963) | No E (2115) | E (242) | No E (546) | E (106) | No E (1200) | E (20) | No E (63) | |
| Analytical abnormalities | 619 (46.5) | 358 (9.1) | 451 (46.8) | 307 (14.5) | 128 (52.9) | 26 (4.8) | 25 (23.6) | 24 (2.0) | 15 (75.0) | 1 (1.6) |
| Health examinations | 506 (38.0) | 1967 (50.1) | 408 (42.4) | 1251 (59.1) | 69 (28.5) | 281 (51.5) | 26 (24.5) | 413 (34.4) | 3 (15.0) | 22 (34.9) |
| Gastrointestinal symptoms | 105 (7.9) | 572 (12.5) | 45 (4.7) | 19 (5.3) | 27 (11.2) | 63 (11.5) | 32 (30.2) | 383 (31.9) | 1 (5.0) | 15 (9.5) |
| Skin symptoms | 61 (4.6) | 200 (5.1) | 36 (3.7) | 10 (2.9) | 10 (4.1) | 6 (4.2) | 14 (13.2) | 112 (9.3) | 1 (5.0) | 3 (4.8) |
| Febrile syndrome | 27 (2.0) | 576 (14.7) | 9 (0.9) | 15 (9.3) | 10 (4.1) | 5 (3.0) | 8 (7.5) | 241 (20.1) | 0 (0) | 10 (30.2) |
Analytical abnormalities: referred because of abnormalities in tests performed in another centre (eosinophilia, anaemia, intestinal protozoa, etc.); health examinations: asymptomatic cases requesting a health check-up; VFR: immigrants established in Spain who visit their country of birth; VFR-travellers: children or spouses of immigrants, born in Spain, who travel to the country of their parents/partners.
Most common parasites.
| Parasites | Total 5255 Immigrants 3078 VFR-immigrants 788 Travellers 1306 VFR-travellers 83 Cases (%) | With eosinophilia (1331) Immigrants 963 VFR-immigrants 242 Travellers 106 VFR-travellers 20 Cases (%) | pa |
|---|---|---|---|
| S. stercoralis | 502 (9.5) | 458 (34.4) | p<0.001 |
| Immigrants | 363 (11.8) | 327 (34.0) | p<0.001 |
| VFR | 115 (14.6) | 109 (45.0) | p<0.001 |
| Travellers | 21 (1.6) | 19 (17.6) | p<0.001 |
| VFR-travellers | 3 (3.6) | 3 (15.0) | p=0.012 |
| Schistosoma sp. | 237 (4.5) | 147 (11.0) | p<0.001 |
| Immigrants | 147 (4.8) | 100 (10.4) | p<0.001 |
| VFR | 32 (4.1) | 21 (8.7) | p<0.001 |
| Travellers | 50 (4.4) | 26 (24.5) | p<0.001 |
| VFR-travellers | 0 | 0 | – |
| S. mansoni | 47 (0.9) | 34 (2.6) | p<0.001 |
| Immigrants | 34 (1.1) | 23 (2.4) | p<0.001 |
| VFR | 9 (1.1) | 7 (2.9) | p=0.005 |
| Travellers | 4 (0.3) | 4 (3.8) | p<0.001 |
| VFR-travellers | 0 | 0 | – |
| S. haematobium | 40 (0.8) | 28 (2.1) | p<0.001 |
| Immigrants | 32 (1.0) | 23 (2.4) | p<0.001 |
| VFR | 1 (0.1) | 1 (0.4) | p=0.307 |
| Travellers | 7 (0.5) | 4 (3.8) | p=0.001 |
| VFR-travellers | 0 | 0 | – |
| Ancylostoma | 134 (2.5) | 115 (8.6) | p<0.001 |
| Immigrants | 103 (3.3) | 91 (9.4) | p<0.001 |
| VFR | 26 (3.3) | 21 (8.7) | p<0.001 |
| Travellers | 5 (0.4) | 3 (2.8) | p=0.005 |
| VFR-travellers | 0 | 0 | – |
| Trichuris trichiura | 105 (2.0) | 75 (5.6) | p<0.001 |
| Immigrants | 89 (2.9) | 66 (6.9) | p<0.001 |
| VFR | 12 (1.5) | 7 (2.9) | p=0.037 |
| Travellers | 3 (0.2) | 1 (0.9) | p=0.224 |
| VFR-travellers | 1 (1.2) | 1 (5.0) | p=0.241 |
| Ascaris lumbricoides | 76 (1.4) | 35 (2.6) | p<0.001 |
| Immigrants | 56 (1.8) | 28 (2.9) | p=0.002 |
| VFR | 10 (1.3) | 5 (2.1) | p=0.183 |
| Travellers | 7 (0.5) | 2 (1.9) | p=0.105 |
| VFR-travellers | 3 (3.6) | 0 | p=1.0 |
| Hymenolepis nana | 42 (0.8) | 21 (1.6) | p<0.001 |
| Immigrants | 34 (1.1) | 20 (2.1) | p<0.001 |
| VFR | 5 (0.6) | 1 (0.4) | p=1.0 |
| Travellers | 2 (0.2) | 0 | p=1.0 |
| VFR-travellers | 1 (1.2) | 0 | p=1.0 |
| Enterobius vermicularis | 29 (0.6) | 22 (1.7) | p<0.001 |
| Immigrants | 17 (0.6) | 13 (1.3) | p<0.001 |
| VFR | 8 (1.0) | 5 (2.1) | p=0.063 |
| Travellers | 0 | 0 | – |
| VFR-travellers | 4 (4.8) | 4 (20.0) | p<0.003 |
| Cutaneous larva migrans | 39 (0.7) | 8 (1.7) | p=0.488 |
| Immigrants | 3 (0.1) | 2 (0.2) | p=0.232 |
| VFR | 2 (0.3) | 1 (0.4) | p=0.520 |
| Travellers | 34 (2.6) | 5 (4.7) | p=0.189 |
| VFR-travellers | 0 | 0 | – |
| D. fragilis and C. belli | 20 (0.4) | 5 (0.4) | p=0.973 |
| Immigrants | 8 (0.3) | 4 (0.4) | p=0.267 |
| VFR | 2 (0.3) | 1 (0.4) | p=0.520 |
| Travellers | 9 (0.7) | 0 | p=1.0 |
| VFR-travellers | 1 (1.2) | 0 | p=1.0 |
| Onchocerca volvulus | 19 (0.4) | 16 (1.2) | p<0.001 |
| Immigrants | 15 (0.5) | 14 (1.5) | p<0.001 |
| VFR | 2 (0.3) | 1 (0.4) | p=0.520 |
| Travellers | 2 (0.1) | 1 (0.9) | p=0.156 |
| VFR-travellers | 0 | 0 | – |
| Loa-loa | 14 (0.3) | 10 (0.8) | p<0.001 |
| Immigrants | 13 (0.4) | 10 (1.0) | p=0.01 |
| VFR | 1 (0.1) | 0 | p=1.0 |
| Travellers | 0 | 0 | – |
| VFR-travellers | 0 | 0 | – |
| Parasitesb | 1183 (22.4) | 888 (66.7) | p<0.001 |
| Immigrants | 803 (26.1) | 643 (66.7) | p<0.001 |
| VFR | 218 (27.7) | 173 (71.5) | p<0.001 |
| Travellers | 146 (11.2) | 62 (58.5) | p<0.001 |
| VFR-travellers | 15 (18.1) | 10 (50.0) | p<0.001 |
VFR: immigrants established in Spain who visit their country of birth; VFR-travellers: children or spouses of immigrants, born in Spain, who travel to the country of their parents/partners.
Eosinophilia is a very common analytical finding in +REDIVI, predominating in males (p<0.001) and immigrants or VFR (p<0.001).
Immigrants and VFRThe prevalence of eosinophilia in immigrants and VFR in our study (31%) was higher than that observed in other studies on immigrant populations (9–27%).3,6,7,14–17 That could be explained by different reference values for eosinophilia, the area of origin of the study population (higher in the Latin American and sub-Saharan population) and periods of residence (more prevalent in studies where residence times are shorter).
Immigrants in our study were resident for long periods of time (3 years) before being seen at an international health unit. This may be a consequence of the administrative, labour and cultural difficulties faced by the study population18; a study in Madrid on 988 immigrants showed that 72% of them were undocumented.6 However, we did not collect these data. In addition, a lack of training among healthcare professionals in the management of eosinophilia can have serious consequences for both the individual and the public health system because of the high cost of treating the complications of certain helminthiases.16,19,20 Although very unlikely, this situation could also increase the risk of local transmission in Europe of some helminthic diseases, as occurred with schistosomiasis in Corsica.21 The immigrants with eosinophilia had shorter times of residence, which seemed logical given that some geohelminths that cause eosinophilia can disappear spontaneously. These differences were not found in the case of VFR, probably because they had been back to visit their country of origin since they had emigrated.
The most common countries of origin for immigrants with eosinophilia were Bolivia, Pakistan and Equatorial Guinea. These are not the most prevalent nationalities in Spain.2 However, Bolivians are one of the groups most commonly seen in international health centres, corresponding with the increase in cases of Chagas disease diagnosed in Spain.22 Barcelona also has the fifth largest Pakistani population of cities in Europe and the majority live in the centre of Barcelona, very close to one of the centres affiliated to REDIVI.23 Lastly, Equatorial Guinea was a Spanish colony until 1968 and, despite becoming independent, it has maintained close ties with Spain.24
As in other studies, we found no association between symptoms and the presence of eosinophilia.3 Parasites were diagnosed in 67–72% of immigrants and VFR with eosinophilia. This rate varies from 29% to 77% in other studies, probably depending on the country of origin of the cases and how long they have been resident, and on the type of tests performed.3,7,8,16,25 Multiple parasitosis was found in 15%, with rates from 4% to 45% in other studies.3,8,17 The most common parasites in immigrants and VFR with eosinophilia were strongyloidiasis (34% and 45%, respectively) and schistosomiasis (Schistosoma sp.+S. mansoni+S. haematobium) (15% and 12%, respectively). The high prevalence of strongyloides and schistosomes may be explained by the use of serological techniques with high sensitivity, but with the possibility of cross-reactions with other helminthiases.25,26 In addition, in the case of schistosomiasis, serology can remain positive indefinitely after treatment.25 Although not the most prevalent helminths in the world, they are of great importance for their potentially life-threatening nature.11,12A. lumbricoides, T. trichiura and hookworms all had a low prevalence in the REDIVI network. Their short life spans, together with the long periods of time the study population had been resident, may account for these results.12 Filariasis was also uncommon in immigrants and VFR (2.5 and 0.4%, respectively). Mass treatment programmes have probably led to its decline worldwide,13 although the prevalence can be higher (29%), as reported in other studies when serological techniques for diagnosis are prioritised.8 However, these techniques can have cross-reactions with other helminthiasis.27
Travellers and VFR-travellersIn the case of travellers, the prevalence of eosinophilia was 8%. The rate was similar in other studies (8%), but lower (5%) in studies that used higher values to define eosinophilia (≥8%).9,10 In VFR-travellers, the prevalence of eosinophilia was higher (24%), probably because they are more likely to be exposed to parasitic diseases during their travels.28 The duration of the trip was longer in the cases with eosinophilia, especially among VFR-travellers, but the differences were not statistically significant. The size of the sample probably prevented this association from being demonstrated. Nonetheless, it seems reasonable to assume that children or spouses of immigrants, born in Spain, are travelling for longer and risk a greater degree of exposure to parasites, and it is therefore worth taking special care in this group of travellers.
Parasites were diagnosed in 50–59% of travellers and VFR-travellers, a value higher than that observed in other studies (14–45%), but which could also be explained by the increasing use of serological parasite detection techniques.9,10,29 Multiple parasitosis was detected in 5–10%, these rates being lower than those reported in other studies (17%).29 In travellers, the most prevalent parasitic disease was schistosomiasis (similar to other studies), followed by strongyloidiasis.9,29 Probably leisure activities more typical in the Western world (such as bathing in rivers) are the risk factors that most determine parasitic infections in travellers. In VFR travellers, enterobiasis was the most prevalent parasitic infection. As reported by other studies, the presence of filariasis in this type of traveller is very uncommon.10 The association between eosinophilia and the majority of parasitic infections was demonstrated, although in some cases it was not significant as a result of the absence or small number of cases.
Possible limitationsThe REDIVI network collects information from a number of international health centres and infectious diseases units in Spain, but not all Spanish centres participate. At the time of study, six autonomous regions were represented (Catalonia, Andalusia, Valencia, Basque Country, Andalusia and Castilla-La Mancha), four of which have the highest immigrant populations in Spain.30
The values for eosinophilia are not well defined in the literature. For this study, each centre used its own criteria, although in more than 75% of cases, eosinophilia was defined as >500/mm3 or >7%.
The eosinophilia protocols at each centre are based on international recommendations, but may vary from one centre to another as they are adapted to the particular situation in each case, depending on experience of microscopic techniques or accessibility to certain tests. We cannot confirm that the protocol was fully adhered to in all cases, and it is therefore possible that the actual number of cases of eosinophilia secondary to parasitic infection was higher than that reported.
In conclusion, when eosinophilia is detected in a person who has lived in areas endemic to helminthiasis, specific diagnostic tests should be performed regardless of the type of migration or the presence of symptoms. Although the likelihood of finding eosinophilia is significantly greater in immigrants who are newcomers (time of residence less than 3 years), it may persist beyond that period (>6 years). The rates for presence of eosinophilia tend to be higher the longer the duration of the trip, especially in VFR-travellers. It is important to stress that the parasitic diseases most frequently diagnosed are strongyloidiasis and schistosomiasis. If not diagnosed early, these helminthiases can have serious consequences for the individual, and involve high costs for the public health system and the risk of local transmission in the host country. Helminth infection can also exist with a normal eosinophil count and all migratory groups should therefore be subject to helminth screening, but especially immigrants and VFR. And if eosinophilia is detected in individuals with such a history, more extensive tests should be performed.
FundingThis study was supported by the 6th National R&D&I Plan 2008–2011, ISCIII-General Division of Cooperative Research Networks and Centres, the European Regional Development Fund (ERDF) and the Cooperative Research Network on Tropical Diseases (RICET): RD12/0018/0019 and RD12/0018/0020.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Hospital General de Albacete: María Martínez.
Hospital General Universitario de Alicante: Diego Torrús.
Hospital Basurto, Bilbao, Bizkaia: Miren Zuriñe Zuberu.
Hospital Cruces, Barakaldo, Bizkaia: Josune Goikoetxea.
Hospital San Cecilio, Granada: Rubén Gálvez.
Unitat de Salut Internacional Drassanes, PROSICS, Barcelona: Jordi Gomez, Antoni Soriano, Diana Pou, Begoña Treviño, Nuria Serre.
Hospital La Fe, Valencia: Eva Calabuig.
Hospital de Fuenlabrada, Madrid: José Manuel Ruiz Giardín.
Hospital de Guadalajara: Esteban Martín Echevarría.
Centro de Atención Primaria [Primary Care Centre] Guayaba, Madrid: Paloma Aguilera.
Hospital Infanta Sofía, San Sebastián de los Reyes, Madrid: Inés Suarez, Eduardo Malmierca.
Hospital La Paz, Madrid: Marta Mora.
Hospital Universitario Príncipe de Asturias, Alcalá de Henares, Madrid: Gerardo Rojo, Juan Antonio Cuadros.
Hospital Ramón y Cajal, Madrid: Rogelio López-Vélez, Francesca Norman, Begoña Monge, Ángela Martínez, José Antonio Pérez-Molina.
Hospital Universitario San Juan de Alicante, Sant Joan d’Alacant, Alicante: José Maria Cuadrado Pastor.
Hospital Virgen de la Macarena, Seville: Belén Gutiérrez, Ángel Domínguez.
Hospital Universitari Vall d’Hebron, Barcelona: Israel Molina, Fernando Salvador, Adrian Sánchez.
Please cite this article as: Serre-Delcor N, Treviño B, Monge B, Salvador F, Torrus D, Gutiérrez-Gutiérrez B, et al. Prevalencia de la eosinofilia y factores relacionados en los viajeros e inmigrantes de la red +REDIVI. Enferm Infecc Microbiol Clin. 2017;35:617–623.