Febrile neutropenia is a very common complication in patients with hematological malignancies receiving chemotherapy, and is associated with high morbidity and mortality. Infections caused by multidrug-resistant bacteria have become a therapeutic challenge in this high-risk patient population, since inadequate initial empirical treatment can seriously compromise prognosis. However, reducing antimicrobial exposure is one of the most significant cornerstones in the fight against resistance. The objective of these new guidelines is to update recommendations for the initial management of hematological patients who develop febrile neutropenia in this scenario of multidrug resistance. The two participating Societies (the Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica [Spanish Society of Infectious Diseases and Clinical Microbiology] and the Sociedad Española de Hematología y Hemoterapia [Spanish Society of Haematology and Haemotherapy]), designated a panel of experts in the field to provide evidence-based recommendations in response to common clinical questions. This document is primarily focused on bacterial infections. Other aspects related to opportunistic infections, such as those caused by fungi or other microorganisms, especially in hematopoietic stem cell transplantation, are also touched upon.
La neutropenia febril es una complicación muy frecuente en los pacientes hematológicos que reciben tratamiento quimioterápico, y se asocia a una importante morbimortalidad. Las infecciones por bacterias multirresistentes se han convertido en un reto terapéutico en esta población de pacientes de alto riesgo, en los que un tratamiento empírico inicial inadecuado puede comprometer gravemente su pronóstico. Sin embargo, reducir la exposición a los antimicrobianos es uno de los pilares más importantes en la lucha frente a las resistencias. El objetivo de esta nueva guía es actualizar las recomendaciones sobre el manejo inicial del paciente hematológico que desarrolla neutropenia febril en el escenario actual de multirresistencia. Para la elaboración de este documento, las 2 sociedades implicadas (la Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica y la Sociedad Española de Hematología y Hemoterapia) designaron expertos en este tema, quienes han realizado recomendaciones basadas en la evidencia, en respuesta a cuestiones clínicas habituales. Este documento está enfocado básicamente a la infección bacteriana. Otros aspectos relacionados con las infecciones oportunistas, como las producidas por hongos u otros microorganismos, sobre todo en el seno del trasplante de progenitores hematopoyéticos, se abordan de forma tangencial.
Recent years have witnessed the re-emergence of bacterial infections with a gram-negative etiology in patients with febrile neutropenia (FN), together with a significant increase in their resistance to antimicrobials. These epidemiological changes are of particular importance in hematologic patients with FN because inadequate initial empirical antibiotic therapy can have a serious adverse effect on prognosis in high-risk patients. Likewise, the management of infections caused by multidrug-resistant bacteria is a major clinical problem in this population.
The management of hematologic patients has also changed in recent years, with a tendency towards outpatient care and new types of immunosuppressive treatment. In the era of multidrug resistance, the objective of these new guidelines is to update the recommendations for the initial management of hematologic patients who develop FN. This document focuses basically on bacterial infection. Other aspects associated with opportunistic infections, such as fungal infections or those due to other microorganisms, especially in hematopoietic stem cell transplantation (HSCT), are also touched upon. Only infections in adult patients will be discussed.
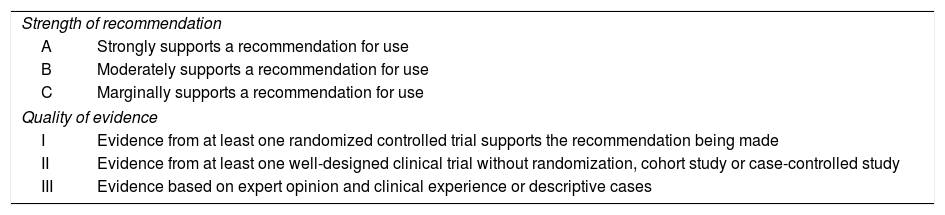
MethodologyThe two participating Societies, the Spanish Society of Infectious Diseases and Clinical Microbiology (Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica) and the Spanish Association of Hematology and Hemotherapy (Sociedad Española de Hematología y Hemoterapia) nominated two coordinators, who selected the rest of the members of the panel of experts. The scientific committees of both societies approved the proposal. The questions to be considered were approved by both scientific societies involved and then distributed among the various members of the panel of experts. The present Document was written following the SEIMC guidelines for consensus documents (www.seimc.org), as well as the recommendations of the AGREE collaboration (www.agreecollaboration.org) for evaluating the methodological quality of clinical practice guidelines. The PubMed search engine (http://www.ncbi.nlm.nih.gov/pubmed) was used to perform a literature search of the MEDLINE database for relevant scientific publications. The key words used for each question are also shown. Only complete articles published in English or Spanish were selected. No specific period of inclusion was defined, although authors were instructed to gather the most recent evidence from the literature to form the basis of their answers. The coordinators wrote the first draft, which was submitted for review by the panel of experts and by SEIMC members after being published on the web page of that society. The complete text has been approved by all authors. The criteria used to evaluate the strength of the recommendation and the quality of the evidence are summarized in Table 1. Possible conflicts of interest associated with all members of the panel of experts are listed at the end of the document.
Strength of recommendations.
| Strength of recommendation | |
| A | Strongly supports a recommendation for use |
| B | Moderately supports a recommendation for use |
| C | Marginally supports a recommendation for use |
| Quality of evidence | |
| I | Evidence from at least one randomized controlled trial supports the recommendation being made |
| II | Evidence from at least one well-designed clinical trial without randomization, cohort study or case-controlled study |
| III | Evidence based on expert opinion and clinical experience or descriptive cases |
- 1.
What tools are available to determine risk in a patient with FN? When should they be applied and in what contexts?
Search terms: “Risk factors” “Risk stratification”, “Febrile neutropenia”, “Cancer patients”.
- 1.
Patients presenting with FN should undergo risk assessment for complications, preferably in the first hour of contact with the healthcare system (A-II).
- 2.
The MASCC (Multinational Association for Supportive Care in Cancer) risk index is a prognostic scale that can be used to assess the risk of complications in patients with FN (B-II).
- 3.
A patient with a MASCC risk index score of <21 is defined as high risk (B-II) and should be hospitalized and receive intravenous empirical antibiotic treatment (B-II).
- 4.
A patient with a MASCC risk index score of ≥21 is defined as low risk (B-II). Some of these patients may be candidates for a regimen of oral antibiotics and can be managed as outpatients, provided that they are not receiving induction chemotherapy for acute myeloid leukemia or in the pre-engraftment phase of allogeneic hematopoietic stem cell transplantation (B-II).
- 5.
Clinical criteria can also be used to determine risk in patients with FN.
- 6.
Patients with an absolute neutrophil count (ANC) of ≤100/mm3, expected neutropenia duration of >7 days, and/or significant comorbidities (hypotension, pneumonia, gastrointestinal symptoms, neurological symptoms) are considered high-risk. These patients should be admitted to hospital and receive intravenous empirical therapy (A-II).
- 7.
Patients with ANC<500/mm3, expected neutropenia duration ≤7 days and having no or few comorbidities or significant evidence of renal or hepatic impairment are considered as at low-risk. These patients may be candidates for oral empirical therapy and outpatient care (A-II).
Diagnostic management
- 1.
What microbiology diagnostic tests should be carried out in patients with FN?
Search terms: “Febrile neutropenia” AND “Etiology”. “Febrile neutropenia” AND “Microbiological diagnosis”.
- 1.
It is recommended that at least two, and preferably three, sets of blood cultures be collected from any patient with FN, whether they are in-patients or seen in the emergency room, high-risk or low-risk. Blood should be drawn through all available catheterized venous access in the patient, paying special attention to long-term devices, as well as samples taken by venipuncture from peripheral vein sites (A-I).
- 2.
If an infection of extravascular origin is suspected, it is recommended to send representative samples from the possible focus of infection. Rapid microbiological tests can be performed on these samples (A-I).
- 3.
For patients being monitored in an outpatient setting with symptoms or radiological signs of respiratory infection, rapid urine antigen tests for the detection of Streptococcus pneumoniae and Legionella pneumophila antigens can be used (A-II).
- 4.
During annual flu epidemics, molecular methods should be used for early diagnosis. In the case of flu, rapid techniques on nasopharyngeal swabs are preferred (B-II).
- 5.
If the patient presents diarrhea, it is advisable to request a Clostridium difficile toxin stool test, on which rapid immunochromatographic assays or PCR can be performed (C-III).
- 2.
When and how should pre-emptive screening for fungal infection be carried out?
Search terms: “Febrile neutropenia AND fungal infection diagnosis”, “Febrile neutropenia AND investigation for invasive fungal infection”.
- 1.
In patients with FN, pre-emptive screening for fungal infection should be considered when fever persists for 4–7 days after having started broad-spectrum antibiotics, expected duration of neutropenia is >7 days, and in clinically compatible cases (A-I).
- 2.
Blood cultures are the microbiological test of choice for the diagnosis of yeast infections (A-I).
- 3.
In clinically stable patients who are not receiving antifungal prophylaxis against filamentous fungi, it is recommended to screen for Aspergillus infection by carrying out serial testing for circulating galactomannan (GM) in serum twice a week. In the event of a positive GM test, a CT scan of the lungs is recommended (A-I).
- 4.
In patients receiving antifungal prophylaxis against filamentous fungi, a CT scan of the thorax is recommended if fever persists (>7 days after initiating broad-spectrum antibiotics, with no other identifiable cause of fever). In the event of findings suggestive of invasive fungal infection, bronchoscopy is recommended for galactomannan testing, and pan-fungal PCR on the bronchoalveolar lavage (BAL) fluid. If results are negative, lesion puncture is recommended (B-II).
- 3.
Are biomarkers useful for infection diagnosis in FN and for determining length of antibiotic treatment?
Search terms: “Biomarkers and infection diagnosis”, “Febrile neutropenia”, “Bacteremia and biomarkers”, “Length of antibiotics in febrile neutropenia”.
- 1.
Biomarkers are not recommended as a guide to antibiotic use in FN, due to the lack of studies demonstrating the safety and usefulness of basing clinical decisions on their results (B-III).
- 2.
It has been demonstrated that neutropenic patients with bacteremia present significantly higher procalcitonin (PCT), C-reactive protein, IL-6, and presepsin levels than those without bacteremia. (A-II). The possible impact of this information on the future management of FN is yet to be clarified.
- 3.
Biomarkers are not useful for determining length of antibiotic treatment (A-II).
- 4.
C-reactive protein levels, especially those that are elevated (>20–30mg/dl), are correlated with greater mortality. This relationship has not been demonstrated with the other biomarkers (PCT, presepsin, IL-6) (C-III).
Empirical antibiotic treatment
- 1.
What empirical treatment strategies are there for patients with NF?
Search terms: “Febrile neutropenia”, “Empirical antibiotic treatment”.
- 1.
Any febrile patient with an ANC of <500/mm3 and those with ANC of 500–1000/mm3 and predicted to decline imminently should receive early empirical antibiotic treatment (A-II) with an appropriate broad-spectrum antibiotic (A-I) and a bactericidal agent.
- 2.
Surveillance programs (antimicrobial stewardship) established in the center for the appropriate use of antibiotic treatment should be taken into consideration (B-III).
- 3.
A strategy of dose-escalation can be applied in patients with an uncomplicated clinical presentation, no previous colonization/infection with multidrug-resistant bacteria, and in centers where there is a low incidence of drug-resistant microorganisms (B-II). In other situations, a de-escalation strategy should be applied (B-II).
- 2.
What is the empirical antibiotic treatment of choice when there is no obvious clinical focus of infection?
Search terms: “Febrile neutropenia”, “Empirical antibiotic treatment”, “Fever unknown origin”.
- 1.
It is recommended to use a beta-lactam antibiotic with antipseudomonal activity as monotherapy, or in combination with another antibiotic, depending on the risk of infection due to multidrug-resistant microorganisms and clinical presentation (A-I).
- 2.
For the escalation strategy:
- 2.1
Use of piperacillin-tazobactam (A-I), or cefepime (A-I), or ceftazidime (B-II) is recommended.
- 2.2
In settings with a high prevalence of ESBs, cephalosporins and piperacillin-tazobactam in monotherapy are not recommended (B-II).
- 3.
For the de-escalation strategy:
- 3.1
Imipenem or meropenem in monotherapy are recommended for use (B-II), or a combination of antipseudomonal beta-lactam plus an aminoglycoside or a fluoroquinolone (if it has not been used as prophylaxis) (B-III). Carbapenems should be reserved for critically ill patients.
- 3.2
The aminoglycoside should be given in a single daily dose (A-II). The need to continue the aminoglycoside should be reassessed at 48–72h.
- 3.3
If there is risk of infection due to multidrug-resistant nonfermenting gram-negative bacilli, it is recommended to combine the beta-lactam with the lowest antimicrobial resistance rate in the center+amikacin or colistin (B-III).
- 3.4
The need for empirical treatments with other combinations can be considered, according to local epidemiology or in outbreak settings (C-III).
- 3.5
The use of antibiotics with activity against gram-positive cocci resistant to beta-lactams (vancomycin, daptomycin, linezolid) would be indicated only in cases of hemodynamic instability and/or risk of methicillin-resistant Staphylococcus aureus (MRSA) infection (B-III).
- 3.6
The empirical addition of vancomycin to initial antibiotic therapy is not recommended if fever persists at 3 days (A-I).
- 3.7
In hemodynamically unstable patients, treatment should be started immediately with a broad-spectrum beta-lactam with antipseudomonal activity together with an antibiotic active against beta-lactam-resistant gram-negative bacilli, and a drug with activity against methicillin-resistant gram-positive cocci (B-III). In patients with septic shock not receiving antifungal prophylaxis, consider adding active treatment against Candida spp to the initial regimen (C-III).
- 3.
What is the empirical treatment of choice when there is an obvious clinical source of infection?
Search terms: “Febrile neutropenia”, “Empirical antibiotic treatment”
- 1.
Oropharyngeal mucositis/esophagitis
- 1.1
In patients with mild forms of mucositis, anaerobic coverage is not essential and cefepime may be used (B-III).
- 1.2
In more severe forms, ensure anaerobe coverage with piperacillin-tazobactam, imipenem or meropenem (A-III).
- 1.3
Consider initiating antiviral and/or antifungal treatment in patients not receiving prophylaxis who have suggestive oral lesions or symptoms compatible with esophagitis (C-III).
- 2.
Neutropenic enterocolitis (typhlitis)
- 2.1
Start treatment with a broad-spectrum antibiotic such as piperacillin-tazobactam, imipenem or meropenem that includes activity against gram-negatives, Gram-positives and anaerobes (A-III).
- 2.2
Consider adding treatment for C. difficile if there is a high index of suspicion (C-III).
- 3.
Perianal infection
- 3.1
Performing a digital rectal examination is contraindicated in the neutropenic patient. Nevertheless a thorough examination of the perianal region is fundamental (B-III).
- 3.2
The treatments of choice are piperacillin-tazobactam, imipenem or meropenem (A-III).
- 3.3
If there is clinical suspicion of a perianal abscess, ensure active treatment against gram-negative bacilli, Enterococcus spp. and anaerobes (A-III).
- 4.
Skin and soft tissue infection (SSTI)
- 4.1
Start treatment with a broad-spectrum, antipseudomonal beta-lactam agent with activity against Gram-positive cocci, including S. aureus (A-III).
- 4.2
Consider adding an antibiotic with activity against MRSA if there is a history of previous colonization/infection (B-III).
- 4.3
It is recommended to obtain a sample of tissue for microbiological and histopathologic analysis from any skin lesion suspected of being a source of infection (B-III).
- 4.4
The possibility of a serious necrotizing soft tissue infection should always be ruled out (B-III).
- 4.5
If a serious necrotizing infection is suspected, it is recommended to use agents such as clindamycin that inhibit protein synthesis, and so inhibit toxin production (A-III).
- 5.
Intravascular catheter-related infection
- 5.1
Start treatment with an antipseudomonal beta-lactam together with an agent with specific activity against drug-resistant Gram-positive organisms such as vancomycin or daptomycin (A-III).
- 5.2
Linezolid is not recommended in this situation (B-III).
- 5.3
If the infection is considered serious and the catheter is the obvious source of infection, remove the catheter promptly before the microbiological results are known (B-III).
- 6.
Paranasal sinuses
- 6.1
Start treatment with a broad-spectrum antipseudomonal beta-lactam with activity against Gram-positive cocci, including S. pneumoniae and S. aureus (A-III).
- 6.2
In risk patients (prolonged neutropenia, corticotherapy), consider adding treatment with activity against Aspergillus or Mucorales, which can give a picture of sinusitis that is initially difficult to differentiate from one with a bacterial etiology (B-III).
- 7.
Pneumonia
- 7.1
Start with a broad-spectrum beta-lactam with activity against S. pneumoniae and P. aeruginosa (A-III).
- 7.2
In critically ill patients, nosocomial cases and patients previously colonized/infected with MDR gram-negative bacilli, it is advisable to combine with a second antibiotic, according to local epidemiology (B-III).
- 7.3
If the infection is community-acquired and an atypical pneumonia is suspected, consider combining with fluoroquinolones or macrolides (B-III).
- 7.4
In patients with MRSA colonization or epidemiological settings of high endemicity, combination with an active agent such as linezolid or vancomycin must be considered. (B-III).
- 7.5
During flu epidemics, add empirical treatment with oseltamivir (C-III). Once samples have been collected and the results are known, continuation or withdrawal of treatment can be assessed.
- 7.6
In risk patients with bilateral infiltrates, consider other possible etiologies (Pneumocystis jirovecii, cytomegalovirus) (B-III).
- 8.
Urinary tract infection
- 8.1
Start with a beta-lactam with antipseudomonal activity (A-III).
- 8.2
Consider adding a second antibiotic in critically ill patients, those with indwelling urinary catheters, and/or a previous history of colonization/infection with multidrug-resistant bacteria, according to local epidemiology (aminoglycoside, glycopeptide) (B-III).
- 9.
Central nervous system infections
- 9.1
In cases of acute meningitis, antibiotic treatment should include a beta-lactam with activity against S. pneumoniae and P. aeruginosa with good penetration into cerebrospinal fluid (CSF) (cefepime or meropenem) and ampicillin to cover Listeriamonocytogenes (A-III).
- 9.2
In risk patients with suggestive clinical forms, or patients with space-occupying lesions, consider other etiologies (Cryptococcus, Listeria, Nocardia, filamentous fungi, toxoplasmosis and Mycobacterium tuberculosis (B-III).
- 4.
What is the duration of antibiotic treatment in patients with FN without clinically or microbiologically documented infection?
Search terms: “Duration OR discontinuation” AND “Neutropenia” AND “Antimicrobial OR antibiotic” AND “Therapy OR treatment”.
- 1.
Empirical antibiotic treatment can be stopped in hematologic patients with FN who do not have clinically or microbiologically documented infection, if they have been afebrile for at least 72h, and hemodynamically stable and asymptomatic since presentation, regardless of neutrophil count or expected duration of neutropenia (A-II).
- 2.
After treatment is discontinued, the patient should be kept under close clinical observation for at least 24–48h, so that antibiotic treatment can be restarted early if fever returns (B-II).
- 3.
Centers that provide antibacterial prophylaxis should consider restarting it after stopping empirical antimicrobial therapy for as long as the neutropenia lasts (C-III).
- 5.
Can patients with FN be treated with oral antibiotics? When? Which antibiotics?
Search terms: “Febrile neutropenia”, “Oral treatment”, “Hematological malignancies”.
- 1.
Patients considered to be at low risk for complications can be treated with oral antibiotics provided that they are also properly followed-up in the outpatient setting (A-II).
- 2.
Treatment must include a fluoroquinolone with antipseudomonal activity (ciprofloxacin 750mg/12h/po) and an agent fully active against Gram-positive cocci, such as amoxicillin/clavulanic acid (875mg/8h/po), or clindamycin (300–600mg/8h po), if the patient has a proven allergy to all beta-lactams or a history of hypersensitivity (A-I). Another alternative is a combination of ciprofloxacin with cefixime or cefuroxime (A-II).
- 3.
Other oral regimens including levofloxacin or ciprofloxacin in monotherapy have been studied less (B-III).
- 4.
Fluoroquinolones should not be used as initial empirical treatment in patients who have received them as prophylaxis. (A-III).
- 5.
Any patient, whether in the emergency room or after admission, who presents signs and symptoms of hemodynamic instability, focality, oral intolerance, new clinical signs and symptoms, or microbiological species not susceptible to initial empirical therapy are isolated, should be admitted to hospital or continue as an inpatient in order to expand the tests for fever syndrome and modify empirical treatment according to the protocol for high-risk patients (A-III).
- 6.
When is empirical antifungal treatment indicated in a patient with NF?
Search terms: “Febrile neutropenia AND empirical antifungal treatment”. “Febrile neutropenia AND pre-emptive antifungal therapy OR diagnostic-driven approach”.
- 1.
High-risk neutropenia patients not receiving prophylaxis against filamentous fungi can be given empirical antifungal treatment if fever with no other obvious cause persists after 4–5 days of broad-spectrum antibiotics and hemodynamic instability (B-II).
- 2.
Alternative treatment strategies, such as biomarker-guided treatment using galactomannan (GM) or beta-D-glucan (BDG), reduce the use of antifungals safely and without affecting mortality in neutropenic patients (A-I).
- 3.
Empirical antifungal treatment is not recommended in the vast majority of hematologic patients with high-grade neutropenia who receive antifungal prophylaxis covering filamentous fungi (A-II).
Targeted antibiotic treatment
- 1.
In documented cases of microbiological isolates, can antibiotic treatment be adjusted to the susceptibility of the microorganism identified, even if neutropenia persists?
Search terms: “targeted OR de-escalation” AND “therapy OR treatment” AND “febrile neutropenia” AND “antimicrobial OR antibiotic”.
- 1.
In patients with documented microbiological isolates, treatment should be targeted at the isolate, taking into account its in vitro activity (including MIC), pharmacokinetic/pharmacodynamic properties, as well as the individual characteristics of the patient (A-I).
- 2.
If the microorganism isolated is considered to be the only causative agent of the febrile episode, it is preferable to use an antimicrobial, normally a beta-lactam, with a narrower spectrum when active (B-III).
- 3.
Beta-lactam monotherapy is appropriate for targeted treatment of most cases of gram-negative bacteremia (A-I).
- 2.
What is the duration of antibiotic treatment in patients with FN and clinically or microbiologically documented infection?
Search terms: “duration OR discontinuation” AND “neutropenia” AND “antimicrobial OR antibiotic” AND “therapy OR treatment”.
- 1.
In hematologic patients with FN and clinically documented infection, antibiotic treatment can be discontinued when the clinical signs and symptoms of infection have resolved and the patient has been afebrile for at least 72h (B-II).
- 2.
In hematologic patients with FN and microbiologically documented infection, treatment should be maintained until clinical and microbiological cure of infection (resolution of signs and symptoms of infection and microbiological eradication) and after at least 4 days of apyrexia and a minimum of 7 days of antibiotic treatment (B-III).
- 3.
In both situations, if neutropenia persists after treatment has been discontinued the patient should be kept under close clinical observation for at least 24–48h, so that antibiotic treatment can be restarted promptly if fever recurs (B-II).
- 4.
Centers that give prophylactic antibacterial agents should consider renewing this regimen when empirical antibiotics have been discontinued for as long as the neutropenia continues (C-III).
- 3.
When is removal of a central venous catheter indicated?
Search terms: “central venous catheter removal”, “catheter-related infection”, “management of central venous catheter infection” “catheter-related bloodstream infection”.
- 1.
When CVC infection is documented, consider removal of the catheter wherever possible, weighing up the advantages of removal against the difficulty of obtaining new venous access (A-II).
- 2.
It is recommended to remove the CVC when there is documented catheter-related bloodstream infection (CRBSI) and local signs at the insertion site (suppuration), along the tunnel tract (tunnel infection), or if the patient presents criteria for severe sepsis with hemodynamic instability (septic shock) (A-II).
- 3.
To improve the prognosis of the patient, it is recommended to remove the CVC when there is documented CRBSI due to fungi (normally Candida spp), S. aureus, enterococci, gram-negative bacilli (especially P. aeruginosa) and mycobacteria (A-II). Removal is also recommended in infections with associated bacteremia caused by microorganisms that are difficult to eradicate (Bacillus spp., Micrococcus spp. and Propionibacterium spp.) (B-II).
- 4.
In uncomplicated infections or where bacteremia is caused by microorganisms different from those mentioned above, systemic targeted antibiotic treatment can be applied without removing the CVC and antibiotic lock therapy should be considered (B-II).
- 5.
Removal of the CVC is recommended if persistent bacteremia is detected (evidenced in positive follow-up control cultures) 48h-72h after starting targeted antibiotic treatment (A-II), if there is no other obvious clinical focus (B-II), if there is infective endocarditis or peripheral embolism (A-II) or an early relapse due to the same microorganism after completion of antibiotic treatment, or failure of conservative treatment (B-II).
- 6.
If fever persists in a neutropenic patient with an indwelling catheter after other focalities have been ruled out, but catheter-related infection has not been confirmed, consider removal of the catheter if there is sepsis or local erythema in the pericatheter area (B-II), or if fever persists and there is no other possible cause despite the absence of sepsis or local signs of infection (C-III).
Treatment of infections caused by multidrug-resistant Gram-negative bacilli (MDR-GNB)
- 1.
What is the treatment of choice for cephalosporin-resistant Enterobacteriaceae?
Search terms: “(ESBL or extended-spectrum beta-lactamase) and treatment and outcome”; “AmpC and Enterobacter* and treatment and outcome”.
- 1.1
Targeted therapy in infections caused by extended-spectrum beta-lactamase (ESBL)-producing Enterobacteriaceae
- 1.1.1
In stable patients, the targeted therapy of choice against extended-spectrum beta-lactamase (ESBL)-producing Enterobacteriaceae is a beta-lactam/beta-lactamase inhibitor (BLBLI) combination, provided that in vitro susceptibility is shown (B-II).
- 1.1.2
Use of carbapenems is recommended for patients with sepsis or septic shock criteria (C-I).
- 1.1.3
Piperacillin-tazobactam and meropenem should be administered in extended infusion, since this has been shown to improve prognosis in severe infections compared with short-term infusions (A-I).
- 1.1.4
Piperacillin-tazobactam should be avoided for treating high-inoculum infections caused by strains with MIC≥4mg/L (B-II).
- 1.2
Targeted therapy in infections caused by AmpC-producing Enterobacteriaceae
- 1.2.1
Cefepime and fluoroquinolones are the preferred treatment options for infections due to AmpC-producing Enterobacteriaceae susceptible to these antimicrobials (B-II).
- 1.2.2
Piperacillin-tazobactam is a valid therapeutic option if in vitro activity is shown (B-II), but should be avoided for treating high-inoculum infections caused by AmpC- producing Enterobacteriaceae with MIC≥4mg/L (B-III).
- 1.2.3
Use of carbapenems is recommended for patients without alternative treatment options, or with sepsis or septic shock criteria (C-I).
- 1.2.4
We recommend that piperacillin-tazobactam, cefepime and meropenem be administered in extended infusion, since this has been shown to improve the prognosis in severe infections when compared with short-term infusions (A-I).
- 2.
What is the treatment of choice for carbapenem-resistant Gram-negative bacilli?
- 2.1
Targeted treatment of infections caused by carbapenem-resistant Enterobacteriaceae (CRE).
Search terms: “(carbapenemase or KPC or OXA or NDM or VIM) and treatment and outcome”.
- 2.1.1
Severe infections caused by KPC-producing Enterobacteriaceae in neutropenic patients should be treated with a combination of at least two active drugs from the options included in the antibiogram (meropenem, colistin, tigecycline, fosfomycin and aminoglycosides) (B-II). We recommend the same approach for treating severe infections caused by other carbapenemase-producing Enterobacteriaceae (CRE) (C-III).
- 2.1.2
For infections caused by strains with meropenem MICs<16mg/L, the combination regimen should include high-dose meropenem (2g every 8h) in extended infusion (over 3h) (B-II).
- 2.1.3
Ceftazidime-avibactam may be an alternative for severe infections due to KPC-producing or OXA-48-producing Enterobacteriaceae (C-III). We do not have well-designed comparative studies available that enable this drug to be positioned against other treatment options (undecided). Nor are there data to support its use in combination therapy (undecided).
- 2.1.4
In this type of infection, it is especially important to ensure control of the source of infection and to administer high-dose antibiotics with optimized dosage regimens, monitoring plasma levels whenever possible (Table 4) (B-II).
- 2.2
Targeted therapy of extensively drug-resistant (XDR) and pandrug-resistant (PDR) non-fermenting gram-negative bacilli (NFGNB).
Search terms: BGN-NF XDR and PDR: (Acinetobacter or Pseudomonas) and (resistant or resistance or MDR or XDR or PDR) and treatment and outcome.
- 2.2.1
In the case of XDR NFGNB infections for which there is a fully active therapeutic alternative, single-agent treatment is recommended with optimized administration (B-I), prioritizing the use (in the following order) of beta-lactams, sulbactam (in infections due to A. baumannii) and colistin, provided that in vitro susceptibility is shown (C-II). Avoid monotherapy with aminoglycosides or tigecycline for the treatment of severe infections (A-II, A-I).
- 2.2.2
For severe infections due to XDR-NFGNB strains with borderline susceptibility to the available treatment options, optimized administration of combination therapy using two or more agents should be considered, based on the best options specified in the antibiogram (B-II).
- 2.2.3
For XDR or PDR P. aeruginosa infections, use of ceftolozane-tazobactam may be considered (C-II) or ceftazidime-avibactam (C-I), although there is as yet limited experience of their use in this setting.
- 2.2.4
If these options are not available or the infection is caused by pan-resistant isolates, it will be necessary to develop combination therapy regimens using two or more agents, choosing those with intermediate susceptibility, or whose MICs are closest to the susceptibility cut-off (C-III).
- 2.2.5
It is particularly important in these infections to ensure control of the source of infection and to administer high-dose antibiotics with optimized administration regimens, monitoring plasma levels whenever possible (B-II).
- 3.
Targeted treatment of Stenotrophomonas maltophilia infections.
Search terms: “Stenotrophomonas and treatment”.
- 3.1
The treatment of choice for infections due to S. maltophilia is co-trimoxazole (trimethoprim 15mg/kg/day in 3–4 divided doses) (C-II).
- 3.2
In patients with infections with co-trimoxazole-resistant strains, or those who cannot take co-trimoxazole (because of hypersensitivity, for example), the recommended treatment is minocycline (C-II) or fluoroquinolones (C-II) if they are active. There is more limited experience of the use of ceftazidime, tigecycline and colistin in monotherapy (C-III). In the case of patients with serious or refractory infections who require second-line therapy, consider combining two drugs with in vitro activity categorized as susceptible.
Adjuvant measures and prevention
- 1.
Is the use of colony-stimulating factors indicated for treatment of FN? When?
Search terms: “febrile neutropenia”, “colony stimulating factor”, “treatment”.
- 1.
Colony-stimulating factors (CSF) are not routinely recommended in the treatment of FN (B-II).
- 2.
They can be considered for therapeutic use in patients with increased-risk for infection-related complications or predictive factors of poor prognosis (B-II).
- 2.
When would granulocyte transfusion be indicated?
Search terms: “febrile neutropenia”, “granulocyte transfusion”.
- 1.
There is insufficient evidence of the efficacy of granulocyte transfusion in patients with FN and documented infection (C-III).
- 2.
Granulocyte transfusions should be administered only in the context of prospective clinical trials (B-III).
- 3.
Is antibacterial prophylaxis indicated? Which drugs?
Search terms: “febrile neutropenia”, “antibacterial prophylaxis”.
- 1.
Antibacterial prophylaxis is not recommended in low-risk patients (A-I).
- 2.
In high-risk patients (ANC<500/mm3>7 days), use of antibacterial prophylaxis should be evaluated on an individual basis in accordance with the characteristics of the patient and local hospital epidemiology, owing to the lack of benefit for mortality and the increasing levels of resistance in gram-negative bacteria (B-I). If prophylaxis is used, epidemiological surveillance for MDRO detection should be implemented.
- 4.
Is prophylaxis with colony stimulating factors indicated? When?
Search terms: “febrile neutropenia”, “colony stimulating factor”, “prophylaxis”
- 1.
The decision to use colony-stimulating factor prophylaxis for the prevention of FN should be based on the relative myelotoxicity of the chemotherapy regimen and the presence of potential risk factors, which should be evaluated before each cycle of chemotherapy is administered.
- 2.
In situations where chemotherapy dose intensity or dose density strategies confer a survival benefit, prophylaxis with G-CSF should be used as supportive treatment (A-I).
- 3.
Primary prophylaxis is recommended from the first chemotherapy cycle for patients whose overall risk of FN is ≥ 20%, based on patient-related, disease-related and regimen-related risk factors (A-I).
- 4.
When the overall risk of FN is 10%–20%, attention should be focused on additional risk factors (such as comorbidities or advanced age), which increase the risk of FN and support an indication of prophylaxis with G-CSF (A-I).
- 5.
Prophylaxis with G-CSF is not recommended if chemotherapy has an FN risk of <10% (A-I).
- 6.
Secondary prophylaxis is recommended for patients who experienced neutropenic complications in a previous cycle of chemotherapy and in whom a dose reduction or delay in treatment could compromise progression-free or overall survival, or treatment outcome (A-I).
- 7.
Prophylaxis can be given with any of the following factors (filgrastim, lenograstim and pegfilgrastim) or any of their available biosimilars (A-I), preferably subcutaneously.
Carlota Gudiol has served as speaker at scientific meetings sponsored by Pfizer, MSD, Astellas and Gilead. Rafael de la Cámara has participated as speaker at scientific meetings sponsored by MSD, GSK, Novartis, Astellas, Pfizer and Gilead; and in consultancy and advisory activities for Novartis, MSD, Janssen, Clinigen and Astellas. Manuel Lizasoain has participated as speaker at scientific meetings sponsored by Pfizer, MSD and Gilead. Jordi Carratalà has participated as speaker at scientific meetings sponsored by Pfizer, MSD, Gilead and Angelini. Rafael Cantón has participated as speaker at scientific meetings sponsored by Angelini, ERN Laboratorios, MSD, Pfizer and Zambon and has received funding for research projects from AstraZeneca and MSD. Manuela Aguilar-Guisado has participated as speaker at scientific meetings sponsored by Pfizer and MSD. Manuela Aguilar-Guisado has participated as speaker at scientific meetings sponsored by Pfizer and MSD. José Molina Gil-Bermejo has received lecturing fees in activities financed by Merck Sharp & Dohme, and has received grants to attend conferences organized by Astellas Pharma. Carlos Solano has participated as speaker at scientific meetings sponsored by Pfizer, MSD, Astellas and Gilead He has received grants for clinical and preclinical research from Pfizer and Astellas. Carolina García-Vidal has received fees for speaking at events sponsored by Gilead Science, Merck Sharp and Dohme, Pfizer, Janssen and Novartis, and has received a subsidy from Gilead Science. María Lourdes Vázquez López has participated as speaker at scientific meetings sponsored by Pfizer, MSD, Gilead, Astellas, Amgen. José Ramón Azanza has participated as speaker at scientific meetings sponsored by Pfizer, MSD, Gilead, Janssen, AstraZeneca, Roche. José Ramón Azanza has participated as speaker at scientific meetings sponsored by Pfizer, MSD, Gilead, Janssen, AstraZeneca, Roche Francisco Javier Candel has participated as speaker scientific meetings sponsored by Pfizer, MSD, Gilead, Angelini, Astellas, and ERN. Isabel Ruiz-Camps has participated as speaker at scientific meetings sponsored by Astellas, Celgene, Gilead, MSD, Pfizer and in scientific consultancy for Astellas, Gilead, and Pfizer. María Suárez-Lledó has participated as speaker at scientific meetings and has collaborated in scientific studies sponsored by Pfizer and MSD. Isidro Jarque has participated as speaker at scientific meetings sponsored by Gilead, MSD, and Pfizer. Isabel Sánchez-Ortega has no conflicts of interest.
The authors would like to thank Antonio Gutiérrez-Pizarraya for his comments and technical support in the preparation of this document. They would also like to thank the members María Illescas and Juan Manuel García-Lechuz Moya for their comments from society members during the revision phase of the document.
The complete consensus statement is available as Appendix in supplementary material.