We present the case of a 50-year-old woman from Arequipa (Peru), in Spain for the past four days on a leisure trip, who consulted due to pain and inflammation in the 3rd finger of the left hand and 4th finger of the right hand which had started 24h previously. She had no fever, chills, or other systemic symptoms. A month earlier, she suffered several cuts to those fingers while handling beef, associating an episode of acute cellulitis for which she received a dose of intramuscular antibiotic; she did not remember which. The lesions were completely resolved.
She is currently consulting for spontaneous reappearance of purplish erythema, mild oedema, increased temperature and intense pain on palpation in the 3rd finger of the left hand and on the two distal phalanges of the 4th finger of the right hand (Fig. 1). Adenopathies were not palpable in the adjacent lymph node territory. Given clinical suspicion, it was decided to take a skin biopsy for a targeted microbiological study and empirical antibiotic treatment with amoxicillin was started.
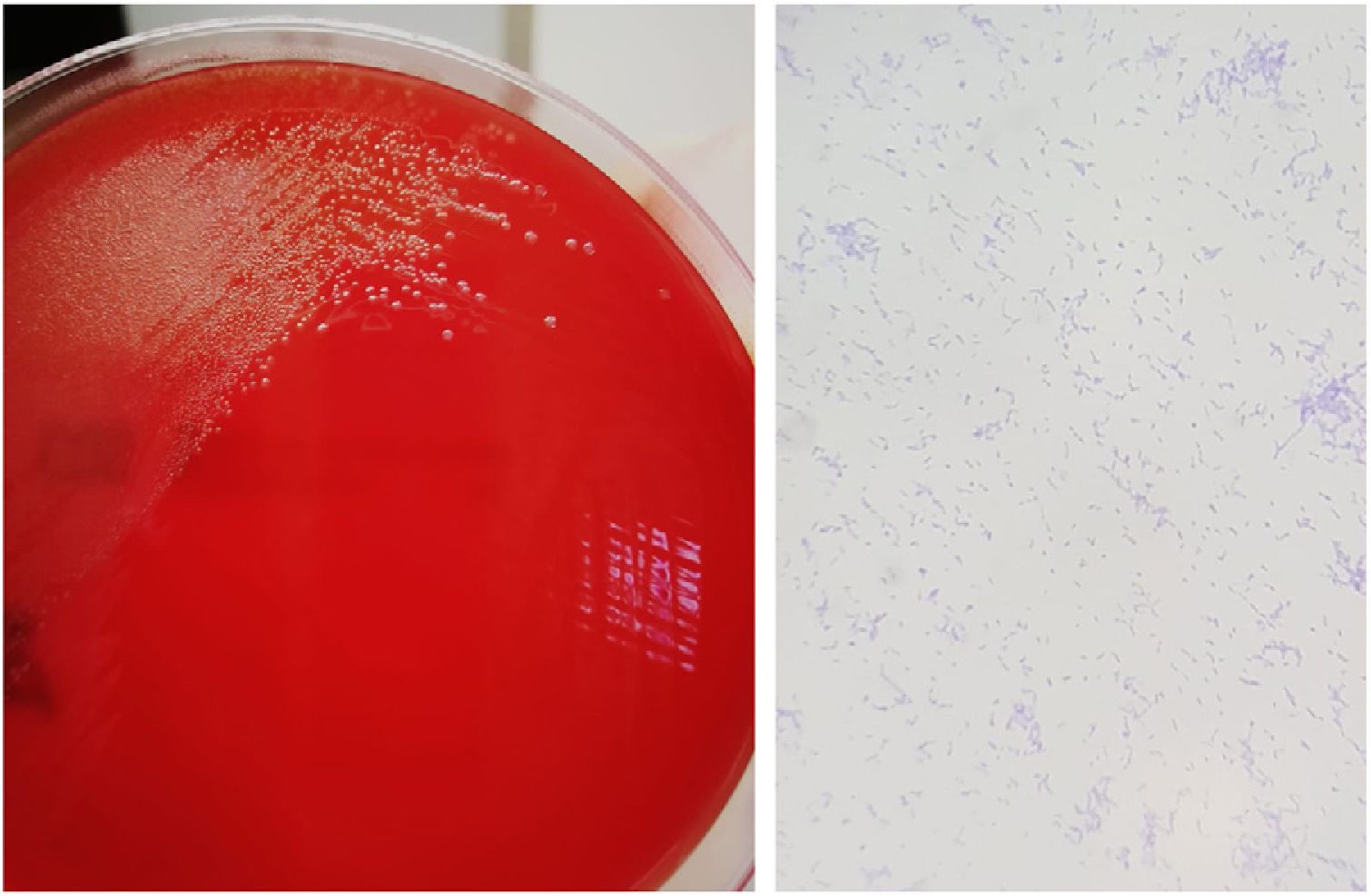
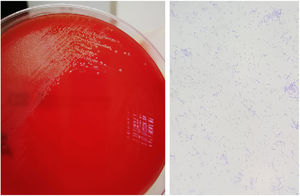
OutcomesA skin biopsy was performed by puncture in the 3rd finger of the left hand, obtaining a cylinder of skin including all the layers of the dermis. The sample was seeded in the media blood agar, chocolate agar, Schaedler agar and in thioglycollate enrichment broth (bioMérieux®). Growth of whitish colonies with slight betaheamolysis was detected on the Schaedler agar plate incubated under anaerobic conditions (Fig. 2). The microorganism was identified as Erysipelothrix rhusiopathiae (E. rhusiopathiae) through MALDI-TOF (Bruker®).
The patient was reassessed clinically after completing a week of antibiotic treatment, aiming for complete healing of the skin lesions described. The return to her country of origin prevented subsequent clinical surveillance and detection of possible recurrences.
Final commentsWe are faced with the typical presentation of skin infection localised by E. rhusiopathiae, also known as “erysipeloid of Rosenbach”.1E. rhusiopathiae is a pleomorphic, non-spore-forming gram-positive bacillus, ubiquitous in nature. It is responsible for skin and systemic infections in both animals and humans,2 who are infected by contact with animals, their waste or excreta. Therefore, it is considered an occupational disease of farmers, veterinarians, butchers, fishermen and, also, of cooks and housewives, as in the case presented.1 It is believed that technological advances in the animal industry have been able to reduce the incidence of this type of infection in our environment,2 but we must take into account its appearance in other environments where the handling of animal products is still common.
The skin infection localised by E. rhusiopathiae (erysipeloid) is characterised by purplish lesions, with an active edge and central pallor in its progression, with disproportionate pain within reach of the skin lesion. It mainly affects fingers or hands, since it is acquired by small wounds or cuts when handling animal products (such as bones, including fish bones).
The characteristic purplish erythema of a subacute course, the absence of suppuration and the significant pain associated with this type of cellulitis, as well as the epidemiological history, helps us to differentiate it from those cases of cellulitis caused by streptococci or staphylococci.1
The study of superficial samples or aspiration of the lesion can be negative because the microorganism is located deep in the dermis, requiring the inclusion of all the layers of the dermis in the biopsy.3
Although this infection tends to heal spontaneously in 3-4 weeks, recurrences are common, as occurred in our patient. Antibiotic treatment usually allows for complete healing of the infection.1
E. rhusiopathiae should be included in the differential diagnosis of skin infections associated with contact with animals, especially in professionals with habitual exposure. Its subacute and recurrent course can make diagnosis difficult by distancing it from the epidemiological history.
Please cite this article as: Verdejo MÁ, López-Valle A, Rivas G, Zarco C. Celulitis recurrente importada, la importancia de la anamnesis. Enferm Infecc Microbiol Clin. 2020;38:291–292.