The prevalence and predisposing factors were determined for inappropriate urinary catheterization (UC) among inpatients in medical wards.
MethodsA cross-sectional study was conducted including all patients aged ≥18 years admitted to medical wards in a 1300-bed tertiary-care centre, and who had a urinary catheter in place on the day of the survey.
ResultsOf 380 patients observed, 46 (12.1%) had a urinary catheter in place. Twelve of them (26.1%) were inappropriately catheterized. The most common indication for inappropriate UC was urine output monitoring in a cooperative, non-critically ill patient. Inappropriateness was associated with increased age, poor functional status, urinary incontinence, dementia, and admission from a long-term care facility.
ConclusionsFurther educational efforts should be focused on improving catheterization prescribing practices by physicians.
Pretendemos analizar la prevalencia y los factores asociados al empleo inapropiado de catéteres urinarios (CU) en los servicios médicos.
MétodosRealizamos un estudio de corte transversal que incluyó a todos los pacientes (≥18 años) ingresados en servicios médicos de un centro de tercer nivel de 1.300 camas y que eran portadores de CU el día de la observación.
ResultadosDe los 380 pacientes observados, 46 (12,1%) eran portadores de un CU. La cateterización fue juzgada inapropiada en 12 de ellos (26,1%). El motivo más habitual para el uso inapropiado de CU fue la monitorización de la diuresis en un paciente colaborador y no crítico. El uso inapropiado de CU se asoció con la edad, la situación funcional, la presencia de incontinencia urinaria, el diagnóstico de demencia y la institucionalización previa.
ConclusionesEs preciso mejorar los hábitos de prescripción de CU mediante esfuerzos educativos específicos.
Urinary catheterization (UC) constitutes a well-documented risk factor for the development of nosocomial urinary tract infections (NUTI).1 Therefore, notable efforts have been devoted to reduce the use of urinary catheters both in number and duration, most of them focused on the implementation and diffusion of institutional guidelines.2,3 Despite such interventions, the rate of inappropriate UC among inpatients continues to be unacceptably high, even in tertiary-care centres.4–8 These somewhat disappointing results might be partially explained by the lack of awareness among attending physicians on the potential risks associated with UC. Moreover, to date there are no widely accepted guidelines for the indications of this procedure in non-surgical patients. The present study was aimed at identifying both patient factors as well as physician educational gaps that contribute to the inappropriate use of UC in medical wards.
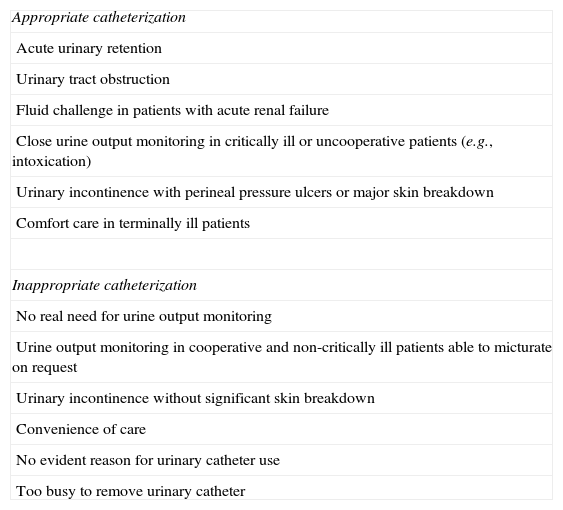
MethodsWe performed a cross-sectional study between 16 and 19 April, 2012 in the University Hospital “12 de Octubre” (Madrid, Spain), a 1300-bed tertiary-care centre with a reference population of 412,930 inhabitants in 2011. All the patients aged ≥18 years hospitalized in medical wards with a urinary catheter in place on the days of the survey were included. Patients with percutaneous nephrostomy tubes and condom or suprapubic catheters were excluded. For each patient the following data were recorded: demographics, underlying diseases, mental status at the time of UC, functional status, type of admission (whether the patient came from home or long-term care facility [LTCF]), duration and site of UC (emergency department [ED], medical ward, or long-term catheter), and indication for the procedure. The indication for UC was classified as appropriate or inappropriate by a researcher not involved in the day-to-day patient care based on a priori criteria determined by reviewing of previous literature (Table 1).5–7 Patient charts were reviewed for documentation of a physician order for UC and the explicit reason for the procedure. In those cases where no explicit indication could be determined, the authors analyzed the clinical scenario and determined the appropriateness. The attending physicians who cared for these patients were then asked whether they were aware of the placement of catheter and, if affirmative, about the reason for placement and duration of UC. Finally, a self-administered questionnaire was distributed among residents and staff physicians from each of the medical wards. The questionnaire consisted of 8 multiple-choice questions and tested physicians’ knowledge of the appropriate indications for UC and management of NUTI. The questionnaire was pilot tested using a convenience sample, and ambiguous questions were rephrased. Quantitative and qualitative variables data were shown as the mean±standard deviation or the median with interquartile range (Q1–Q3), and absolute and relative frequencies, respectively. Comparisons were made using the χ2 test, Fisher's exact test, Student's T test, or U Mann–Whitney test, as appropriate. Statistics were performed using SPSS v. 15.0 (Statistical Package for Social Sciences, Inc., Chicago, IL).
Criteria for appropriateness of urinary catheterization.
| Appropriate catheterization |
| Acute urinary retention |
| Urinary tract obstruction |
| Fluid challenge in patients with acute renal failure |
| Close urine output monitoring in critically ill or uncooperative patients (e.g., intoxication) |
| Urinary incontinence with perineal pressure ulcers or major skin breakdown |
| Comfort care in terminally ill patients |
| Inappropriate catheterization |
| No real need for urine output monitoring |
| Urine output monitoring in cooperative and non-critically ill patients able to micturate on request |
| Urinary incontinence without significant skin breakdown |
| Convenience of care |
| No evident reason for urinary catheter use |
| Too busy to remove urinary catheter |
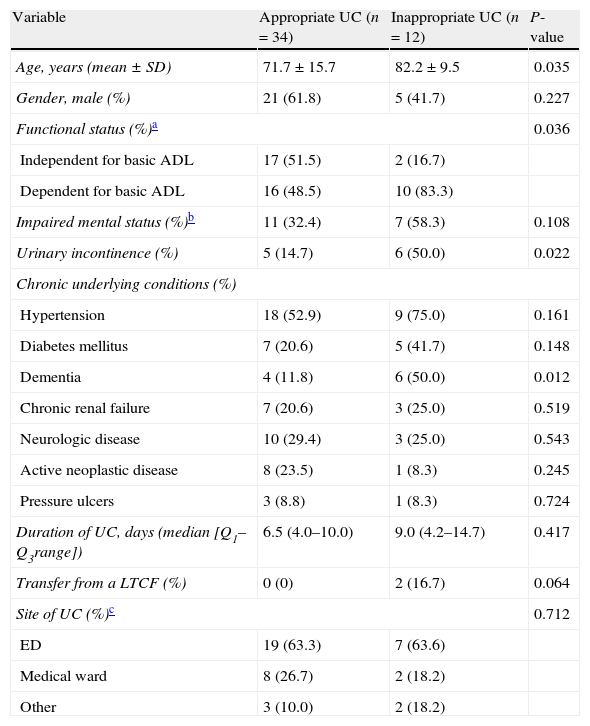
Of 380 patients hospitalized in medical wards at the time of the survey, 46 (12.1%) had a urinary catheter in place and were therefore included. Only 3 patients (6.5%) had a catheter already placed at the time of hospital admission, 26 patients (56.5%) were catheterized in the ED, 10 (21.7%) in the wards, and 6 (13.0%) in the department of intensive medicine. The median duration of UC was 7.0 days (Q1–Q3 range, 4.0–11.2 days). There was a physician order for UC in 47.8% of patient charts, whereas its indication was explicitly documented in only 41.3% of cases. Most attending physicians were aware that their patients had a catheter in place (95.7%), and knew the initial indication for UC (93.5%) and its duration (82.6%). According to our criteria, 12 patients (26.1%; 95% confidence interval, 13–39%) had an inappropriate indication for UC at the day of the survey. The initial indication in this group included: urine output monitoring (10 cases), 24-h urine specimen collection, and no obvious indication (one case each). Table 2 shows the comparison between patients with appropriate and inappropriate UC. Inappropriateness was associated with increased age, dependency for basic activities of daily life, urinary incontinence, diagnosis of dementia, and admission from a LTCF. The small sample size precluded multivariate analysis.
Clinical characteristics of patients with appropriate and inappropriate urinary catheterization.
| Variable | Appropriate UC (n=34) | Inappropriate UC (n=12) | P-value |
| Age, years (mean±SD) | 71.7±15.7 | 82.2±9.5 | 0.035 |
| Gender, male (%) | 21 (61.8) | 5 (41.7) | 0.227 |
| Functional status (%)a | 0.036 | ||
| Independent for basic ADL | 17 (51.5) | 2 (16.7) | |
| Dependent for basic ADL | 16 (48.5) | 10 (83.3) | |
| Impaired mental status (%)b | 11 (32.4) | 7 (58.3) | 0.108 |
| Urinary incontinence (%) | 5 (14.7) | 6 (50.0) | 0.022 |
| Chronic underlying conditions (%) | |||
| Hypertension | 18 (52.9) | 9 (75.0) | 0.161 |
| Diabetes mellitus | 7 (20.6) | 5 (41.7) | 0.148 |
| Dementia | 4 (11.8) | 6 (50.0) | 0.012 |
| Chronic renal failure | 7 (20.6) | 3 (25.0) | 0.519 |
| Neurologic disease | 10 (29.4) | 3 (25.0) | 0.543 |
| Active neoplastic disease | 8 (23.5) | 1 (8.3) | 0.245 |
| Pressure ulcers | 3 (8.8) | 1 (8.3) | 0.724 |
| Duration of UC, days (median [Q1–Q3range]) | 6.5 (4.0–10.0) | 9.0 (4.2–14.7) | 0.417 |
| Transfer from a LTCF (%) | 0 (0) | 2 (16.7) | 0.064 |
| Site of UC (%)c | 0.712 | ||
| ED | 19 (63.3) | 7 (63.6) | |
| Medical ward | 8 (26.7) | 2 (18.2) | |
| Other | 3 (10.0) | 2 (18.2) | |
ADL: activities of daily life; ED: emergency department; LTCF: long-term care facility; SD: standard deviation.
Of the 63 questionnaires distributed, 55 were completed and returned by 38 resident and 17 staff physicians (overall response rate, 87.3%). The median percentage of correct responses was 62.5% (Q1–Q3 range, 62.5–75.0%). The questions for which the highest rates of correct responses were obtained were those concerning the risk factors for UC-related NUTI (94.5%) and the appropriateness of UC for urine output monitoring in uncooperative patients (96.4%). The questions for which the lowest percentage of correct answers were obtained were those focused on the daily risk of NUTI in patients with UC (45.5%), the inappropriateness of UC for convenience of care in patients with impaired mobility (49.1%), and the therapeutic approach to UC-related NUTI (50.9%). We found no significant differences in rates of correct responses according to the years of practice, category, or department of the surveyed physician.
DiscussionWe have found that one quarter of patients admitted to medical wards with a urinary catheter in place had an inappropriate indication for catheterization at the time of the survey. This figure is intermediate as compared to data from other studies, in which rates of inappropriate UC ranged from 15% to 54%.5,6 However, direct comparisons are hampered by differences in evaluation criteria and clinical setting due to the inclusion of surgical and critically ill patients in most of the studies.6–8 Non-surgical patients have been shown to be at increased risk for inappropriate UC,6,8 likely due to the lack of guideline-based indications for this specific population. Bhatia et al. found that 28.8% of patients were inappropriately catheterized in the medical wards of a tertiary-care hospital in New Dehli,9 which closely correlates with our results.
All the factors associated with inappropriate UC in this survey—age, dependency for basic activities of daily life, urinary incontinence, underlying diagnosis of dementia, and transfer from a LTCF—are considered as markers of frailty in elderly patients. Increased age4,6,8,10 and nonambulatory status4 have been identified as risk factors for inappropriate catheter use in previous studies. Unnecessary urine output monitoring—in a cooperative, non-critically ill patient who could micturate on demand—was the most common inappropriate indication for catheterization. Of note, we only assessed the appropriateness of catheter use at the day of the prevalence survey, not at initial placement. Thus, it could be hypothesized that catheters appropriately indwelled in the ED for close haemodynamic monitoring in acutely ill elderly patient with functional dependency were not removed on the floor once they were no longer necessary, on the sole basis of the convenience of personnel providing patient care. Accordingly, previous studies have shown that duration UC is a strong risk factor for inappropriate urinary catheter use.5,10 It is worth noting that the question with the lowest correct response rate among surveyed physicians was that concerning the inappropriateness of catheter use in patients with impaired mobility as the only potential justification for the procedure.
Despite the small sample size and the limitations of its non-prospective design, a number of messages can be drawn from this study: (1) one out of four patients admitted to a medical ward at a tertiary-care hospital is inappropriately catheterized; (2) older patients with low functional status and urinary incontinence are particularly at risk; (3) retained use of catheter after urine output monitoring may explain most cases of inappropriate UC; and (4) further educational efforts should be focused on improving physicians’ catheterization prescribing practices. We propose the implementation of a NUTI bundle that should include the daily observation and registration of the indication for UC, as well as a continuous assessment of the current need for maintaining such a device, by improving routine communication between nursing staff and attending physicians. In addition, educational and awareness campaigns are needed to discourage UC on the basis of convenience of care in non-critical patients with impaired mobility.
Conflict of interestThe authors have no conflict of interest to declare.
Funding sourceMario Fernández-Ruiz holds a research-training contract “Río Hortega” (CM11/00187) from the Spanish Ministry of Economy and Competitiveness (Instituto de Salud Carlos III).