A 74-year-old woman with a history of allopurinol allergy, arterial hypertension, dyslipidemia, atrial fibrillation, chronic renal failure beginning hemodialysis in 2008 through arteriovenous fistula (AVF). Renal transplantation was performed in 2011, lost due to acute humoral rejection, suffering a cytomegalovirus infection as complication. After suspending immunosuppression, she presented renal graft intolerance, therefore graft embolization was performed in 2012.
The creation of multiple access for hemodialysis were required including a right humeral-cephalic AVF performed in 2008, functional until 2014 due to thrombosis. Given the infeasibility for creation of native access, a left humero-axillary prosthetic AVF was performed in 2015, currently used for hemodialysis.
She was admitted to the emergency room with a 3-day history of pain, erythema and swollen in the area of the thrombosed AVF of the right elbow. She explained a self-limited episode of abdominal pain and diarrhea a week ago. On physical examination, phlogotic signs were observed in the fistula area of the right elbow, without pulsatile mass. In the contralateral arm, a functioning prosthetic fistula without inflammatory signs. The peripheral blood laboratory test reported a PCR 265mg/L and mild leukocytosis with neutrophilia. Blood cultures were collected and the patient was hospitalized with empirical antibiotic treatment (piperacillin–tazobactam 4g/12h, and 1 dose of 4g after dialysis).
EvolutionAfter 24-h of incubation (BD Bactec FX System), all blood cultures were positive for a gram negative bacilli identified as Salmonella spp. by MALDI-TOF MS (MADLI-Biotyper). Further agglutination (Bio-Rad®) identified the isolate as Salmonella enterica subsp. enterica Serogroup C2. Antimicrobial susceptibility was tested by microdilution method (MicroScan WalkAway) using EUCAST breakpoints 2019.1 The bacterial isolate was susceptible to ampicillin, piperacillin/tazobactam, cefotaxime, trimethoprim/sulfamethoxazole and ciprofloxacin. The antibiotic treatment was adjusted to ceftriaxone 1g/day.
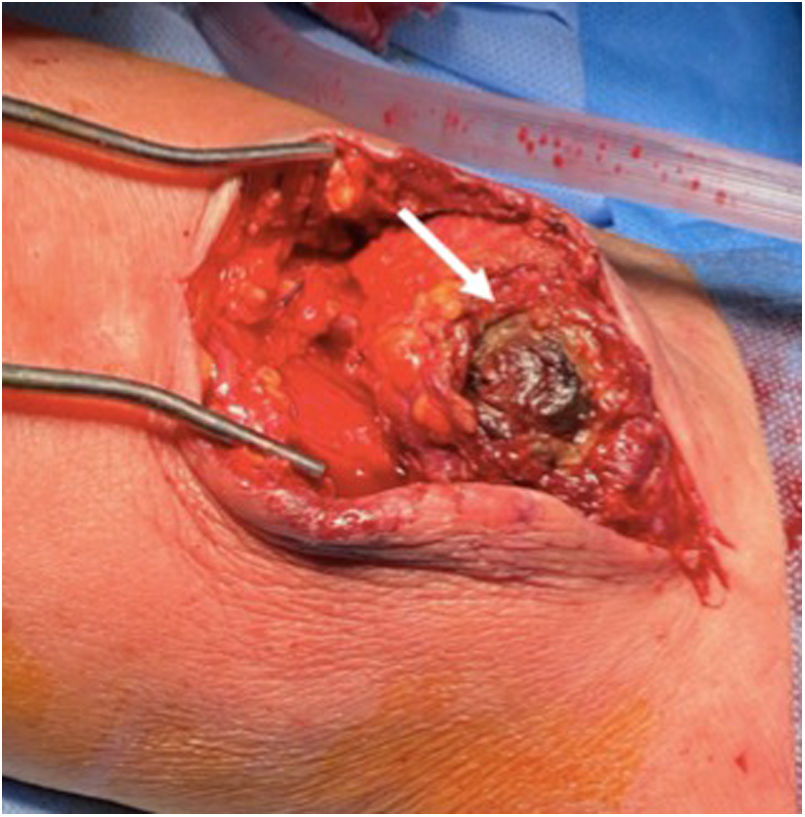
An angio-CT showed fistula thrombosis with abnormal subcutaneous cell tissue suggestive of inflammation (Fig. 1). At 48-h after hospitalization, the patient presented worsening pain and appearance of abscess. Urgent surgery was performed. Macroscopic findings of disruption of the venous wall (Fig. 2). It was performed a debridement and disconnection of AVF, associated with bicipital myoplasty.
Blood cultures and four arterial tissue samples were taken during the surgery. While the blood cultures were negative after 48h of appropriate antibiotic treatment, S. enterica serogroup C2 was isolated in all cultures of arterial samples.
A postoperative PET-CT with 18F-FDG revealed areas of hypercaptation affecting the anteromedial zone of the right arm and slight diffuse and heterogeneous uptake in the left upper limb prosthesis (Fig. 3). Conservative treatment of these findings was proposed in the absence of clinical signs that suggest infection.
Finally, the patient completed antibiotic treatment with ceftriaxone 1g/day for 2 weeks and then discharged with ciprofloxacin 500mg/12h until complete four weeks.
DiscussionSalmonella is a genus of rod-shaped gram-negative bacteria of the family Enterobacteriaceae.Salmonella serotypes include Typhi, Paratyphi and Nontyphoidal Salmonella. Nontyphoidal Salmonella infection occurs through the consumption of contaminated foods.2,3 In most salmonellosis outbreaks resulting from the consumption of poultry products, S. enterica ser. Enteritidis and ser. Typhimurium have been isolated, usually as a self-limited enterocolitis.4,5
Approximately 5% of cases of Salmonella gastroenteritis cause bacteremia, the arteritis association is unusual (1/10 cases). Nevertheless, it remains one of the most common causes of mycotic aneurysm due to the affinity of the bacterium to vascular tissues especially in large atherosclerotic areas, commonly aorta.6–8 The infection of peripheral arteries, especially in the upper extremity as infection of an arteriovenous fistula is fairly uncommon. Our patient illustrates a peculiar presentation of vascular infection by Nontyphoidal Salmonella. We consider that the AVF thrombosis, has played a role in the adherence to the fistula tissue.
The most frequent microorganisms involved in the infection of vascular accesses for hemodialysis are gram-positive cocci in approximately 70%, especially Staphylococcus aureus. Gram-negative bacilli cause between 10% and 20% of hemodialysis access cases.7
Uremic patients have a tendency of immunity defects specially cell-mediated. This could explain the accelerated infection's evolution in our patient. In these cases, antibiotic treatment alone is not eradicator. The association of surgical debridement is the key to success.9
Nonetheless, caution should be applied when interpreting PET-CT results. Various prosthetic materials and suture granulomas could present radiotracer uptake on PET-CT without having clinical repercussions.10