Lactobacillus includes one heterogeneous group of gram-positive, microaerophilic, non-sporulating, catalase-negative bacilli.1 They are part of the common bacterial flora within the oral cavity, the GI tract, and the genitourinary apparatus.2 Its isolation in clinical samples usually goes unnoticed due to its special nutritional requirements; long periods of incubation; and inadequate identifications through conventional systems.3 In most cases, they are usually regarded as contaminants; however, their participation in serious infections such as bacteremia, and endocarditis, especially in hosts with certain comorbidities has often been reported.3,4
We hereby present the case of a twenty-eight (28) year old male who was referred to our hospital for the surgical assessment of an aortic valve endocarditis. His personal history showed the presence of one bicuspid aortic valve. He presented to his hospital emergency room a 10-day history of fever and dyspnea. Upon his arrival, hemocultures were collected and one transthoracic echocardiogram was performed that showed the thickening of his bicuspid aortic valve, and a 5×7mm image of mobile nodules confirmed the presence of vegetation and severe aortic failure. Empirical antibiotic therapy with ampicillin, cloxacillin, and ceftriaxone was started. Since the patient's heart failure was getting worse and his fever persisted even after 72h of antibiotic treatment, the patient was referred to our center. After hospital admission, three (3) new sets of hemocultures were collected and the patient's valve was replaced by one biological device. All hemocultures obtained in our center tested positive 48–72h after incubation even though the patient was receiving antibiotic treatment.
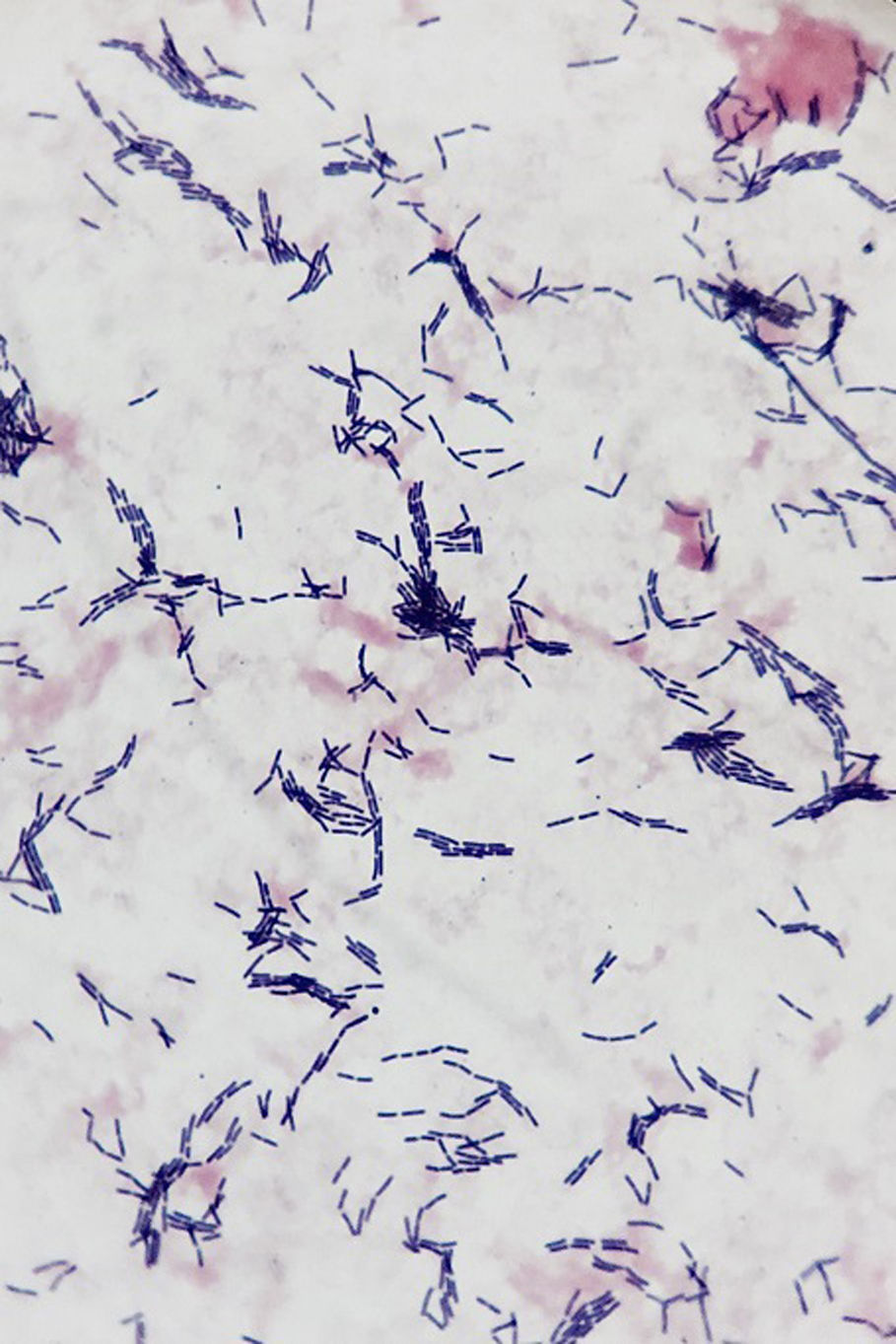
The Gram staining revealed the presence of one gram-positive, non-sporulating bacillus (Fig. 1) that was isolated in both blood agar and chocolate agar after 48h of incubation under aerobic and anaerobic conditions. Alpha-hemolytic and catalase-negative colonies were seen in pure cultures. Using the MALDI-TOF MS analysis (Bruker Daltonics, Bremen, Germany) the Lactobacillus rhamnosus bacteria was isolated (score: 2.18). Eventually, the 16S ARNr gene was sequenced showing 99 per cent homology with L. rhamnosus (GenBank: CP016823.1). The surgical material of the heart valve showed presence of L. rhamnosus bacteria too. Also, the reference hospital confirmed growth of L. rhamnosus in the hemocultures.
One antibiogram was conducted using the E-test method, and the minimal inhibitory concentration (MIC) was interpreted based on the recommendations established by EUCAST. The strain was sensitive to penicillin (MIC 0.25μg/ml); amoxicillin–clavulanic acid (MIC 0.75μg/ml); imipenem (MIC 0.75μg/ml); and clindamycin (MIC 0.047μg/ml). Once the microbiological results were available, a course of treatment with ampicillin (2g/4h), and gentamicin (240mg/24h) was started and it went on for another six (6) weeks. The patient was interrogated in search for any predisposing factors of lactobacilli endocarditis; the patient denied having any recent dental procedures done, but confirmed the daily use of probiotic products enriched with Lactobacillus.
L. rhamnosus is a rare cause of endocarditis and it has been reported in the medical literature in 18 cases only.5 The predisposing factors documented in the development of this entity are dental procedures, periodontitis, immunosuppression, heart valve disease, and the use of probiotics.5–7 In our patient, the combination of an underlying heart condition and the use of probiotics were the two (2) factors that most likely contributed to the patient's endocarditis due to L. rhamnosus. This microorganism is able to bind itself to different components of the extracellular matrix, such as collagen and fibrinogen, which allows its colonization and survival in valve surfaces.8
We should bear in mind that the L. rhamnosus bacteria may be erroneously identified using conventional methods.3 Nevertheless, the MALDI-TOF MS system allows us to conduct a quick and reliable identification of these microorganisms, which helps us minimize the need to use molecular techniques for their characterization.9 Most strains of L. rhamnosus are sensitive to penicillin and aminoglycosides. However, we may confront clinical manifestations of persistent bacteremia as it happened in our case due to the ability of this microorganism to reduce the pH of its environment through the production of lactic acid, which may complicate the way antibiotics behave.6
In sum, although it is a rare condition, lactobacillus endocarditis may occur, above all, in patients who have undergone dental procedures or have been treated with probiotics, especially if they show certain comorbidities such as immunosuppression, or structural heart disease. This is why we should not underestimate the importance of isolating it with hemocultures.
Please cite this article as: Recio R, Chaves F, Reyes CA, Orellana MÁ. Endocarditis infecciosa por Lactobacillus rhamnosus: riesgos del consumo de probióticos en un paciente con cardiopatía estructural. Enferm Infecc Microbiol Clin. 2017;35:609–610.