Pneumonia is a major cause of morbidity and mortality in children. Over the past 2 decades, a slight increase in the prevalence of Staphylococcus aureus as the causative agent has been observed.1 Among children hospitalised with community-acquired pneumonia (CAP), S. aureus is currently the causative agent in 1% of cases, and 15% of cases of typical CAP are of bacterial origin.2
A gradual increase in the rate of community-acquired methicillin-resistant S.aureus (MRSA) strains has also been observed in some countries.1,3 These isolates are characterised as being more virulent since Panton-Valentine leukocidin (PVL) is produced more readily,4 with MRSA pneumonia being more common in younger children, especially infants.1
A retrospective review of children under the age of 2 years hospitalised at our hospital with CA-MRSA pneumonia over the past 5 years (2013–2017) has been performed in order to describe their clinical and epidemiological characteristics.
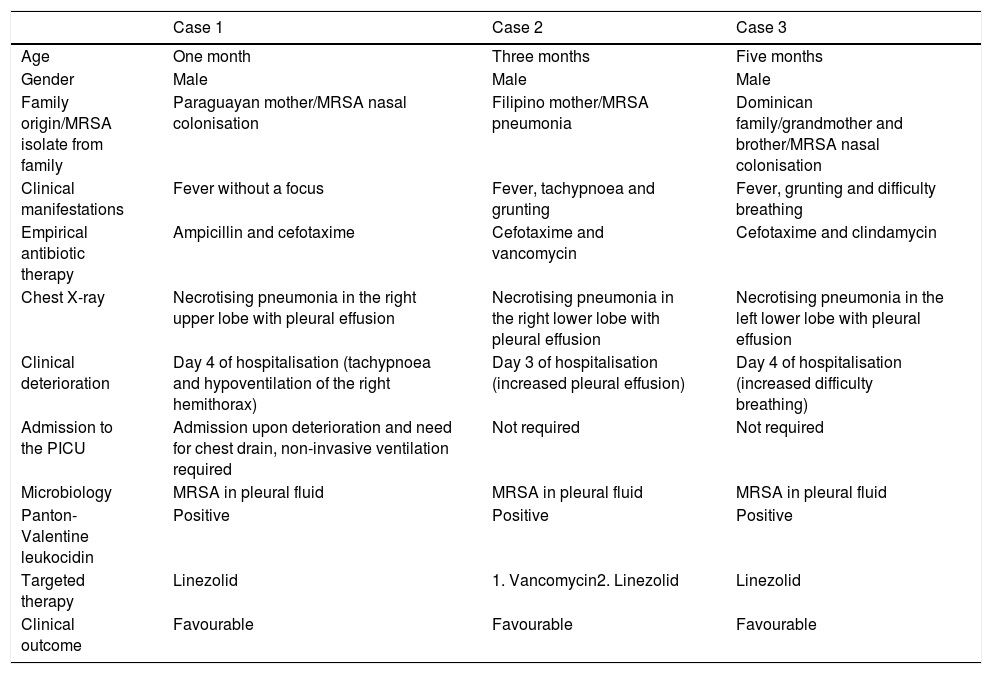
Three cases were identified, all involving children under the age of 6 months born in Spain to immigrant families (Table 1). The 3 patients developed severe pneumonia with pleural effusion and parenchymal necrosis (X-ray images included in Appendix. Supplementary material) and clinical deterioration was observed with the usual antibiotic therapy. All isolates were susceptible in vitro to clindamycin and trimethoprim-sulfamethoxazole. After getting the culture results back (3–4 days after hospitalisation), the antibiotic regimen was changed to linezolid in 2 cases while the third patient continued to receive vancomycin. However, this had to be changed to linezolid after 72h due to no signs of clinical improvement. The outcome was favourable in all cases, with complete clinical resolution at the time of discharge.
Characteristics of infants admitted with community-acquired methicillin-resistant Staphylococcus aureus pneumonia.
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Age | One month | Three months | Five months |
| Gender | Male | Male | Male |
| Family origin/MRSA isolate from family | Paraguayan mother/MRSA nasal colonisation | Filipino mother/MRSA pneumonia | Dominican family/grandmother and brother/MRSA nasal colonisation |
| Clinical manifestations | Fever without a focus | Fever, tachypnoea and grunting | Fever, grunting and difficulty breathing |
| Empirical antibiotic therapy | Ampicillin and cefotaxime | Cefotaxime and vancomycin | Cefotaxime and clindamycin |
| Chest X-ray | Necrotising pneumonia in the right upper lobe with pleural effusion | Necrotising pneumonia in the right lower lobe with pleural effusion | Necrotising pneumonia in the left lower lobe with pleural effusion |
| Clinical deterioration | Day 4 of hospitalisation (tachypnoea and hypoventilation of the right hemithorax) | Day 3 of hospitalisation (increased pleural effusion) | Day 4 of hospitalisation (increased difficulty breathing) |
| Admission to the PICU | Admission upon deterioration and need for chest drain, non-invasive ventilation required | Not required | Not required |
| Microbiology | MRSA in pleural fluid | MRSA in pleural fluid | MRSA in pleural fluid |
| Panton-Valentine leukocidin | Positive | Positive | Positive |
| Targeted therapy | Linezolid | 1. Vancomycin2. Linezolid | Linezolid |
| Clinical outcome | Favourable | Favourable | Favourable |
MRSA: methicillin-resistant Staphylococcus aureus; PICU: paediatric intensive care unit.
Methicillin resistance in community-acquired S. aureus in children was first described in Spain in 2006. These strains currently account for 5–10% of all community-acquired S. aureus isolates in children.5 Most of the cases reported are skin and soft tissue infections.5
Community-acquired S. aureus pneumonia is associated with high mortality rates (1–5%)6 and a higher risk of lung necrosis and abscesses.7 In a recent European study on invasive community-acquired S. aureus infections in children, methicillin-resistant isolates produced more cases of pneumonia than methicillin-susceptible strains and infection severity was associated with PVL production.4
MRSA pneumonia often presents with unilateral consolidation, pneumatoceles and pleural effusion8 and is more common in younger infants. At our hospital we found no cases of CA-MRSA pneumonia in infants over the age of 6 months. In children over the age of 2 years, the radiological findings, need for surgery and complications of MRSA pneumonia are similar to those observed in infants.6
MRSA carrier status increases the risk of pneumonia caused by this strain up to six-fold,3 and the rate of intrafamilial spread is very high.6 MRSA colonisation in Spain is more common among the immigrant population, especially among immigrants from South America.9 There is an ongoing spirited debate regarding the need for decolonisation in children and their family members. Decolonisation seems to be well advised in children with risk factors, such as premature infants, immunosuppressed children or patients admitted to intensive care units, and their relatives.
The American Academy of Pediatrics recommends the use of vancomycin or clindamycin in suspected cases of MRSA pneumonia.10 Once advantage of clindamycin is that it is active against PVL, but experience in actual cases of pneumonia is very limited and there may be resistant isolates. Vancomycin shows poor tissue penetration and its toxicity requires the use of serial loading doses. Linezolid is an excellent alternative, since its activity against MRSA is similar to that of vancomycin and it shows adequate penetration into lung tissue and antitoxic activity. Although the use of linezolid in paediatrics is off-label, pharmacokinetic and safety studies have demonstrated that it is a well-tolerated drug, with adequate plasma concentrations at the established doses, and that it also allows sequential administration due to its excellent oral bioavailability.
To conclude, MRSA must be suspected as the causative agent in cases of CAP with radiological signs of clinical deterioration (necrosis and pleural effusion) despite conventional empirical antibiotic therapy, especially in infants born to immigrant families. Linezolid is a good alternative to vancomycin in these patients.
Please cite this article as: Martín Espín I, Aguilera-Alonso D, García-Perea A, Baquero-Artigao F. Neumonías adquiridas en la comunidad por Staphylococcus aureus resistente a meticilina en lactantes. Enferm Infecc Microbiol Clin. 2019;37:551–552.