Mycobacterium lentiflavum is considered as a slow-growing nontuberculous mycobacterium (NTM). It was first described as a new species in 1996.1
We present the case of a 56-year-old woman, a former smoker with a five-pack-year history who had stopped 15 years previously, with no relevant medical history. She went to the Accident and Emergency department with haemoptysis, with an expectorated volume of up to 150 mL in 10 h. In view of her symptoms, she was given an emergency bronchoscopy, in which two blood clots were detected (in the right upper and lower lobes). Three days later, a second bronchoscopy was performed to complete the examination. The patient subsequently had a chest computed tomography (CT) scan, which showed bronchiectasis, nodular-looking images, discrete peribronchial ground-glass areas (likely related to recent bleeding), and hilar lymphadenopathy in the pathological range.
Three respiratory samples were taken (two bronchial aspirate obtained from the two different bronchoscopies and one sputum) and sent to the Microbiology laboratory, where microscopic examination was performed and they were cultured in solid medium (Coletsos) at 35 °C, and in liquid medium, using an automatic incubation and detection system: BACTEC MGIT 960 system (Becton Dickinson, Maryland, USA). In the auramine staining, acid-alcohol-fast bacilli were observed in all the samples. However, no Mycobacterium tuberculosis complex-specific DNA was detected by the commercial real-time PCR technique (BD MAX MDR-TB, BD New Jersey, USA) in any of the samples. While in hospital, the patient was started on empirical treatment with ceftriaxone and, in view of her adequate clinical progress, she was discharged to continue investigations as an outpatient. Identification of mycobacteria was still pending.
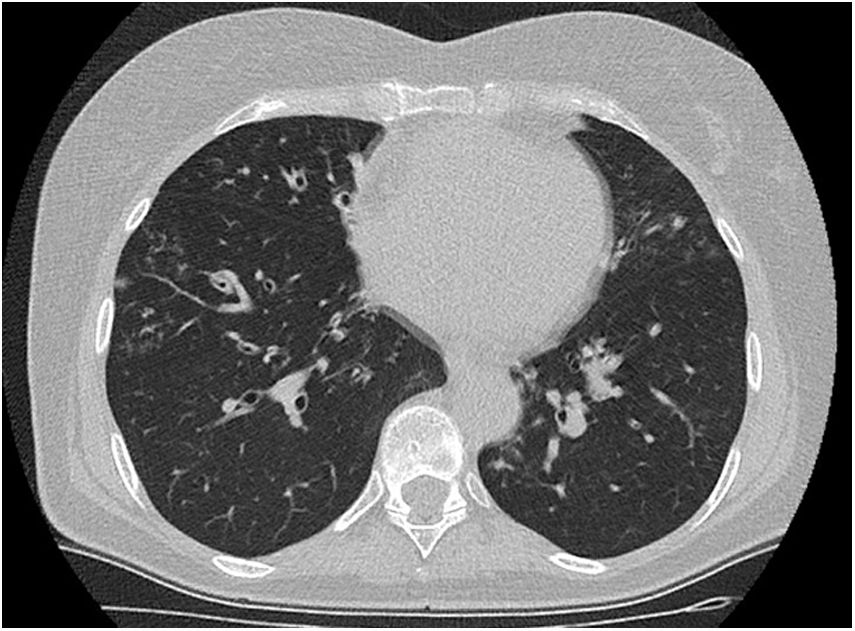
At two and a half months, the chest CT scan was repeated, showing persistence of bronchiectasis, nodular images and lymphadenopathy with disappearance of the discrete ground-glass areas (Fig. 1). The patient's respiratory function tests, autoimmunity tests and coagulation were all normal.
After two months of incubation, mycobacteria grew in the three respiratory samples, identified as M. lentiflavum by the strip-based reverse hybridisation and amplification method (GenoType® Mycobacterium AS [Hain Lifescience, Nehren, Germany]). As other aetiologies had been ruled out and the patient fulfilled clinical, radiological and microbiological criteria compatible with infection by M. lentiflavum,2 it was decided to start treatment with azithromycin, ethambutol and rifampin, with adequate initial tolerance. A month after starting treatment, the first control sputum was performed, which was negative for mycobacteria.
The patient has now completed eight months of treatment with no new episodes of respiratory infection and no medication side effects.
M. lentiflavum is a slow growing, scotochromogenic NTM, found mainly in soil and water, and it can cause infection in humans. It has a coccobacillary shape and in culture the colonies are small and pale yellow.
In childhood, it is the main cause of cervical lymphadenitis, while in adulthood it is associated with lung infection or disseminated disease in immunosuppressed patients. Some authors have described it as the third most common NTM in patients with cystic fibrosis.3 The most extensive review of cases published to date of respiratory infection by this NTM has 16 patients not infected with the immunodeficiency virus, and the majority are older women who are not showing an aggressive clinical course.4
This infection is described as being predominant in women with a mean age of 60, similar to the age of the patient we present here. It is usually benign; however, there is a published case of necrotising pneumonia with parapneumonic pleural effusion in an immunocompetent patient.5 Radiologically, it tends to present as bronchiectasis, nodules, or with a tree-in-bud pattern, and it has been described as a causal agent for super-infection of pre-existing bronchiectasis.6
From a therapeutic point of view, given the low prevalence of this infection, there are no standardised guidelines in the various official guidelines which cover the management of NTM infections. However, it is described as a mycobacterium with high resistance to the usual antibiotics.
According to the review consulted, the case we present here seems to be the first lung disease caused by M. lentiflavum to be described in Spain in a patient who was an immunocompetent patient and had no previous medical history of respiratory disease. It is very often difficult to determine the clinical significance of the isolates due to this mycobacterium. It is, nevertheless, a microorganism that needs to be taken into account and not be systematically considered as a contaminant, even in patients with no associated comorbidity.
Conflicts of interestAll the authors declare that they have no conflicts of interest directly or indirectly related to the contents of the manuscript.
Please cite this article as: Matesanz-López C, Loras-Gallego C, Cacho-Calvo JB, Río-Ramírez MT. Mycobacterium lentiflavum. Infección pulmonar en una paciente inmunocompetente. Enferm Infecc Microbiol Clin. 2020;38:347–348.