We report a case of a 27-year-old man without relevant medical history. He was born in Costa Rica and was at that moment visiting Barcelona. He presented to the emergency department with a 3-day history of fever, headache and polyarthralgia. On clinical exam hepatosplenomegaly, jaundice and fever (39°C) were documented. He referred a negative HIV serology performed 6 months before in his country, and reported sex with other men.
Initial laboratory test revealed altered liver parameters. Total bilirubin was 6.5mg/dL (predominantly conjugated), aspartate aminotransferase 885IU/L, alanine aminotransferase 2847IU/L, alkaline phosphatase 238IU/L, gamma-glutamyl transferase 864IU/L and prothrombin time 67%.
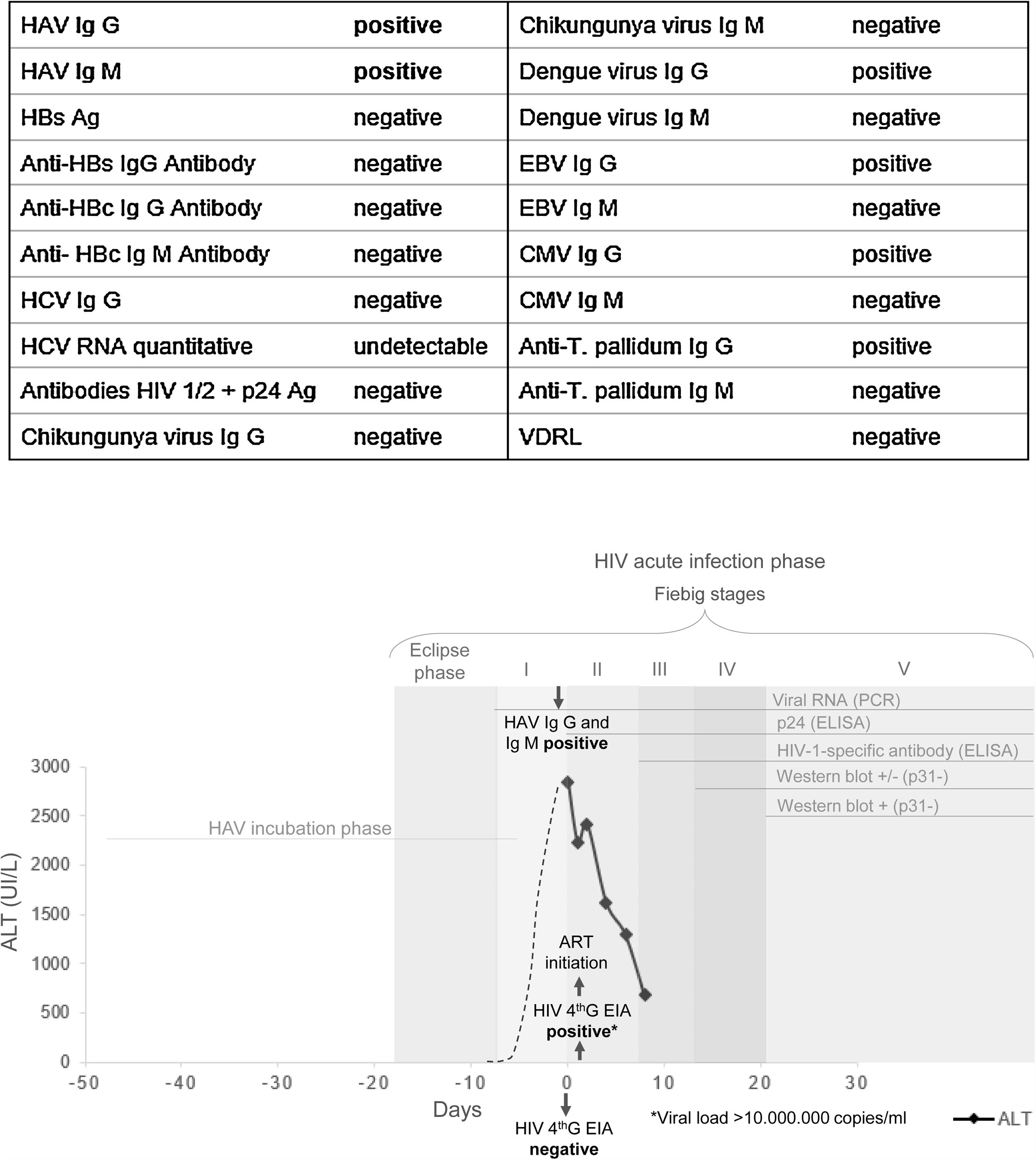
According to geographical origin of the patient, laboratory results and clinical presentation, primary hepatotropic viruses serologies (HAV, HBV, HCV, HDV, HEV) and viral load, EBV, CMV, dengue, chikungunya, syphilis serologies and HIV 1/2 4th generation EIA were requested (Fig. 1A). Acute hepatitis A infection was diagnosed, also with serological evidence to previous exposure to dengue, syphilis, CMV and EBV.
Re-exploring the patient 24h later, polyadenopathies and rash were identified, unnoticed the day before. HIV-1 viral load was then requested, being >10,000,000copies/ml and CD4+ T cells count was 224/mm3 (17%). Retrospectively repeated EIA from that day resulted now positive, only 24h later than the previously negative. Concomitant acute hepatitis A and severe acute primary HIV infection (PHI) were then the final diagnoses. TDF/FTC/dolutegravir at usual doses were immediately started with rapid remission of symptoms and liver tests progressive improvement over the following weeks. Virological, immunological and biochemical markers are shown in Fig. 1B.
A week later the patient's partner, a 65-year-old Spanish man, presented at hospital, reporting their last sexual intercourse being 18 days before. He had HIV negative test 2 years ago and was asymptomatic at that moment. HIV RNA, IgM and IgG HAV were requested. HAV vaccine/immune globulin was indicated depending on the results, but he decided to perform laboratory tests in another hospital. A week later he returned to the emergency department with fever and altered liver parameters. IgG and IgM HAV were positive confirming acute hepatitis A, HIV-1 viral load was undetectable, excluding HIV-1 infection.
DiscussionPHI can co-exist with other sexually transmitted infections (such as HAV) thus health professionals should be aware and always suspect them. PHI clinical symptoms may be non-specific and results of diagnostic tests rapidly modify, as in the current case, in 24h. Sexual intercourse during PHI is associated to high transmission risk due to uncontrolled viral replication and extremely high HIV viral load in this phase, with frequent unawareness of infection.
About 20% of diagnosis in Spain and other European countries are made during acute infection (detection of p24 Ag and/or HIV-RNA in absence of HIV antibody) or during recent infection (HIV antibody detection up to 6 months after infection).1–3 Immediate ART initiation controls symptoms, minimize viral reservoirs and decrease transmissibility.4
Hepatitis A is an acute, self-limiting disease transmitted by faecal–oral route through contaminated food or water or through person-to-person contact, including sexual contact. If sexual transmission of HAV is suspected, particularly among men-who-have-sex-with-men (MSM), PHI should be excluded. PHI presents clinically as a mononucleosis-like or flu-like syndrome, easily missed in the context of a concomitant acute hepatitis. HAV incubation period could potentially be shorter than serological evidence of HIV infection. HIV RNA become positive 7–10 days after HIV exposure, p24-antigen approximately 14 days and HIV antibodies at around 21 days.5 Thus, if concomitant or near exposure to HAV and HIV are suspected, HIV RNA should be requested to exclude PHI. HIV-VL is frequently extremely high in this period, with increased transmission risk. Complete seroconversion to HIV takes approximately 3 months until last WB band become positive (usually p31 band).
Sexually transmitted outbreaks of acute hepatitis A have been reported in the last years in Europe among MSM, particularly HIV-positive.6–9 Hepatitis A infection is not more severe among HIV-infected individuals, but HAV viraemia is higher and longer, increasing transmission risk. In high-income countries anti-HAV IgG in general population is usually low (<50% by the age of 30 years).10 Therefore, when HAV is introduced in groups at particular high-risk, as MSM population, outbreaks may occur, stressing the importance of preventive measures, particularly vaccination. As for HBV and HCV, HAV must also be considered as a potential co-infection in the context of PHI.
Conflict of interestJA has received research funding from Gilead Sc and ViiV Healthcare, out of the current work.
NAD: none to declare.