Mycobacterium mageritense is a non-pigmented rapidly growing microorganism identified as a new species in the year 1997 in Madrid, Spain.1 Since 2002, there are several published papers of clinical infections caused by M. mageritense (e.g., sinusitis, pneumonia, skin and soft tissue infections, and catheter-related bacteraemia).2–6 Different antimicrobials (doxicicline, ciprofloxacine, amykacine, imipenem, linezolid and trimethoprim/sulfamethoxazole) have been used for the treatment of these infections. We report here our experience with an immune-competent patient diagnosed of M. mageritense meningitis likely associated to an intrathecal catheter.
In July 2008, a 39-year-old woman was admitted at her reference hospital because of fever. She was carrier of an intrathecal catheter (with a reservoir for epidural analgesia); also, she was taking several psychotropic drugs because of posttraumatic back pain and left radiculopathy (following a car crash). There was a purulent discharge in the reservoir area. Therefore, both the epidural catheter and the reservoir were removed. Microbial cultures (three set of blood, the exudates and the catheter tip) were all negative. An empirical combination of intravenous (IV) vancomycin and gentamicin was prescribed during 14days. There was total resolution of fever and the patient was discharged from her reference hospital.
Twenty days later (August 2008), she developed a new fever (38.5°C), headache and somnolence, and the back pain increased significantly. She was remitted to our hospital. The cerebrospinal fluid (CSF) study showed a count of 246leukocyte/μL (60% of mononuclear's cells), 33mg/dL of glucose, 155mg/dL of protein, and the adenosinedeaminase (ADA) was 29U/L (normal range: <9U/L). CSF usual stains, bacterial cultures and LCR serology (VDRL, Brucella sp., Listeria monocytogenes, Coxiella burnetii, Leptospira sp., and Borrelia sp.) were all negative. A Mantoux test was negative. Chest X-ray was within normal limits. Empirical treatment with rifampin, isoniazid, pyrazinamide and ethambutol in standard doses was prescribed. Twelve days after, the patient developed a sudden facio-braquio-crural hemiplegy. NMR study showed several ischaemic infarcts (at the protuberance and right intern capsule). The first CSF culture in Löwenstein medium (August 2008) was positive for a mycobacterium. The isolate was sent to the National Reference Laboratory for Mycobacteria and identified by phenotypic methods as colonies non-pigmented after 3days of incubation at 22, 30, 37 and 42°C, negative for Tween Hydrolysis and heat-stable catalase test, positive for arylsulfatase activity at 3days, and for nitrate reductase. Furthermore, it was identified as M. mageritense by PCR-RFLP of hsp65 gene.8 The strain showed three fragments (240, 130 and 85bp) by BstEII restriction enzyme digestion and three fragments (145, 120 and 60bp) by HaeIII restriction enzyme digestion. In addition, the identification was confirmed by sequencing of 16S rRNA gene. Susceptibility testing was made by the proportions method (on Agar 7H10) that showed resistance to isoniazide, streptomycin, ethambutol, rifampicin, P.A.S., kanamycin, cycloserine and ethionamide. Pirazinamide susceptibility on MGIT 960 was made following the manufacturer recommendations. The susceptibility to other drugs (amikacin, norfloxacin, ofloxacin, ciprofloxacin, imipenen, linezolid, trimetil-sulfametoxazol, capreomycin, doxiciclin, claritromycin, amoxicillin-clavulanic and tobramycin) was made by E-TEST (on Mueller-Hinton agar).
The initial antitubercular therapy was changed to linezolid (600mg/12h), doxicicline (100mg/12h), and moxifloxacin (400mg/12h) all by IV route. There was a good clinical response but the patient developed nausea and vomiting. Linezolid was switched to oral cothrimoxazole (one strength tablet BID) because of a probable interaction with psychotropic drugs,9 and vomiting ceased completely. A new CSF study was normal. Nowadays, after 1year of continuous antimicrobial therapy and nearly 4years after the clinical diagnosis of meningitis, the patient is in a good state of health with a left hemiplegy as neurological sequel.
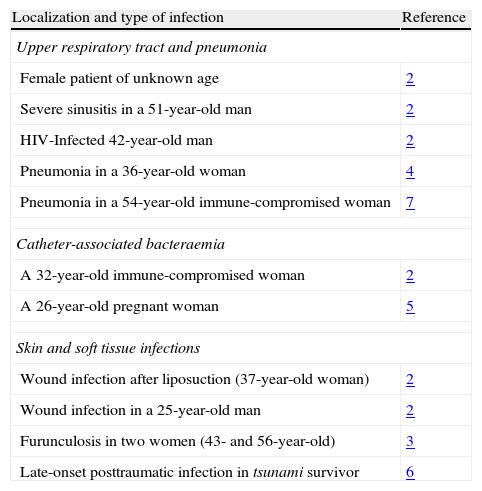
This rare case of meningitis widens the still small spectrum of M. mageritense infections.2–6 The most likely way of entry of the mycobacterium in this patient could be through the intrathecal catheter. M. mageritense is a ubiquitous bacterium. It can be carried on freshwater and seawater.3,6 It has been recovered from respiratory secretions, blood, wound infections, and some catheters.2,4,7 In addition, it is able to form biofilms that can provide resistance to several antimicrobials, but the clinical importance of this fact is not well defined10 (Table 1).
Mycobacterium mageritense infections.
| Localization and type of infection | Reference |
| Upper respiratory tract and pneumonia | |
| Female patient of unknown age | 2 |
| Severe sinusitis in a 51-year-old man | 2 |
| HIV-Infected 42-year-old man | 2 |
| Pneumonia in a 36-year-old woman | 4 |
| Pneumonia in a 54-year-old immune-compromised woman | 7 |
| Catheter-associated bacteraemia | |
| A 32-year-old immune-compromised woman | 2 |
| A 26-year-old pregnant woman | 5 |
| Skin and soft tissue infections | |
| Wound infection after liposuction (37-year-old woman) | 2 |
| Wound infection in a 25-year-old man | 2 |
| Furunculosis in two women (43- and 56-year-old) | 3 |
| Late-onset posttraumatic infection in tsunami survivor | 6 |
Regarding the clinical course of our patient, she developed a sudden facio-braquio-crural hemiplegy. In our opinion, this neurological manifestation was probably due to cerebral vasculitis. The relationship between mycobacterial meningeal infections and cerebral ischaemic lesions is well known.
In conclusion, acute meningitis opens the narrow clinical spectrum of M. mageritense infections. Also, iatrogenic meningitis is frequently secondary to contamination of aerosolized bacteria from environment (e.g., the mouth of medical staff).11 In this regard, it is necessary to bear in mind the real probability of environmental infections, whatever the origin, in the carriers of catheters.