A 67-year-old male patient with chronic ulcerative colitis on treatment with mesalazine and recently diagnosed biphasic synovial sarcoma of the mediastinum, was admitted to the hospital with acute bloody diarrhea. He had not received any treatment for the sarcoma. Colonoscopy and biopsies revealed cytomegalovirus colitis. Intravenous ganciclovir was administered and then changed to oral valganciclovir with improvement.
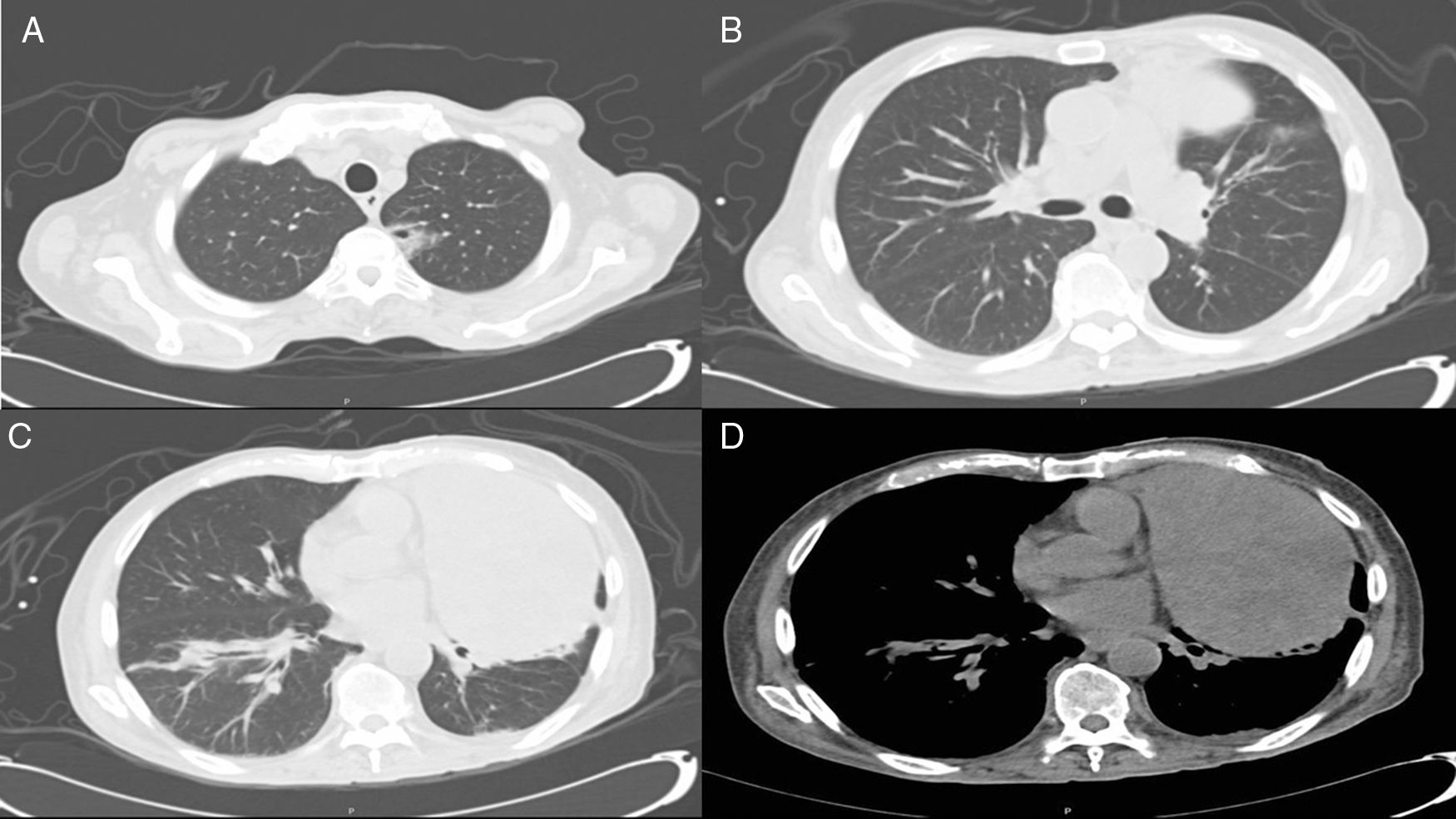
Two weeks later, the patient presented with fever, rhinorrhea and developed a necrotic lesion inside the right nostril (Fig. 1). On physical examination, there was a necrotic lesion within the right nostril, left nasal induration and bilateral basal rales. Laboratory testing revealed the presence of neutropenia (514cells/mm3). CT scan of the chest showed a left apical cavitated lesion, a right basal pneumonic infiltrate and the previously known tumor (Fig. 2).
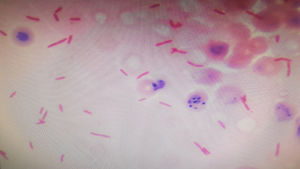
Diagnosis and evolutionA swab test and biopsy of the nasal lesion were performed showing gram negative rods in palisades. That culture grew Pseudomonas aeruginosa (PAE), which also was isolated from blood (Fig. 3), bronchoalveolar lavage and pleural fluid cultures. The histopathological report showed extensive necrotic tissue and non-specific inflammatory infiltrate.
The final diagnosis was disseminated infection by PAE with necrotizing pneumonia and nasal ecthyma gangrenosum. Treatment with meropenem was immediately started and colistin was added after susceptibility testing showed multirrestistant PAE. The patient developed septic shock requiring vassopresors, refused to receive mechanical ventilation and died.
Final commentP. aeruginosa bacteremia is a serious condition with mortality as high as 60% when associated with septic shock. Risk factors for disseminated infection by PAE include immunosuppression, malignant neoplasms, previous use of broad spectrum antibiotics, and long hospital stay. In this case, the patient presented with moderate neutropenia which was probably caused by valganciclovir, and worsened by sepsis.
Cutaneous manifestations caused by PAE are broad and may include folliculitis, onicholysis, cellulitis, conjunctivitis, cutaneous nodules and necrotic lesions also known as echtyma gangrenosum.1–3 Ecthyma gangrenosum is considered a cutaneous manifestation of sepsis secondary to PAE, and it is present in 1.3–6% of the cases. The most characteristic location is the perianal and gluteus area, along with the lower limbs (>85% of reported cases).2,4–6 Nasal ecthyma gangrenosum reports account for <1% of the cases and according to our search, there are only four cases previously described.1,4–7 Because of the location of the lesion the differential diagnosis was a fungal infection such as mucormycosis, aspergillosis and fusariosis. Other entities which appearance may resemble echtyma are malignant neoplasms (lymphoma, sarcoma), bacterial infections caused by S. aureus and other gram-negative bacilli, vasculitis, disseminated intravascular coagulation and septic emboli.1,3–6 Ecthyma gangrenosum secondary to PAE is uncommon and should be considered in the differential diagnosis of necrotic lesions in middle line.
Conflicts of interestThe authors declare no conflict of interest or have receive any sponsorship.