A 12-year-old male with no prior personal or family history of interest presented an intermittent fever having started 2 weeks earlier, with initial signs and symptoms of pharyngitis and tonsillitis with whitish exudate. He was treated with oral azithromycin (10mg/kg/day) for 5 days and then oral amoxicillin/clavulanic acid (50mg/kg/days) for 10 days due to persistent fever and pharyngeal exudate. After completing antibiotic therapy, the patient had a persistent low-grade fever and started to experience acute abdominal pain in the left hypochondrium. He had no associated vomiting or diarrhoea. He also reported significant weight loss in the last 2 weeks.
A physical examination revealed a small amount of residual whitish exudate in the left tonsil, with no significant lymphadenopathy, as well as pain on palpation in the left hypochondrium, with no signs of peritoneal irritation, hepatomegaly or splenomegaly. Otherwise, the examination was normal.
Laboratory testing in the emergency department revealed hypertransaminasaemia (GOT 58U/l, GPT 124U/l) and LDH 507U/l, with no increase in acute-phase reactants (CRP 2.4mg/l) and relative lymphocytosis. A peripheral blood smear showed numerous activated lymphocytes.
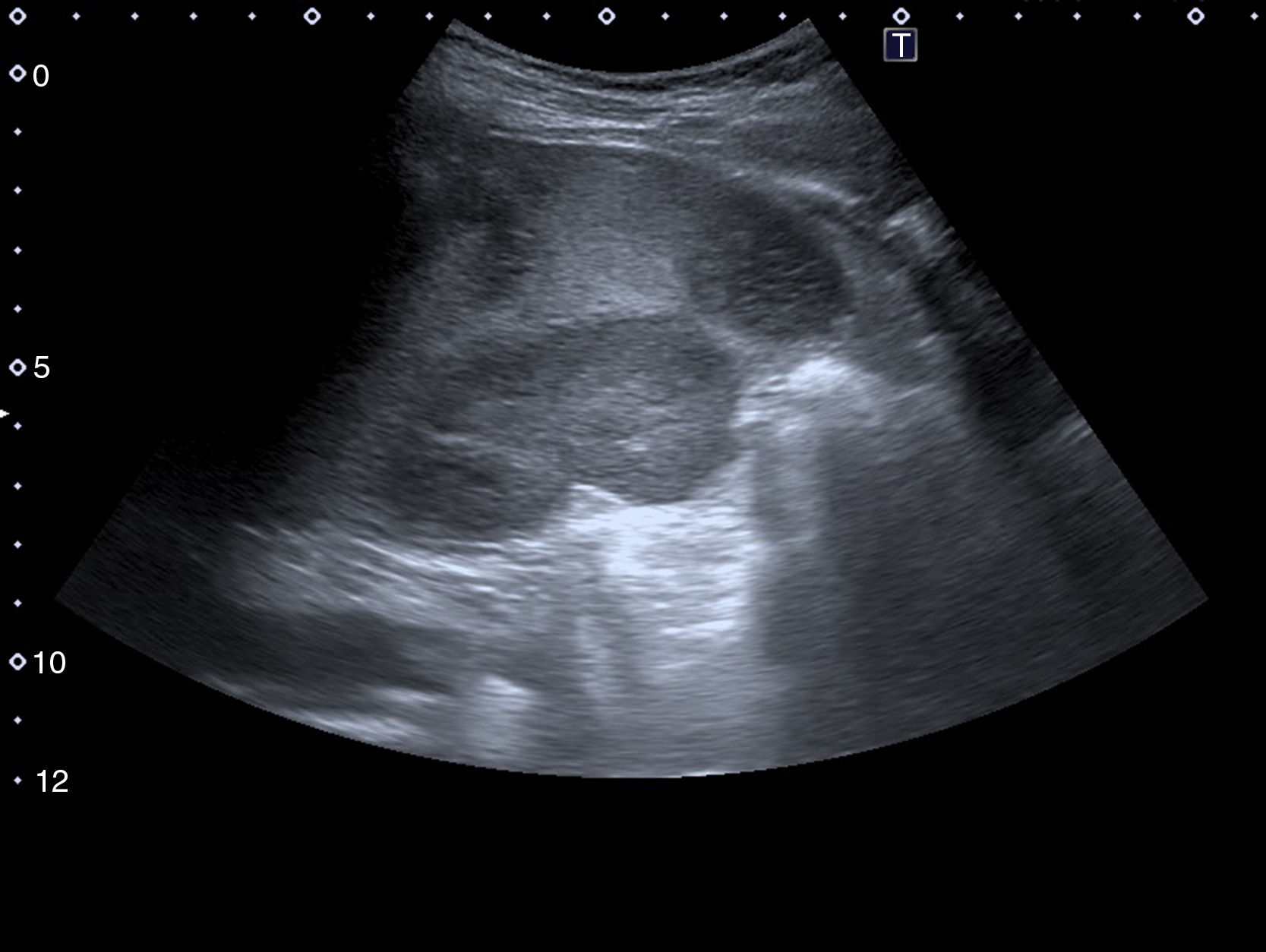
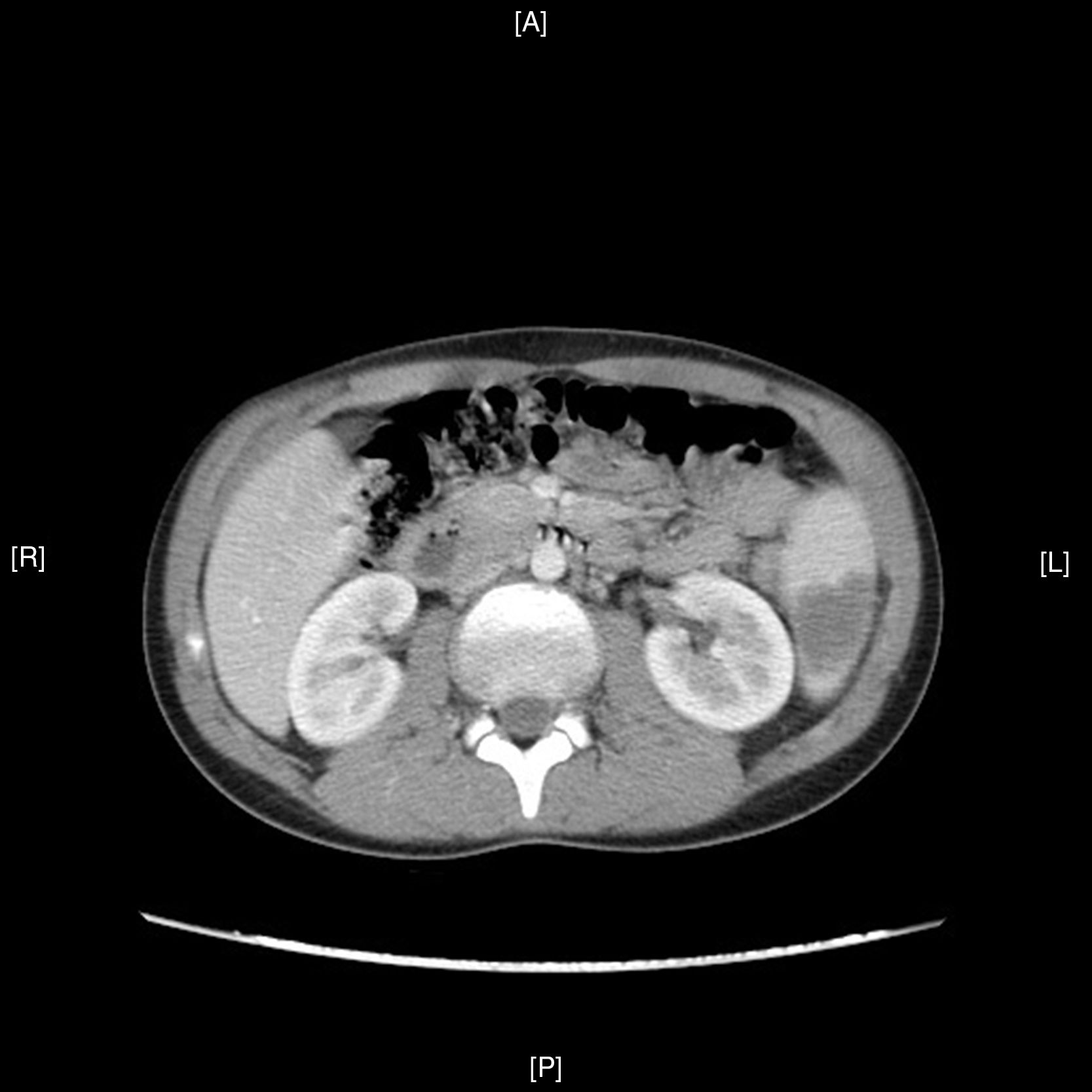
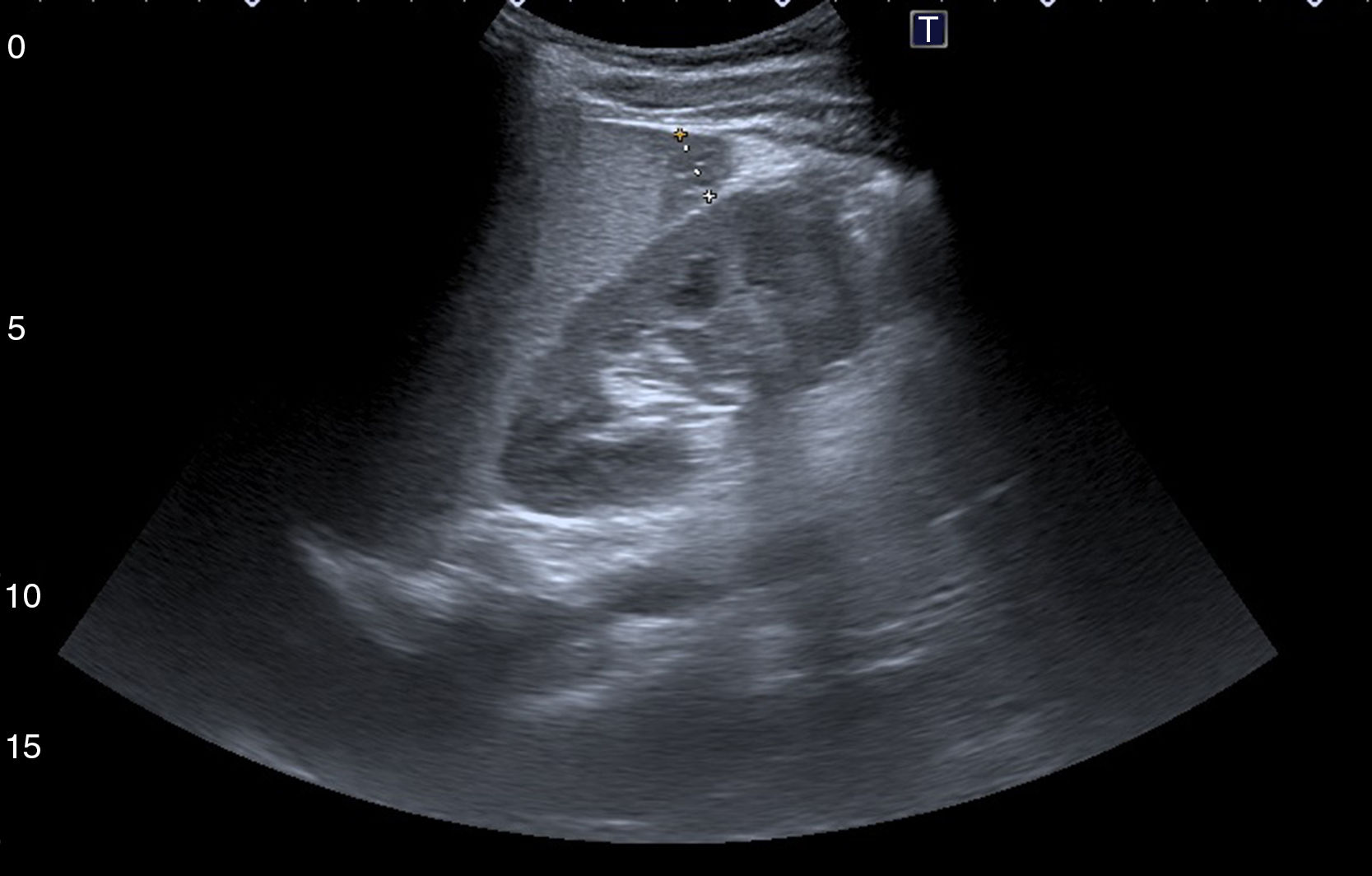
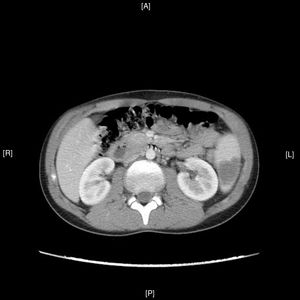
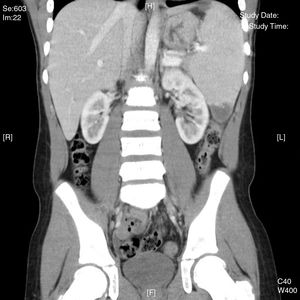
An abdominal ultrasound in the emergency department showed 5 hypodense images, with a wedge-shaped morphology on the periphery of the spleen, suggestive of splenic infarctions (Figs. 1 and 2). A CT scan confirmed the suspicion of splenic infarctions (Figs. 3 and 4), and the patient had to be hospitalised.
The patient was confirmed to have splenic lesions given the appearance of multiple hypodense images with a wedge-shaped morphology throughout the spleen, from the periphery to the splenic hilum, suggesting splenic infarctions as a leading possibility. Moderate splenomegaly (13cm×14.5cm).
Given the suspicion of splenic infarctions potentially secondary to a mononucleosis syndrome, it was decided to admit the patient to hospital.
Absolute rest was indicated. The patient was found to be haemodynamically stable and afebrile with improvement of his abdominal pain. Viral serologies came back positive for EBV capsid antigen IgM and IgG and negative for EBV nuclear antigen IgG, antibodies for HIV 1 and 2, and cytomegalovirus IgG and IgM.
The patient's transaminase level was seen to decrease to the point of normalisation. Ultrasound monitoring showed a decrease in the number and size of his splenic infarctions (Fig. 5). Subsequently, the patient followed a course of outpatient clinical and ultrasound monitoring until his lesions resolved.
DiscussionA prolonged fever that does not respond to antibiotic therapy plus pharyngeal and tonsillar exudate, hypertransaminasaemia, and relative lymphocytosis with activated lymphocytes mean that an infection is highly likely to be of viral origin.
Although the patient exhibited neither lymphadenopathy nor hepatosplenomegaly, these clinical findings are not present in all mononucleosis syndromes. The clinician must take into consideration a current epidemiological environment with many EBV infections in addition to the complementary tests performed prior to serology.
Splenic infarction caused by infectious mononucleosis due to EBV is a rare complication reported in adults and in paediatric patients. Its clinical presentation varies widely, from rupture due to splenic infarctions with intense acute abdominal pain to sub-acute abdominal signs and symptoms.1–3 This complication seems to result from transient increases in hypercoagulability factors, which may be fostered by underlying diseases (malaria, sickle-cell anaemia or haemoglobinopathies)4–6 and sometimes presents in a context of concomitant infection (EBV, CMV or M. pneumoniae).7
It is important to recognise the value and dynamic of antibody production in EBV infection. EBV capsid antigen IgM may be present when signs and symptoms develop and disappear after a few weeks. EBV capsid antigen IgG appears 3–4 weeks later and remains present throughout the life of all patients. IgG anti-EBNA nuclear antigen usually appears a month after symptoms develop, normally persists throughout life and rules out an acute EBV infection.8
In immunocompetent patients, a serology with these 3 antibodies would suffice to interpret the status of the infection. Our patient had an acute EBV infection demonstrated in the third week of his signs and symptoms.
Abdominal ultrasound is a test to assess acute abdominal pain in a patient with infectious mononucleosis and demonstrate splenic disease (organomegaly, infarctions, rupture, etc.), as well as to perform subsequent follow-up.9 There is no specific treatment for this complication apart from splenectomy in an unstable patient. Treatment for splenic infarctions is conservative, with close observation and ultrasound monitoring showing gradual improvement.10
Please cite this article as: García-Vázquez J, Plácido Paias R, Portillo Márquez M. Infarto esplénico debido a una infección común. Enferm Infecc Microbiol Clin. 2018;36:593–595.