Assessing the role of HIV and non-HIV related factors is essential for a better understanding of the neurocognitive outcomes in perinatally HIV-infected (PHIV+) young people. The aim of our study was to assess cognition and quality of life (QoL) of a PHIV+ cohort of young people and to compare it with a control group.
MethodsThirty PHIV+ and 30 HIV(−) healthy young adults matched by age, sex and socioeconomic status completed a protocol that included neurocognitive tests, a psychosocial semi-structured interview and a QoL questionnaire (PedsQL). Neurocognitive domain-specific and domain-general (NPZ-5) Z-scores were calculated. CDC AIDS-defining category C or not C (PHIV+/C, PHIV+/noC) was considered to evaluate differences within the PHIV+ group. Univariate and multivariate analysis were performed.
ResultsSixty patients were included; 67% were female; median age (IQR) 19 years (18–21). Regarding PHIV+ young people, 27% showed CDC C category (none encephalopathy), 93% were on ART and 77% had undetectable viral load. No differences regarding occupation were found, although the HIV(−) group repeated less grades (p=0.028) and had a higher education level (p=0.021).
No differences were found between PHIV+/noC and HIV(−) participants. However, the PHIV+/C group showed poorer performance than PHIV+/noC (NPZ-5, p=0.037) and HIV(−) subjects (crystallised intelligence, p=0.025; intelligence quotient, p=0.016). Higher nadir CD4+ T-cell count was related to better Z-score in memory (p=0.007) and NPZ-5 (p=0.025). Earlier and longer exposure to ART resulted in better performance in memory (p=0.004) and executive functions (p=0.015), respectively.
ConclusionsNo significant differences were found in the neurocognitive profile nor QoL between PHIV+/noC and HIV(−) adolescents; however, PHIV+/C participants obtained lower scores. The use of longer and earlier ART seems to have a beneficial effect.
Para estudiar el perfil neurocognitivo de jóvenes infectados perinatalmente por VIH (PVIH+) es importante valorar tanto los factores asociados al virus como los no relacionados. El objetivo de nuestro estudio fue evaluar la cognición y la calidad de vida de una cohorte de jóvenes PVIH+ y compararlas con las de un grupo control.
MétodosTreinta jóvenes PVIH+ y 30 sujetos sanos VIH− pareados por edad, sexo y nivel socioeconómico completaron un protocolo que incluía pruebas neurocognitivas, entrevista psicosocial semiestructurada y cuestionario de calidad de vida PedsQL. Se calculó el Z-score global (NPZ-5) y específico para cada dominio neurocognitivo. Adicionalmente, se consideró la categoría SIDA (PVIH+/C, PVIH+/noC). Se realizó análisis univariante y multivariante.
ResultadosDe los 60 pacientes incluidos, el 67% eran mujeres; edad media (IQR) 19años (18-21). Respecto al grupo PVIH+, el 27% tenían categoría CDCC (ninguna encefalopatía), el 93% tomaban antirretrovirales y el 77% tenían carga viral indetectable. No hubo diferencias en cuanto a ocupación, aunque el grupo VIH− repitió menos cursos académicos (p=0,028) y tuvo mayor nivel educativo (p=0,021).
No hubo diferencias entre los grupos PVIH+/noC y VIH−. El grupo PVIH+/C tuvo un rendimiento inferior al de PVIH+/noC (NPZ-5, p=0,037) y VIH− (inteligencia cristalizada, p=0,025; cociente de inteligencia, p=0,016). Mayor nadir de célulasT CD4+ se relacionó con mejor Z-score en Memoria (p=0,007) y NPZ-5 (p=0,025). La exposición temprana y prolongada a la terapia antirretroviral favoreció un mejor rendimiento en Memoria (p=0,004) y en Funciones Ejecutivas (p=0,015), respectivamente.
ConclusionesNo hubo diferencias significativas en el perfil neurocognitivo ni en calidad de vida entre los adolescentes PVIH+/noC y VIH−; sin embargo, los participantes PVIH+/C obtuvieron puntuaciones más bajas. La exposición temprana y prolongada a la terapia antirretroviral parece tener un efecto beneficioso.
Even though the HIV mother-to-child transmission rate has decreased dramatically, in 2018 160,000 children (<15 years) were infected with HIV worldwide,1 resulting in early and continuous exposure to the effects of the virus in the developing brain of infants and children making them a highly vulnerable population.2
Neurocognitive deficits are increasingly being assessed. Several studies have shown global and specific cognitive impairments in perinatally HIV-infected (PHIV+) patients even after the introduction of combination antiretroviral therapy (cART),3,4 while in others the performance was within normal ranges.5,6 The cognitive effects of PHIV infection may be difficult to assess since the populations included in these studies had heterogeneous sociodemographic, cultural and immunovirological characteristics. This assessment is further complicated by the lack of consensus among researchers on the neuropsychological instruments used and the absence of well-matched control groups. Aspects like having a biological parent as caregiver, higher household income or caregiver's cognitive functioning have been related to better cognitive outcomes in PHIV+ children.7,8 Attention and executive processes are among the most prevalent findings even when the patients are clinically stable.4,6,9,10 On the other hand, the literature commonly shows varying degrees of neurocognitive impairment that seems to be positively influenced by initiation of cART and virus suppression.9,11–13
Other clinical variable that needs to be taken into consideration is the category C diagnosis (CDC AIDS-defining, PHIV+/C compared to PHIV+/noC). Several studies have shown lower cognitive performance specifically for the PHIV+/C patients.7,9,14,15 These found differences are frequently attributable to a prior diagnosis of encephalopathy in some studies.7,9
The purpose of this study was to assess the neurocognitive profile and health-related quality of life (HRQoL) in a cohort of PHIV+ youths, considering factors related to the infection and their social-environmental context in order to better address medical, neurocognitive and psychosocial cares in PHIV+ children.
Materials and methodsParticipants and proceduresNeuroCoRISpeS is an ongoing prospective study with the objective of evaluating the psychosocial, psychopathological, neurocognitive and neuroimaging profile of PHIV+ pediatric patients. In this cross-sectional case-control study, 97 patients who belonged to 7 major hospitals in Spain included in the national pediatric cohort (CoRISpeS) were invited to participate during their follow-up visits. Each participant completed a standard protocol that included neurocognitive and psychosocial variables as well as HRQoL measures. PHIV+ participants between 16 and 23 years old were selected and matched with not exposed HIV negative (HIV−) subjects by range of age, sex and socioeconomic status (SES). The whole process of recruiting and assessing both patients and their matched control group was accomplished between May 2012 and August 2017. We chose parental education as indicator of SES since it has been linked with cognitive functioning.16 Patients with encephalopathy were excluded (no other neurological diagnoses were present). Information about use/abuse of drugs was collected but exposure was not an exclusion criteria. Data related to HIV infection were obtained from clinical records, and self-reported adherence to antiretroviral therapy (ART) was defined as good when ≥95% of doses were taken. ART included both combination of >2 antiretrovirals as well as mono/bi-therapies, as some of our patients were born before the introduction of cART.
Ethical approval was obtained from the Ethics Committee of every participant Hospital. Informed consent and assent were obtained from parents and children <18 years old. For those participants aged ≥18 informed consent was requested.
Instruments/neurocognitive assessmentA sociodemographic and psychosocial semi-structured questionnaire was created for this project in order to collect data on: age, sex, ethnicity, country of origin, to have experienced the death of one or both parents, family structure, occupation, years of education, completed secondary education, number of repeated grades, caregiver's education level, and lifestyle habits (use of drugs and exercise).
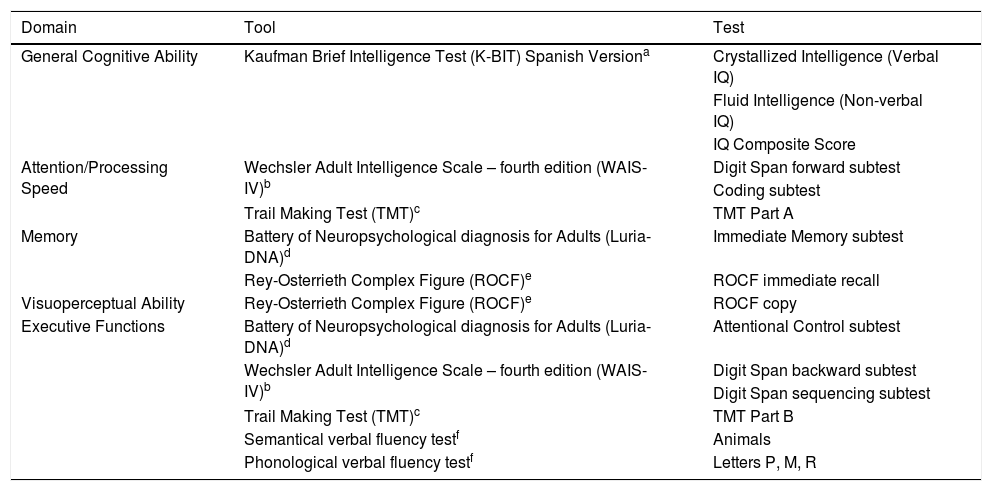
For the neurocognitive assessment, several tests were used to evaluate five cognitive domains (Table 1).
Neurocognitive assessment battery.
| Domain | Tool | Test |
|---|---|---|
| General Cognitive Ability | Kaufman Brief Intelligence Test (K-BIT) Spanish Versiona | Crystallized Intelligence (Verbal IQ) |
| Fluid Intelligence (Non-verbal IQ) | ||
| IQ Composite Score | ||
| Attention/Processing Speed | Wechsler Adult Intelligence Scale – fourth edition (WAIS-IV)b | Digit Span forward subtest |
| Coding subtest | ||
| Trail Making Test (TMT)c | TMT Part A | |
| Memory | Battery of Neuropsychological diagnosis for Adults (Luria-DNA)d | Immediate Memory subtest |
| Rey-Osterrieth Complex Figure (ROCF)e | ROCF immediate recall | |
| Visuoperceptual Ability | Rey-Osterrieth Complex Figure (ROCF)e | ROCF copy |
| Executive Functions | Battery of Neuropsychological diagnosis for Adults (Luria-DNA)d | Attentional Control subtest |
| Wechsler Adult Intelligence Scale – fourth edition (WAIS-IV)b | Digit Span backward subtest | |
| Digit Span sequencing subtest | ||
| Trail Making Test (TMT)c | TMT Part B | |
| Semantical verbal fluency testf | Animals | |
| Phonological verbal fluency testf | Letters P, M, R |
Note: IQ: Intelligence quotient.
Kaufman A, Kaufman N. K-BIT Test Breve de Inteligencia [K-BIT. Kaufman Brief Intelligence Test]. Madrid: TEA; 1997.
WAIS: Wechsler D. WAIS-IV. Escala de inteligencia de Wechsler para adultos-IV. Madrid: NCS Pearson, Inc; 2012.
Tamayo F, Casals-Coll M, Sánchez-Benavides G, et al. [Spanish normative studies in a young adult population (NEURONORMA young adults Project): norms for the verbal span, visuospatial span, Letter-Number Sequencing, Trail Making Test and Symbol Digit Modalities Test]. Neurologia. 2012 Jul–Aug; 27(6):319–29. doi:10.1016/j.nrl.2011.12.020.
Luria-DNA: Manga D, Ramos F. Luria-DNA (Batería Luria de diagnóstico neuropsicológico de adultos). Madrid: TEA; 2000.
PedsQL TM 4.0-Spanish version was used to assess HRQoL. It has been widely used in PHIV+ patients, obtaining adequate reliability and validity indexes in this population.17,18 The PedsQL assess HRQoL for ages 2–18 years, although it was extended above this age to allow the same assessment measure across participants. The Total Scale range from 0 to 100, with higher scores indicating better HRQoL. It comprises several scales: Physical, Emotional, Social, and School Functioning. Additionally, a Psychosocial Health Summary Score is calculated (mean score on the Emotional, Social, and School Functioning subscales).
Statistical analysisDomain-specific and overall (NPZ-5) Z-scores were calculated for PHIV+ group (CDC C category was specifically considered to assess if differences existed) using the HIV(−) mean and standard deviation (SD) according to their age: 17–18 or ≥19 years. Previously we checked that healthy group Z-scores were similar to normative data (Z-scores range: −0.39 to 0.32). Z-score indicates how many SD below or above the reference group mean a patient's score is. After that, Z-scores were averaged to obtain the mean of each domain. NPZ-5 score was calculated as the mean Z-score across all domains. Cognitive impairment was considered if Z-score was ≤−1 in ≥2 domains, following Frascati criteria.19
Results were expressed by median and interquartile ranges (IQR) or means and SD for quantitative variables, and by frequencies and percentage for qualitative variables. To compare categorical variables Pearson Chi-Square or Fisher exact tests were used, whereas quantitative variables were compared using Student t or Mann–Whitney U tests, as appropriate. Spearman's rank correlation was used to determine the strength and direction between quantitative variables. Multivariate linear regression was used to estimate the effects of HIV-related variables on Memory domain and NPZ-5. Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS v.24, Chicago, IL, USA).
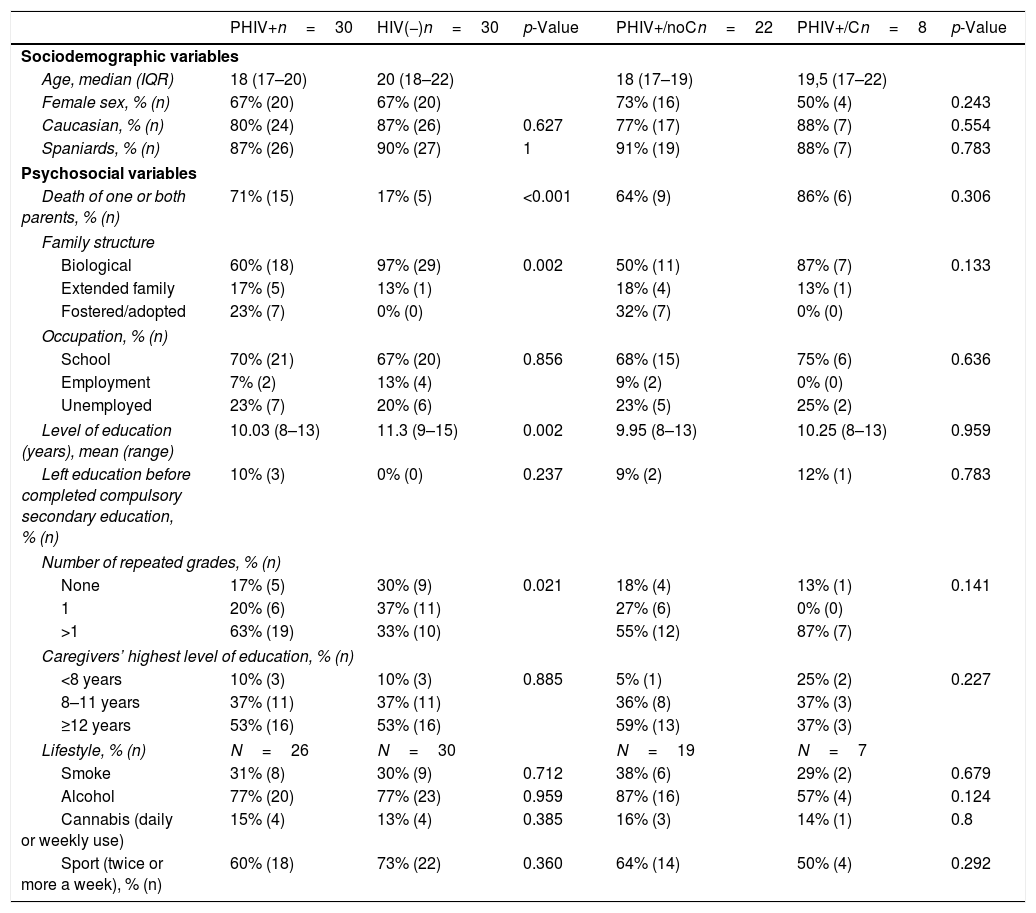
ResultsParticipant characteristicsA total of 30 PHIV+ and 30 HIV(−) participants agreed to participate. Table 2 presents sociodemographic and psychosocial characteristics. The median age was 19 years (IQR: 18–21), most were Caucasian and 67% were female. Sociodemographic characteristics were similar in both groups. Regarding PHIV+ youths, 71% of them had experienced the death of at least one of their biological parents, compared with 17% of HIV(−) participants (p<0.001), and 40% of them were raised by their extended family or in fostercare, unlike 3% of HIV(−) group (p=0.002). There were no differences regarding occupation, but HIV(−) participants repeated less grades (p=0.028) and accessed higher education (p=0.021) than PHIV+ patients. About their lifestyle habits, there were no differences between both groups.
Sociodemographic and psychosocial characteristics.
| PHIV+n=30 | HIV(−)n=30 | p-Value | PHIV+/noCn=22 | PHIV+/Cn=8 | p-Value | |
|---|---|---|---|---|---|---|
| Sociodemographic variables | ||||||
| Age, median (IQR) | 18 (17–20) | 20 (18–22) | 18 (17–19) | 19,5 (17–22) | ||
| Female sex, % (n) | 67% (20) | 67% (20) | 73% (16) | 50% (4) | 0.243 | |
| Caucasian, % (n) | 80% (24) | 87% (26) | 0.627 | 77% (17) | 88% (7) | 0.554 |
| Spaniards, % (n) | 87% (26) | 90% (27) | 1 | 91% (19) | 88% (7) | 0.783 |
| Psychosocial variables | ||||||
| Death of one or both parents, % (n) | 71% (15) | 17% (5) | <0.001 | 64% (9) | 86% (6) | 0.306 |
| Family structure | ||||||
| Biological | 60% (18) | 97% (29) | 0.002 | 50% (11) | 87% (7) | 0.133 |
| Extended family | 17% (5) | 13% (1) | 18% (4) | 13% (1) | ||
| Fostered/adopted | 23% (7) | 0% (0) | 32% (7) | 0% (0) | ||
| Occupation, % (n) | ||||||
| School | 70% (21) | 67% (20) | 0.856 | 68% (15) | 75% (6) | 0.636 |
| Employment | 7% (2) | 13% (4) | 9% (2) | 0% (0) | ||
| Unemployed | 23% (7) | 20% (6) | 23% (5) | 25% (2) | ||
| Level of education (years), mean (range) | 10.03 (8–13) | 11.3 (9–15) | 0.002 | 9.95 (8–13) | 10.25 (8–13) | 0.959 |
| Left education before completed compulsory secondary education, % (n) | 10% (3) | 0% (0) | 0.237 | 9% (2) | 12% (1) | 0.783 |
| Number of repeated grades, % (n) | ||||||
| None | 17% (5) | 30% (9) | 0.021 | 18% (4) | 13% (1) | 0.141 |
| 1 | 20% (6) | 37% (11) | 27% (6) | 0% (0) | ||
| >1 | 63% (19) | 33% (10) | 55% (12) | 87% (7) | ||
| Caregivers’ highest level of education, % (n) | ||||||
| <8 years | 10% (3) | 10% (3) | 0.885 | 5% (1) | 25% (2) | 0.227 |
| 8–11 years | 37% (11) | 37% (11) | 36% (8) | 37% (3) | ||
| ≥12 years | 53% (16) | 53% (16) | 59% (13) | 37% (3) | ||
| Lifestyle, % (n) | N=26 | N=30 | N=19 | N=7 | ||
| Smoke | 31% (8) | 30% (9) | 0.712 | 38% (6) | 29% (2) | 0.679 |
| Alcohol | 77% (20) | 77% (23) | 0.959 | 87% (16) | 57% (4) | 0.124 |
| Cannabis (daily or weekly use) | 15% (4) | 13% (4) | 0.385 | 16% (3) | 14% (1) | 0.8 |
| Sport (twice or more a week), % (n) | 60% (18) | 73% (22) | 0.360 | 64% (14) | 50% (4) | 0.292 |
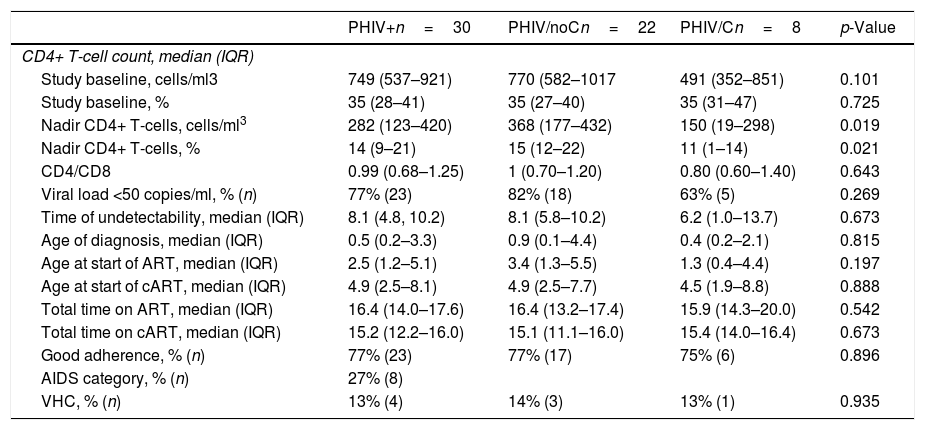
Concerning patients’ HIV-related markers, the majority showed good clinical and immunovirological status at the moment of assessment (Table 3). The median CD4+ T-cell percentage was 35% (28%–41%) while nadir CD4+ T-cell was 14% (9%–21%). Viral load was undetectable (<50 copies/ml) in 77% of the patients. Following the CDC classification, 27% of the patients were diagnosed as category C. With regard to HIV-related markers stratified by CDC C category, the only significant difference that was found was lower nadir CD4+ T-cell count (number and percentage) for the PHIV+/C group.
Clinical HIV-related markers.
| PHIV+n=30 | PHIV/noCn=22 | PHIV/Cn=8 | p-Value | |
|---|---|---|---|---|
| CD4+ T-cell count, median (IQR) | ||||
| Study baseline, cells/ml3 | 749 (537–921) | 770 (582–1017 | 491 (352–851) | 0.101 |
| Study baseline, % | 35 (28–41) | 35 (27–40) | 35 (31–47) | 0.725 |
| Nadir CD4+ T-cells, cells/ml3 | 282 (123–420) | 368 (177–432) | 150 (19–298) | 0.019 |
| Nadir CD4+ T-cells, % | 14 (9–21) | 15 (12–22) | 11 (1–14) | 0.021 |
| CD4/CD8 | 0.99 (0.68–1.25) | 1 (0.70–1.20) | 0.80 (0.60–1.40) | 0.643 |
| Viral load <50 copies/ml, % (n) | 77% (23) | 82% (18) | 63% (5) | 0.269 |
| Time of undetectability, median (IQR) | 8.1 (4.8, 10.2) | 8.1 (5.8–10.2) | 6.2 (1.0–13.7) | 0.673 |
| Age of diagnosis, median (IQR) | 0.5 (0.2–3.3) | 0.9 (0.1–4.4) | 0.4 (0.2–2.1) | 0.815 |
| Age at start of ART, median (IQR) | 2.5 (1.2–5.1) | 3.4 (1.3–5.5) | 1.3 (0.4–4.4) | 0.197 |
| Age at start of cART, median (IQR) | 4.9 (2.5–8.1) | 4.9 (2.5–7.7) | 4.5 (1.9–8.8) | 0.888 |
| Total time on ART, median (IQR) | 16.4 (14.0–17.6) | 16.4 (13.2–17.4) | 15.9 (14.3–20.0) | 0.542 |
| Total time on cART, median (IQR) | 15.2 (12.2–16.0) | 15.1 (11.1–16.0) | 15.4 (14.0–16.4) | 0.673 |
| Good adherence, % (n) | 77% (23) | 77% (17) | 75% (6) | 0.896 |
| AIDS category, % (n) | 27% (8) | |||
| VHC, % (n) | 13% (4) | 14% (3) | 13% (1) | 0.935 |
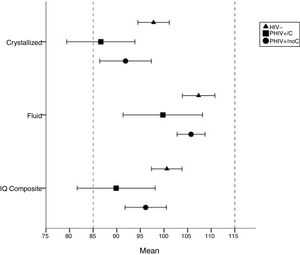
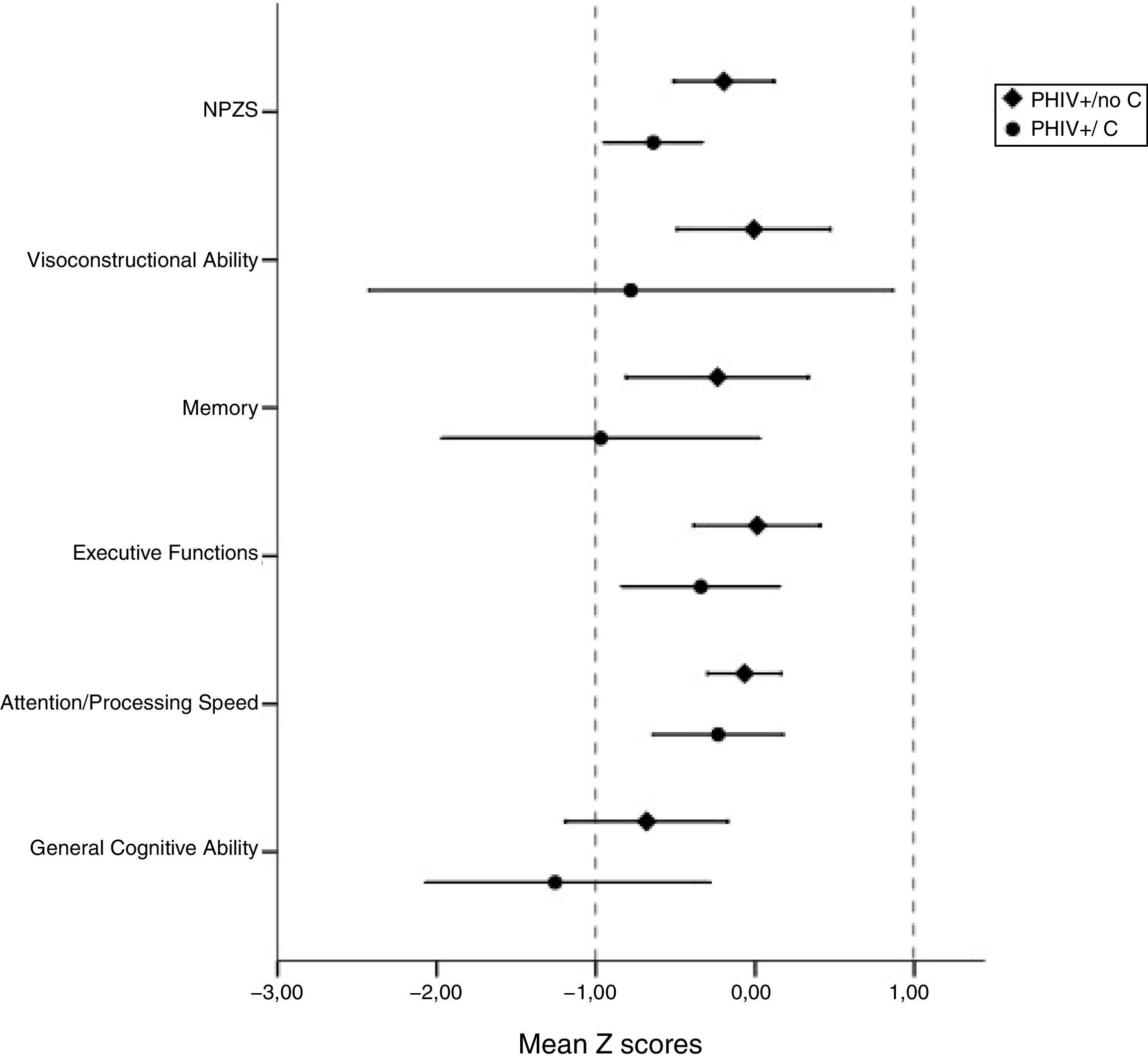
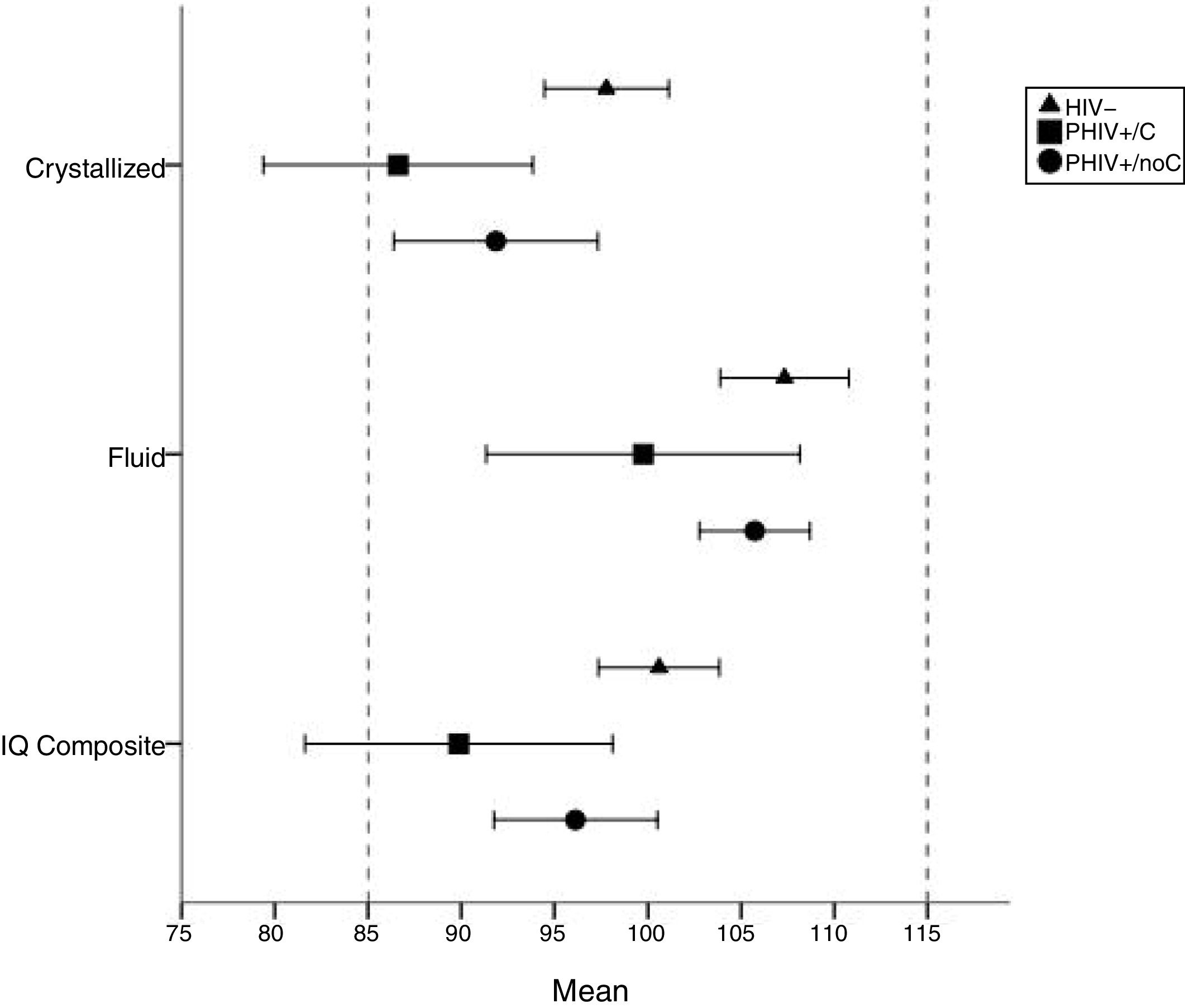
Figs. 1 and 2 present intellectual results and mean Z-scores for each cognitive domain and NPZ-5 by CDC status. Intellectual scores for both PHIV+ and HIV(−) groups were within reference mean (mean=100, SD=15), and there were no statistically significant differences between PHIV+/noC and HIV(−) participants. PHIV+/C participants had the lowest scores in all the 3 intellectual measures, and they specifically showed poorer performance than HIV(−) subjects in crystallized intelligence (mean [SD]: 87 [9], 98 [9] respectively; p=0.025) and intelligence quotient (IQ) (mean [SD]: 90 [10], 101 [9] respectively; p=0.016).
Neurocognitive mean Z-scores by domain in PHIV+/noC and PHIV+/C.
Note: Significant differences were found among PHIV+/C and PHIV+/noC: NPZ-5, mean Z-score [SD], −0.64 [0.34], −0.19 [0.64] respectively, p=0.037; Memory, mean Z-score [SD], −0.97 [1.08], −0.21 [1.18], respectively; p=0.067). Z-score indicates where the patient's score is compared to the HIV(−) group mean (how many standard deviations below or above the reference group mean). The results between −1 SD and +1 SD were considered normal.
KBIT crystallized and fluid intelligence and IQ composite standard scores by HIV status.
Note: All scales represent age-based standard scores (mean=100, SD=15). Crystallized intelligence is more affected by culture, education and experience, while fluid intelligence is related to the ability to think logically and solve problems in novel situations. From both of them, an overall composite score is calculated (IQ composite score). Significant differences were found among PHIV+/C vs. HIV(−): crystallized ability (mean difference: 11.175, p=0.025); IQ composite (mean difference: 10.725, p=0.016).
According to the cognitive domains results of PHIV+ patients, General Cognitive Ability (GCA) was the most affected, with almost 1 SD below the healthy group data (Z-score=−0.805). The remaining domains obtained Z-scores around zero (from −0.036 to −0.393).
NPZ-5 score reflected a general tendency to score significantly worse in PHIV+/C category than PHIV+/noC (mean Z-score [SD], −0.64 [0.34], −0.19 [0.64] respectively; p=0.037), similar to the findings in the Memory domain where we found a trend to worse performance in those patients (mean Z-score [SD], −0.97 [1.08], −0.21 [1.18], respectively; p=0.067).
Three (10%) of the HIV− participants were classified as cognitively impaired, compared to 7 (23%) of PHIV+ participants (p=0.171), but this percentage could not be explained by CDC status.
Associations of cognitive functioning with HIV-related and psychosocial variablesRegarding immunovirological variables, Memory domain and NPZ-5 were positively correlated to higher nadir CD4+ T-cells/mm3 (r=0.487, p=0.007; r=0.414, p=0.025; respectively) and negatively correlated to age at start of cART (r=−0.516, p=0.004; r=−0.331, p=0.079; respectively). Longer exposition to ART resulted in better performance in Executive Functions (r=0.446, p=0.015).
Regarding psychosocial variables, pursuing studies at the moment of the evaluation had a beneficial effect on Memory and NPZ-5 performance, showing better mean scores the patients who were studying compared to those who were neither studying or working (mean Z-score [SD], 0.12 [0.69], −1.50 [1.23], respectively; p=0.038 and −0.11 [0.53], −0.72 [0.42], respectively; p=0.023). Patients who had not repeated any grade showed better performance in GCA (p=0.051) and Executive Functions (p=0.018). On the other hand, patients who practiced exercise regularly revealed better Memory outcomes than those who did not (p=0.043). We did not find association between cognitive performance and use of alcohol or cannabis, primary language, to have experienced the death of one or both parents, type of family nucleus nor family maximum level of education.
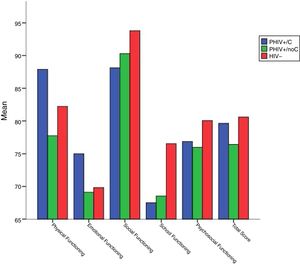
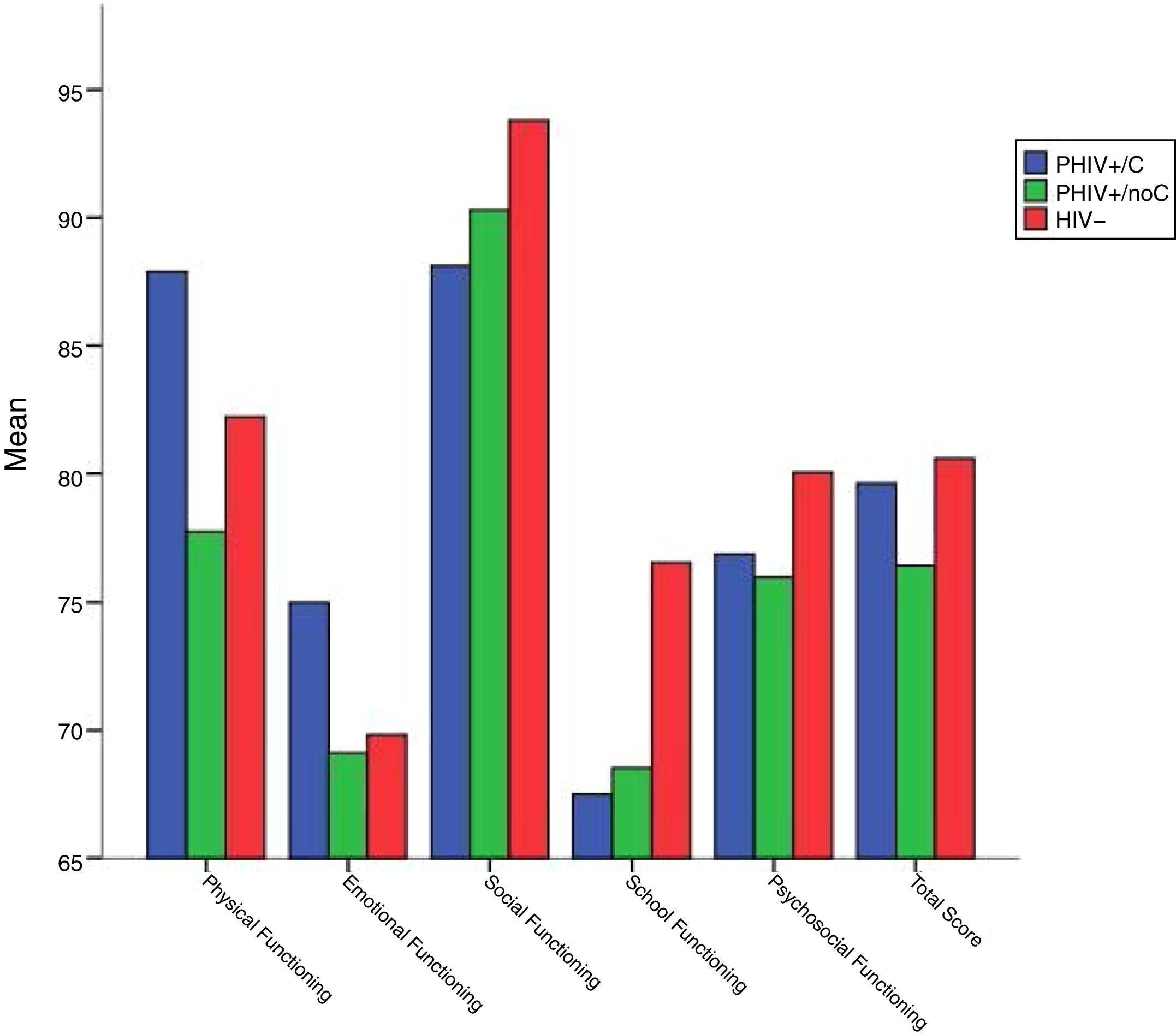
Health-related quality of life outcomes and its associations with HIV-related and psychosocial variablesAbout their HRQoL, there were no significant differences between patients and HIV(−) subjects on PedsQL scores, neither when having into account CDC C category (Fig. 3). Males scored higher in Physical functioning (92 vs. 76, p=0.004). Patients who started earlier on treatment had higher Social scale scores (r=−0.580, p=0.002), while School functioning was better in those who were older when they started on ART and at the time of assessment (age at start of ART: r=0.420, p=0.037; age at start of cART: r=0.583, p=0.002; age at assessment time: r=0.580, p=0.002).
Self-report PedsQL mean scores by HIV status.
Note: Higher mean scores indicate better HRQoL in that domain, in a range from 0 to 100. The Psychosocial Health Summary Score is computed as the sum of the Emotional, Social, and School Functioning Scales. No significant differences were found between groups (p>0.05) in any of the scales.
We adjusted variables that could be potentially affecting the statistically significant results found in Memory domain and NPZ-5. Nadir CD4+ T-cell count, CDC C category and to be studying at the moment of assessment were associated with NPZ-5 scores in univariable analysis but they did not in multivariable analysis (all p>0.05). On the other hand, Memory scores improved after adjustment of nadir CD4+ T-cell count and CDC C category when patients were studying at the moment of assessment (multivariable coefficient, 0.961; 95% confidence interval, 0.069–1.853; p=0.036), but its associations with nadir CD4+ T-cell and CDC C category were not statistically significant.
DiscussionThe goal of our article was to examine neurocognitive performance among PHIV+ patients compared with HIV-unexposed uninfected youths, and to explore its relationship with clinical, environmental and lifestyle HIV-related factors. In our study, PHIV+/noC participants and healthy subjects showed similar performance, scoring near the average for the normative data. Both groups did not present statistically significant differences, while PHIV+/C patients did in some cognitive domains. PHIV+ group obtained the poorest results in General Cognitive Ability, although it remained 1 SD below the healthy subject's mean, which is considered average scoring. In relation to the other domains and NPZ5, differences between HIV(−) participants and PHIV+ were non-significant. These results suggest that well-controlled PHIV+ individuals not only may show preserved intellectual capacity but also their neurocognitive general ability (measured through individual and overall neurocognitive domains). PHIV+/C participants showed the poorest performance in every domain, but specifically they scored low-average in crystallized intelligence – highly related with cultural learning –, while in fluid intelligence, related with abstract reasoning free from culture influence, were average. These findings also highlight the importance of the environment where the children are raised as a key aspect in the intellectual development of the patient.
Regarding the findings in PHIV/C patients, recently Judd et al.9 described similar outcomes in 296 PHIV+ adolescents and 97 HIV(−) peers, overall but among the HIV-infected adolescents, those PHIV+/C were the most cognitively affected. In addition, studies have found a relationship between the presence of a previous class C event, and an increased risk for impairment in neurocognitive functioning.7,15 These results, together with the fact that most of the CDC C events occur early in life and the relationship found between neurocognitive performance and ART, point out the importance of early initiation of ART to minimize disease severity and long-term sequels. Specifically, we found that Memory and NPZ-5 were positively influenced by not having CDC C category, higher nadir CD4+ T-cell count and an early start of cART. Being exposed more time to ART was also related to better scores in Executive Functions. On the contrary, although these patients were previously severely immunosuppressed and they have now a good immunovirologic situation, which is associated with improved overall health, still showed poorer neurocognitive performance. The main measured difference between PHIV+/C and PHIV+/noC groups was the level of nadir CD4+ T-cell. Literature has also shown an inverse association between nadir CD4+ T-cell count and neurocognitive impairment and it has recently been defined as a robust predictor in both cART and previous era.20–22 Interestingly in our study the effect of both variables was statistically non-significant after adjustment for educational status, which is encouraging as it might suggest a major bearing on environmental variables not related to the infection.
Previous research points out that Information Processing Speed and Executive Functions are especially vulnerable to the neurodevelopmental effects of HIV disease.6,7,9,23 Curiously, in our study these domains were the less affected even for the PHIV+/C subgroup. Although a possible explanation might be related with the recruitment of a specific control group carefully matched, another influencing factor could be the exclusion of patients with encephalopathy from the study, as it has been related with severe cognitive impairment.
Other independent risk factors evaluated were psychosocial, educational and lifestyle factors. Both physical and cognitive training showed a beneficial effect on mnesic performance, and more discretely better global scoring in those patients who were studying, consistent with the positive relation shown in previous studies.11 The other relationship found was that patients who had not repeated any grade had better performance in GCA and Executive Functions. Difficulties in school attainment in patients with PHIV+ infection have been well documented.17,24–26 Due to the cross-sectional nature of this study and the age of participants we cannot establish causal connection between educational attainment and neurocognitive performance, but we can hypothesize that educational attainment is more related to neurocognitive benefits for children, or that those kids who have improved daily cognitive function also show better outcomes in the school. Either way, these findings underline the importance of inquiring about neurocognitive and educational functioning in the outpatient's visits, specially in those who show CDC C category, in order to develop appropriate interventions to facilitate positive academic trajectories.
We did not find association between cognitive performance and primary language, parent death, type of familiar nucleus or familiar level of education. As parental education and living in an enriched environment have been linked with child development,16,27,28 this relationship was expected. On the other hand, we could not find any association between the use of alcohol and cannabis with any of the variables studied probably because we have few daily users in our cohort, in line with Alperen29 results, who did not find PHIV+ infection to be a risk factor for alcohol or marijuana use, while emotional or conduct problems and the use of these drugs in the home were related. It also could be related to response bias or the fact that face-to-face studies may often result in under-reporting.
About their HRQoL, there were no significant differences between patients and healthy subjects on PedsQL scores, even when considering CDC C category. In this regard, our results are inconsistent with recently published studies conducted on PHIV+ children,17,30 which could be related to our thorough SES-matching process, our smaller sample size or the different ages of the patients between studies. HRQoL was reasonably good in both PHIV+ and HIV(−) participants, showing the lowest scores for Emotional and School functioning in all 3 groups, similar to previous results found in HIV children and youths.17,30 We found some unexpected and contradictory results regarding the onset of ART (better functioning in Social scale but worse School functioning starting earlier on ART), which lead us to think that this specific QoL questionnaire might not be adequate for measuring this entity because some of our patients, who were already working at the moment of the assessment, were less influenced by the complexity of the school years.
This study presents some limitations. Firstly, our results belong to a cohort of individuals from a limited geographical region with specific socioeconomic characteristics, which could not be extrapolated to other groups. Secondly, the fact that a longitudinal follow up is needed and the relatively small sample size used, which, however, has allowed us to implement a sophisticated matching method (including ethnicity and SES), which remains a challenge in this field. Thirdly, the use of drugs data method collection could result in under-reporting. Fourthly, the limited magnitude of some of our findings due to most of the significant correlations found were low. Despite these limitations, the described findings respond to an exhaustive study performed in a primarily Caucasian cohort, in contrast to other studies whose patients are usually from Afro-American or black African origin, providing valuable data. Assessing the neurocognitive, educational and psychosocial profile as well as HRQoL of a cohort of PHIV+ youths has been successfully achieved, having into account both the influence of HIV-related variables and environmental aspects, and comparing their results with those of their well-matched HIV(−) peers.
In summary, we have not found differences in the neurocognitive profile between PHIV+/noC adolescents and their matched uninfected peers. PHIV+/C participants obtained the poorest scores representing mild impairment (near 1 SD below the mean). Remarkably, markers of HIV disease severity (nadir CD4+ T-cell and AIDS) were related to poorer cognitive function, while taking prolonged and earlier ART treatment had a beneficial effect. On the other hand, while there is still no differences between groups in HRQoL measures nor occupation, HIV infection has been related to poorer outcomes in school and lower level of education. Thus, our results suggest that youngsters with PHIV+, even those who come from the pre-cART era, can show an adequate neurocognitive functioning and quality of life when they are well-controlled.
Funding sourceThis work was supported by Fundación para la Investigación y Prevención de SIDA en España (FIPSE) [24691/07, 3608229/09, 240800/09, 361910/10 and 36-0910-1]; Red Temática de Investigación en SIDA (RED RIS) [RD16/0025/0017-ISCIII-FEDER, RD16/0025/0019-ISCIII-FEDER, RD16/0025/0024-ISCIII-FEDER and RIS_EPICLIN_07/2016); Instituto de Salud Carlos III [FIS 15/00694] which is co-funded by Fondo Europeo de Desarrollo Regional (FEDER): “Una manera de hacer Europa”; grant for Río Hortega specialized health care post-training contract [CM 16/0022] to BRS; and grant by Comunidad de Madrid and fondos FEDER (Ayudas para la contratación de ayudantes de Investigación y técnicos de laboratorio/Orden 2524/2016, de 1 de agosto, BOCM núm. 188, de 8 de agosto de 2016) to CV.
Financial disclosureAuthors declare have no financial relationships relevant to this article to disclose.
Conflict of interestAuthors declare have no potential conflicts of interest to disclose.
This study would not have been possible without the collaboration of all the patients and their families, medical and nursing staff, and data managers who have taken part in the project.






![Neurocognitive mean Z-scores by domain in PHIV+/noC and PHIV+/C. Note: Significant differences were found among PHIV+/C and PHIV+/noC: NPZ-5, mean Z-score [SD], −0.64 [0.34], −0.19 [0.64] respectively, p=0.037; Memory, mean Z-score [SD], −0.97 [1.08], −0.21 [1.18], respectively; p=0.067). Z-score indicates where the patient Neurocognitive mean Z-scores by domain in PHIV+/noC and PHIV+/C. Note: Significant differences were found among PHIV+/C and PHIV+/noC: NPZ-5, mean Z-score [SD], −0.64 [0.34], −0.19 [0.64] respectively, p=0.037; Memory, mean Z-score [SD], −0.97 [1.08], −0.21 [1.18], respectively; p=0.067). Z-score indicates where the patient](https://static.elsevier.es/multimedia/0213005X/0000003800000009/v1_202011061044/S0213005X20300057/v1_202011061044/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)