An outbreak of serogroup C meningococcal disease (MD) that involved employees from an oil refinery occurred in Paulínia, from March to June 2010, and spread to the community of Cosmópolis, both situated in São Paulo State, Brazil. The aim of this study was to describe the epidemiological and laboratory aspects, and the control measures that were implemented.
MethodsDescriptive and molecular epidemiological analysis was used to define the extent of the outbreak and the common risk factors among outbreak related cases. Vaccination initiative targeted the employees from the oil refinery and the community-based individuals.
ResultsA total of six outbreak-related cases of MD in the oil refinery and 12 cases in the city of Cosmópolis, São Paulo State occurred in a three-month period. All 18 MD cases were confirmed as serogroup C either by culture, real time polymerase chain reaction (RT-PCR), or counterimmunoelectrophoresis (CIE). The meningococcal isolates (n=15) had the phenotype C:23:P1.14-6 and showed close genetic relationship by pulsed field gel electrophoresis (PFGE). Multilocus sequence typing (MLST) characterization showed that the clones were ST 3780, ST-103 complex. The isolates were susceptible to the antibiotics tested. Vaccination was administered to 15,848 persons at the oil refinery and 18,571 persons of the community.
ConclusionsThe molecular characterization of the Neisseria meningitidis (N. meningitidis) strains, and the efficient investigation and the prompt measures implemented were essential for controlling the disease in the region.
De marzo a junio de 2010 se produjo un brote de enfermedad meningocócica (EM) del serogrupo C en una refinería de petróleo en la ciudad de Paulina, afectando a los empleados y a la comunidad de Cosmópolis, ambas ciudades situadas en el estado de Sao Paulo (Brasil). Los objetivos del estudio fueron describir los aspectos epidemiológicos y de laboratorio así como las medidas de control que se implementaron.
MétodosSe realizo un análisis epidemiológico descriptivo y molecular para definir la extensión de la epidemia y los factores de riesgo comunes entre los casos relacionados con el brote. Se utilizo vacuna para los empleados de la refinería de petróleo y sus contactos en la comunidad.
ResultadosUn total de seis casos fueron relacionados con el brote de EM en la refinería de petróleo y 12 casos en la ciudad de Cosmópolis, durante un período de tres meses. Dieciocho casos de EM fueron confirmados como del serogrupo C mediante cultivo, reacción en cadena de la polimerasa en tiempo real (RT-PCR) o contrainmunoelectroforesis (CIE). Las cepas de meningococo aisladas (n=15) presentaban el fenotipo C: 23: P1.14-6 y mostraron estrecha relación genética por PFGE. La caracterización de MLST demostró que las cepas eran ST 3780, complejo ST-103 y eran susceptibles a los antibióticos probados. La vacunación se administró a 15.848 personas en la refinería y a 18.571 personas de la comunidad.
ConclusionesLa caracterización molecular de las cepas de N. meningitidis, la investigación eficaz y rápida y las medidas implementadas fueron esenciales para controlar la enfermedad en la región.
MD is still a major public health concern, and occurs either in endemic or in epidemic forms all over the world.1 Most cases in industrialized countries are sporadic and the attack rates are highest in infants from 3 months to 1 year old.1,2 Other factors favoring illness include: crowed places, lower socioeconomic households, poor ventilation, poor nutrition and more virulent strains.1,2
Brazil has experienced several epidemic waves of MD over the decades, with a predominance of serogroups A, B and C, in different periods.3–5 Following a period of 18 years (1987–2005) of predominance of serogroup B, Brazil began to realize a change in the epidemiology of MD, with a decline of serogroup B and increase of cases caused by serogroup C in several regions of the country.5,6
Currently approximately 75% of all MD in Brazil is caused by N. meningitidis strains belonging to clone of the ST-103 complex serosubtyped as C:23:P1.14-6 (personal communication). Outbreaks of serogroup C MD have been reported in several Brazilian cities.7–9 During the period from 2000 to 2009, most MD cases have occurred sporadically with annual rates from 1.5 to 2.5 across Brazil and 3.0 to 4.4 per 100,000 inhabitants in São Paulo State.10,11
An outbreak of MD occurred in an oil refinery in Paulínia and in the community of Cosmópolis, both located near Campinas, in São Paulo State, Brazil. This study aimed to describe the epidemiological and laboratory aspects, including the molecular analysis, as well as the control measures that were implemented.
MethodsA descriptive study reporting a N. meningitidis C outbreak in an oil refinery and in an adjacent community was conducted. The outbreak investigation, the disease control measures, the outbreak's social impact and the N. meningitidis molecular characterization are described.
Case definitionIn Brazil, practitioners, public health units and hospitals have a statutory obligation to notify any suspected case of meningitis. Laboratories also have the obligation to notify any isolates of N. meningitidis from a normally sterile site. A clinical case of MD is defined as: (i) for children over 1 year and adults – fever, severe headache, vomiting, stiff neck, signs of meningeal irritation, seizures or red spots on the body; (ii) for children under 1-year-old – signals of irritability, persistent crying and a bulging fontanelle.12 Criteria for a confirmed case are: (i) isolation of N. meningitidis from blood, cerebrospinal fluid (CSF) or skin lesion or (ii) detection of N. meningitidis antigen in blood or CSF or (iii) detection of intracellular Gram-negative diplococci or (iv) detection of meningococcal DNA by RT-PCR.12 All MD cases as well as their close contacts are investigated and receive chemoprophylaxis, as stated in the guide to epidemiological surveillance of the Brazilian healthy ministry.12
SettingsThe city of Paulínia has a population of 85,000 inhabitants and activities of fuel industries dominate in the city, among them oil refinery.
The oil refinery where the MD outbreak occurred had, at that time, its own employees and temporary workers with a total number of 17,590 employees (men and women, from 18 to 43 years old).
The city of Cosmópolis, that borders northern Paulínia, has a population of 59,319 inhabitants. This city is near the oil refinery and almost all the temporary workers were living there.
Laboratory analysisMD cases were confirmed at the Adolfo Lutz Institute, the National Reference Laboratory for Bacterial Meningitis. Cases were confirmed by isolation of N. meningitidis, using conventional microbiologic methods and the serogroup was determined by slide agglutination with specific polyclonal antibodies.13,14 In specimens found to have no viable bacteria, detection of serogroup specific meningococcal polysaccharide antigen was carried out by CIE or detection of meningococcal DNA by RT-PCR in blood or CSF.15,16
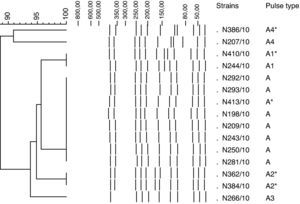
Pulsed field gel electrophoresisAll N. meningitidis isolates were typed by PFGE using NheI restriction enzyme as described elsewhere.17 Restriction profiles were analyzed using the Bionumerics software, version 4.0 (Applied Maths, St-Martens-Latem, Belgium). The isolates showing similarity >85% were considered genetically related, i.e. belonging to the same clone. The isolates considered to be related were tabulated by using the same capital letter and numbers if the isolates were non-identical but closely related.18,19
Serological typingSerotyping for all isolates was performed by dot-blotting using whole cell suspensions as previously described.20 The serotyping was performed with a set of 18 PorB and 15 PorA murine MAbs specific for the variable regions.5
Multilocus sequence typingMLST, using the Multi Locus Sequence Typing Website (http://neisseria.org/nm/typing/mlst) to assign alleles and sequence types, was also performed for all isolates according to the methods of Maiden et al.21
Antimicrobial susceptibility testingAll isolates were tested for susceptibility to penicillin, ampicillin, ceftriaxone, ciprofloxacin, chloramphenicol and rifampin using the broth microdilution procedure described in CLSI document M7-A8.22 The susceptibility/resistance breakpoints were those recommended by the CLSI document M100-S21.23
Data analysisThe descriptive analyses were performed using the Epi-Info software version 6.04d.
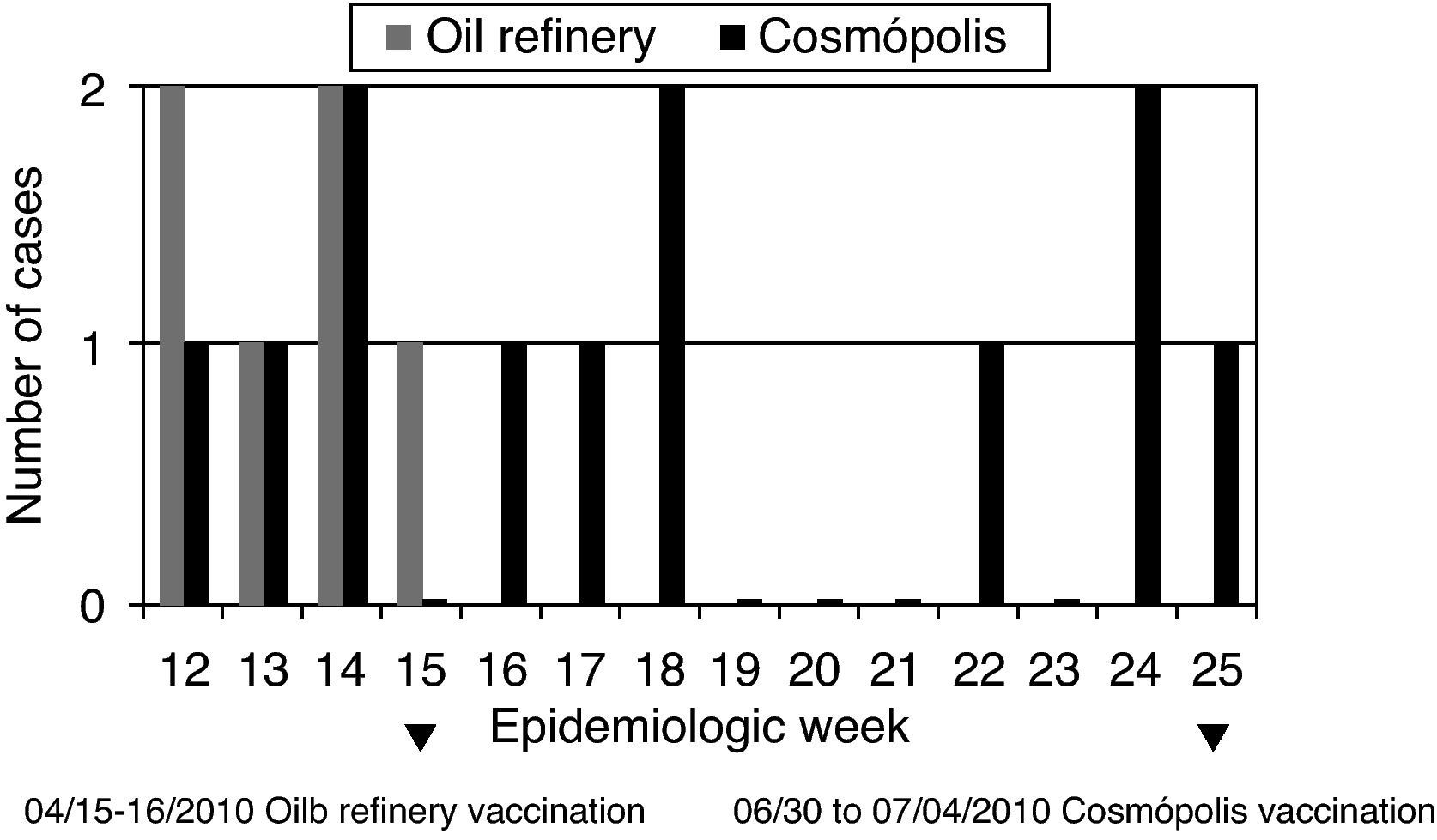
ResultsOil refinery outbreakOn 29 March 2010, the Paulínia epidemiological surveillance received the notification of three adults admitted to a local hospital with MD over a 3-day period. The Paulínia epidemiological surveillance considered this report an unusual cluster since the epidemiologic investigation revealed that 2 cases had a common point of exposure, a local oil refinery and the third one was son from an employee of the oil refinery. A supplementary epidemiologic investigation was implemented. From 01 to 11 April 2010 a total of six cases of MD in male workers from the oil refinery occurred over a 3-week period (Table 1 and Fig. 1). All cases were serogroup C, with two deaths (mortality 33%). Three out of six cases resided in Paulínia, one case lived in Mogi Mirim and two in Cosmópolis, cities of the micro-region of Campinas. The cases occurred in patients aged from 20 to 43 years old.
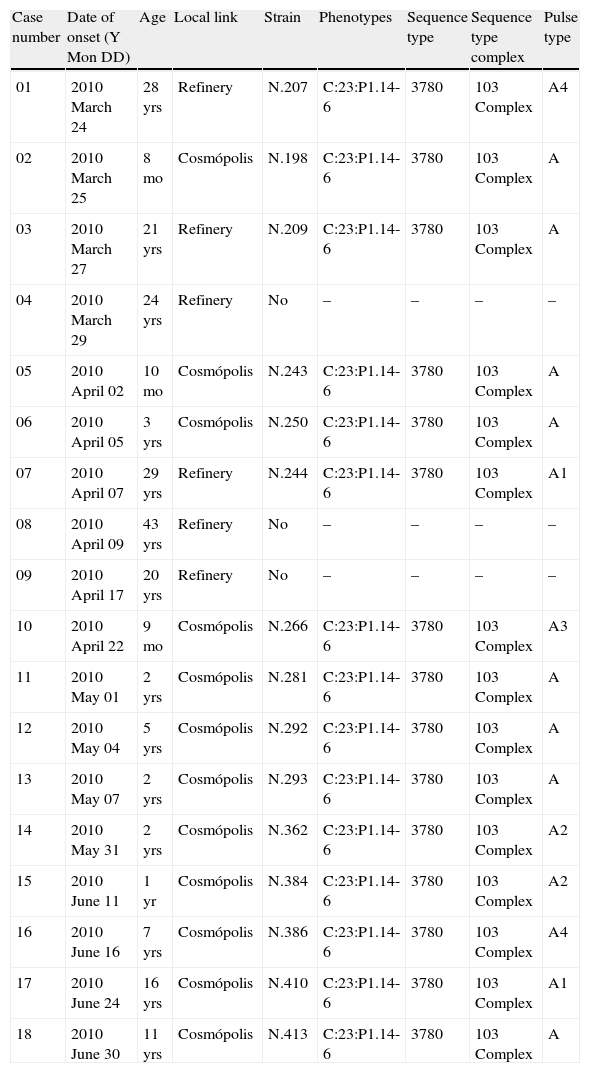
Summary of cases from meningococcal disease outbreak from the oil refinery and the Cosmópolis community and, the characterization of Neisseria meningitidis strains recovered from the patients.
| Case number | Date of onset (Y Mon DD) | Age | Local link | Strain | Phenotypes | Sequence type | Sequence type complex | Pulse type |
| 01 | 2010 March 24 | 28 yrs | Refinery | N.207 | C:23:P1.14-6 | 3780 | 103 Complex | A4 |
| 02 | 2010 March 25 | 8 mo | Cosmópolis | N.198 | C:23:P1.14-6 | 3780 | 103 Complex | A |
| 03 | 2010 March 27 | 21 yrs | Refinery | N.209 | C:23:P1.14-6 | 3780 | 103 Complex | A |
| 04 | 2010 March 29 | 24 yrs | Refinery | No | – | – | – | – |
| 05 | 2010 April 02 | 10 mo | Cosmópolis | N.243 | C:23:P1.14-6 | 3780 | 103 Complex | A |
| 06 | 2010 April 05 | 3 yrs | Cosmópolis | N.250 | C:23:P1.14-6 | 3780 | 103 Complex | A |
| 07 | 2010 April 07 | 29 yrs | Refinery | N.244 | C:23:P1.14-6 | 3780 | 103 Complex | A1 |
| 08 | 2010 April 09 | 43 yrs | Refinery | No | – | – | – | – |
| 09 | 2010 April 17 | 20 yrs | Refinery | No | – | – | – | – |
| 10 | 2010 April 22 | 9 mo | Cosmópolis | N.266 | C:23:P1.14-6 | 3780 | 103 Complex | A3 |
| 11 | 2010 May 01 | 2 yrs | Cosmópolis | N.281 | C:23:P1.14-6 | 3780 | 103 Complex | A |
| 12 | 2010 May 04 | 5 yrs | Cosmópolis | N.292 | C:23:P1.14-6 | 3780 | 103 Complex | A |
| 13 | 2010 May 07 | 2 yrs | Cosmópolis | N.293 | C:23:P1.14-6 | 3780 | 103 Complex | A |
| 14 | 2010 May 31 | 2 yrs | Cosmópolis | N.362 | C:23:P1.14-6 | 3780 | 103 Complex | A2 |
| 15 | 2010 June 11 | 1 yr | Cosmópolis | N.384 | C:23:P1.14-6 | 3780 | 103 Complex | A2 |
| 16 | 2010 June 16 | 7 yrs | Cosmópolis | N.386 | C:23:P1.14-6 | 3780 | 103 Complex | A4 |
| 17 | 2010 June 24 | 16 yrs | Cosmópolis | N.410 | C:23:P1.14-6 | 3780 | 103 Complex | A1 |
| 18 | 2010 June 30 | 11 yrs | Cosmópolis | N.413 | C:23:P1.14-6 | 3780 | 103 Complex | A |
The oil refinery had began in February the so-called “the stop”, in which a given area (a boiler at that time) is closed for maintenance. During “the stop” temporary workers are received from diverse cities, and even coming from other states. The temporary workers are hired by subcontractors. The number of employees at that moment was as follows: 16,415 temporary workers, 1175 own employees with a total of 17,590 workers, most of them were involved in the boiler maintenance. The MD cases occurred after the increase in the number of the temporary workers, thus local epidemiological surveillance considered the oil refinery a crowded condition and this fact could be a predisposing factor for meningococcal infection.
The oil refinery is organized into several departments and teams of workers. All the six MD cases worked in different departments and teams. A complete epidemiological investigation was performed and no evidence of contact between the cases was found, and thus the cases could not be characterized as secondary cases.
Chemoprophylaxis with rifampin was administered to all close contacts of cases. The recommendation that chemoprophylaxis may be expanded in the event of an outbreak led the central epidemiological health authority (CVE) to provide rifampin to all employees that had face-to-face contact with the cases. Chemoprophylaxis was provided to over 80 employees.
The central, regional and local epidemiological health authorities reported an outbreak of MD in the refinery with a coefficient of incidence of 34.1 per 100,000 persons and indicated the vaccination according to the recommendations stated in the epidemiological surveillance guidelines.12,24,25
On 15 and 16 April, the local epidemiological surveillance implemented the vaccination for all the oil refinery employees with meningococcal AC polysaccharide vaccine.
Following the outbreakActive surveillance for new cases of MD was implemented by frequent contact with the local area health facilities. MD incidence in the refinery declined after the vaccination. However, notifications of MD cases increased in Cosmópolis, a city near the oil refinery where almost all the temporary workers were living.
From March to June 2010, a total of 12 cases of MD serogroup C were notified among relatives of the oil refinery employees living in Cosmópolis, although these employees were not close contacts from the cases that occurred in the refinery (Table 1 and Fig. 1).
The coefficient of incidence in Cosmópolis at that time was 20.2 per 100,000 inhabitants and the cases occurred in patients aged from 8 months to 16 years-old. Prior to the outbreak the MD coefficient of incidence in Cosmóplis used to vary from 1.7 to 3.4 per 100,000 inhabitants. The increased number of cases in a short period led the epidemiological authorities to vaccinate Cosmópolis inhabitants from 2 months to 19 years old.
On 30 June and over a 5-day period, 18,571 inhabitants of Cosmópolis were offered the conjugate meningococcal or the meningococcal AC polysaccharide vaccine, according to the age, with immunization coverage of 90.9%. The phases of the vaccination program included: (1) elementary school students; (2) preschool children; (3) high school students; children and teens out of school and (4) a “catch-up” at a local basic health unit for people who had missed the previous vaccination days.
After the vaccination the MD incidence in Cosmópolis declined and the outbreak was regarded as controlled.
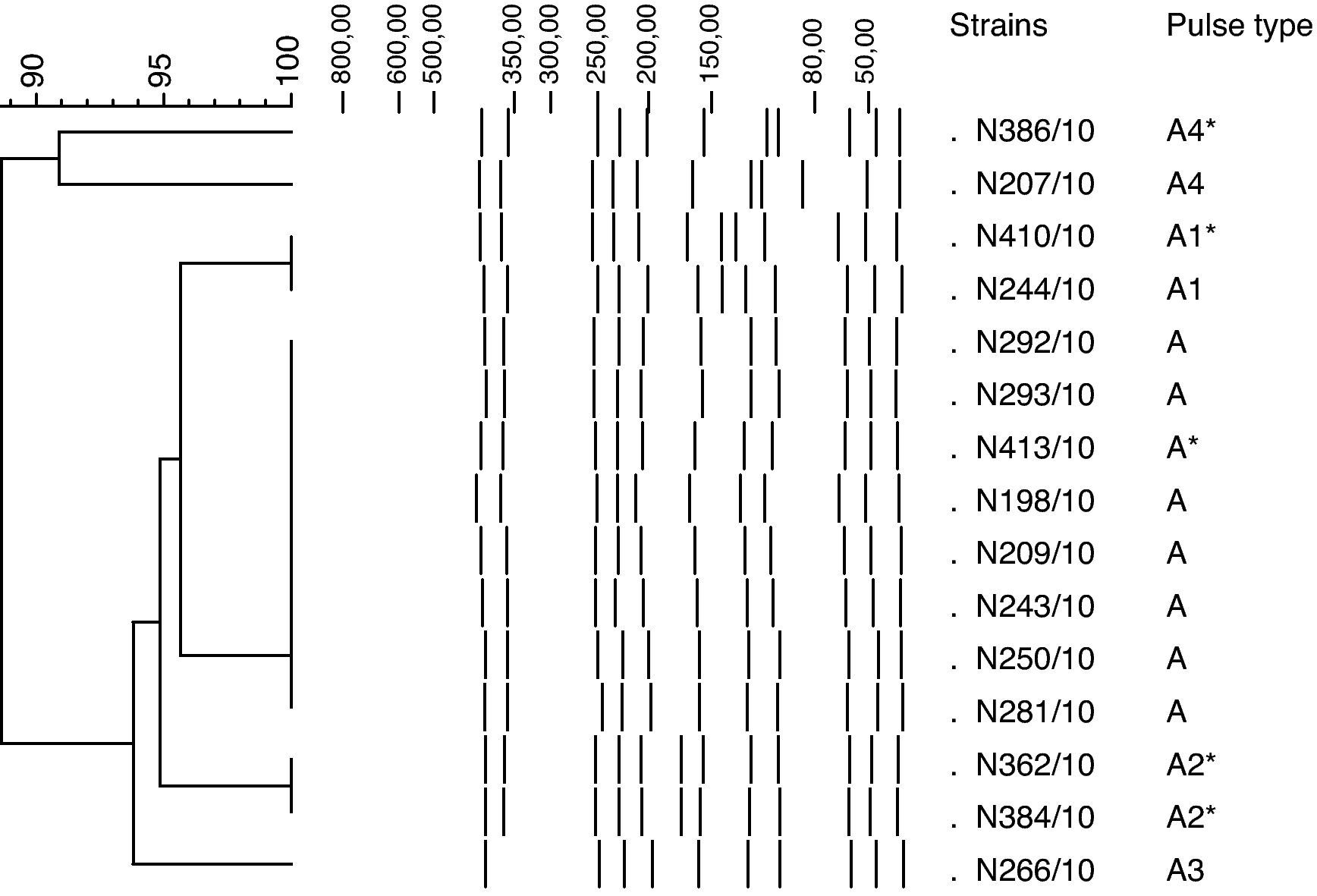
Laboratory investigationEighteen MD cases were confirmed as serogroup C either by culture, RT-PCR, or CIE. N. meningitidis serogroup C was isolated from blood in six patients and from CSF in nine patients of which 3 were oil refinery workers and, 12 were from the relatives of the oil refinery employees living in Cosmópolis. Two cases were confirmed only by RT-PCR and one was confirmed only by CIE. Overall, among the 15 isolates collected during the investigation, 10 had PFGE patterns that were indistinguishable (eight isolates) or related each other at >95% (two isolates), being designated as A and A1, respectively. Two of the 15 isolates PFGE patterns were related to the predominant PFGE pattern (A) at 94% (A2) and one of them, at 93% (A3) relatedness level. Two isolates displayed PFGE patterns (A4) with 89% of genetic homology with isolates PFGE pattern A. All the isolates were genetically associated, displaying 89–100% relatedness level (Fig. 2).
All the 15 isolates were indistinguishable by MLST analysis belonging to the ST-103 complex displaying the ST-3780 and the C:23:P1.14-6 phenotype (Table 1). Antimicrobial susceptibility patterns from the cases were identical and the isolates were susceptible to all antibiotics tested.
DiscussionCrowded conditions have been demonstrated to be a risk factor for meningococcal carriage or disease. Clusters of MD involving nightclubs, universities, military training institutes have been previously reported, and close contacts of persons with confirmed MD are shown to be at increased risk of developing MD (about 1000 times the general population).26–28 The higher attack rate of MD in the oil refinery (34.1 per 100,000 persons) compared with the attack rate (3.0 per 100,000 inhabitants) in the Paulínia city, suggested that the oil refinery environment was a predisposing factor for invasive meningococcal infection. The MD outbreak occurred after an increase in the number of the temporary workers due to the boiler maintenance in oil refinery, confirming that MD risk was closely related to crowed conditions.
During the closed-community-oil refinery outbreak in Paulínia, as well as the population-based outbreak in Cosmópolis, the attack rates were monitored at several intervals to determine whether the rates met guidelines (incidence rates equal to or greater than 10 per 100,000 inhabitants) for implementing additional measures such as vaccination.12,24,25
The availability to genetically characterize the N. meningitidis isolates was of great assistance in giving accurate and up-to-date information to the public health authorities. DNA fingerprinting confirmed the relatedness of C:23:P1.14-6 strains from patients who were from the city of Cosmópolis with the strains recovered from oil refinery cases showing that the same clone of N. meningitidis associated with the oil refinery outbreak was introduced into the community, where almost all the temporary workers were living, causing the population-based outbreak. This evidence associated with the decrease of the MD cases in the refinery showed that the meningococcal polysaccharide vaccine was useful for controlling the closed-community outbreak but did not prevent the spreading of the clone into the community. Although the immunogenicity and clinical efficacy of serogroups A and C meningococcal polysaccharide vaccine has been well established for controlling serogroup C meningococcal outbreaks,25 the polysaccharide vaccine is not able to reduce nasopharyngeal carriage of N. meningitidis, which is essential to herd immunity.29 In the medium and long term, the choice of conjugate vaccine would be profitable, especially in scenarios like the one present in Brazil, where currently 75% of all MD is caused by serogroup C meningococci. In the light of the current scenario the Ministry of Health of Brazil is now considering recommending the use of conjugate vaccine to control outbreaks caused by serogroup C meningococci.
The complex ST-103 N. meningitidis serogroup C has been the cause of sporadic and MD outbreaks in Brazil recently, as previously reported30; however, to our knowledge this is the first reported MD outbreak associated with an oil refinery in Brazil involving additionally an adjacent community.
The molecular characterization of the N. meningitidis strains recovered from the MD cases, and the efficient investigation and the prompt measures implemented were essential for controlling the disease in the region.
Conflict of interestThe authors declare no conflict of interest.
We thank all staff in the regional and municipal epidemiological surveillance for their commitment during the outbreak investigation. We are grateful to Leonard W. Mayer from Laboratory Meningitis and Vaccine Preventable Diseases Branch-CDC, Atlanta, USA, for his excellent suggestions and critical review of the manuscript, to Maria Vaneide de Paiva for assistance in antimicrobial susceptibility analyses, to Maristela M. Salgado for assistance in RT-PCR, to Samanta C. G. Almeida for assistance with Bionumerics software, to Helena K. Sato from CVE Immunization Division for her assistance during the outbreak vaccination both in the refinery and in Cosmópolis and to Ana Freitas Ribeiro head of CVE for her suggestions and assistance in the conduction of outbreaks. We thank Maria Cristina C. Brandileone head of the Reference Laboratory for Meningitis in the Adolfo Lutz Institute, for the assistance in the investigation.