Salmonella osteomyelitis is a rare infection manifested mostly in patients with sickle cell disease. Of all locations, sternal osteomyelitis comprises only 0.3% of the cases,1 the majority being a complication secondary to sternotomy. Primary sternal osteomyelitis is a rare syndrome, with Staphylococcus aureus being the most frequent cause.2 We report the case of a primary sternal osteomyelitis caused by Salmonella.
A 45 year-old male presented with a long-standing history of an osteo-cutaneous fistula over the sternal area. His previous medical history included poorly controlled Diabetes Mellitus and hypertrigliceridemia. His present illness started 16 months before his visit to our hospital, when he developed a left pectoral muscle tear after lifting a heavy object. He initially received conservative care with little improvement, later presenting with fever, pain and edema over retrosternal area. An MRI demonstrated an isolated left major-pectoralis abscess near the left sternum border at the level of third intercostal space, with no chondroesternal involvement. A surgical drainage was performed, obtaining purulent material that grew positive for Salmonella enteritidis with intermediate sensitivity for quinolones (MIC=1ng/mL). Oral ciprofloxacin was prescribed for three months, with clinical improvement. Eight months later, a lump formed over the sternal area, fistulizing days later. Culture grew positive for S. enteritidis and antibiotic was restarted. Patient remained with continuous discharge trough sternal fistula.
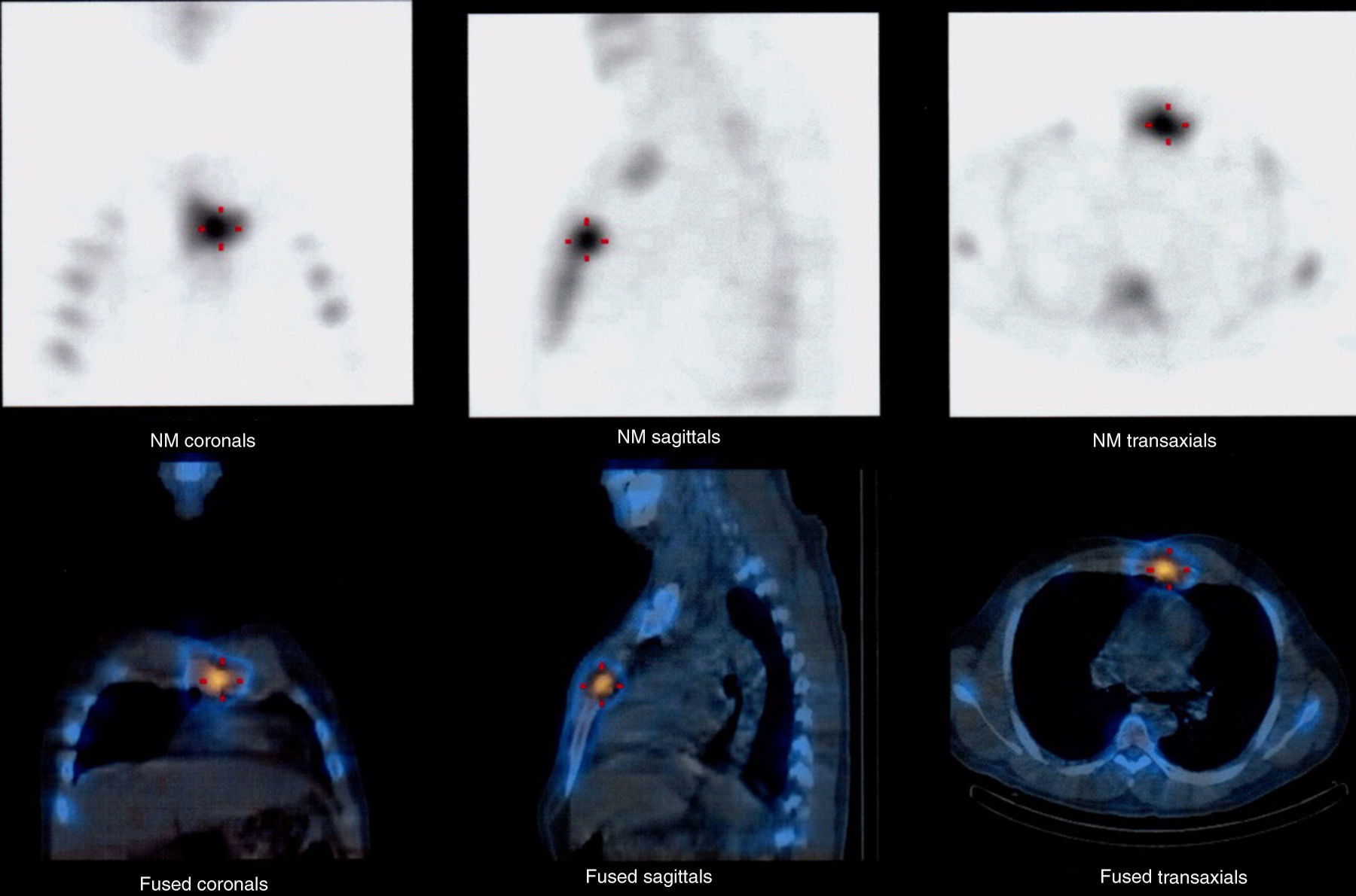
After several months of unsatisfactory evolution, he attended to our hospital for further investigation. Physical examination was remarkable for an osteo-cutaneous fistula over the sternal area. Culture of the sternal discharge grew positive for S. enteritidis. Full laboratory analysis showed a markedly elnacyevated glycosilated hemoglobin (HbA1C=13.02%). We performed a mediastinum-focused Tc 99m bone gammagram that showed early and late radiotracer uptake at left edge of sternal handle. A low dose PET/CT scan confirmed the results and also showed a component of adjacent soft tissue activity in the posterior aspect of costal cartilage (Fig. 1). A full body contrast enhanced CT scan showed no other areas of inflammation or infection. An abdominal ultrasound showed no involvement of the biliary tract. A transthoracic echocardiogram ruled out infective endocarditis. Blood and stool cultures were negative. Open surgical drainage was performed via partial sternotomy, showing fibrous tissue, bad quality bone and the presence of a granuloma fistulising to fourth and fifth intercostals space. Granuloma resection and curettage were performed and a negative pressure wound therapy system was used during 7 days. Antibiotic therapy with intravenous ceftriaxone 1g b.i.d. was administered for 14 days; Trimethoprim 800mg/sulfamethoxazole 160mg q.d. was then continued for six weeks. C-reactive protein, erythrocyte sedimentation rate and control cultures were negative after cessation of antibiotic therapy, and the patient remained symptom free during his follow up.
Salmonella is estimated to cause 0.45% of osteomyelitis, and is most commonly associated with sickle cell disease.3 The three most common strains of Salmonella causing osteomyelitis are Salmonella typhimurium, Salmonella typhi, and S. enteritidis, with S. typhi being the only strain to be transmitted from human to human. Typhoid osteomyelitis has a predilection for patients with comorbidities such as diabetes, systemic lupus erythematosus, lymphoma, liver disease, previous surgery and those at extremes of age. The incidence of typhoid osteomyelitis in otherwise healthy individuals is much lower. Given the extremely low incidence of the pathogen and the very unusual site of infection, it is unsurprising that only two comparable case reports of S. osteomyelitis in the sternum were found. The first case reported a 71 year-old man with primary sternal osteomyelitis caused by Salmonella hirschfeldii,4 treated successfully with surgical debridement and 6 weeks of high dose ampicillin. The second case reported the case of 73-year-old man with Crohn's disease and a history of a sternotomie 15 years before, who developed Salmonella sternoclavicular osteomyelitis subsequent to a S. enteritidis sepsis.5
In regard to our case, we found no clinical risk factors for osteomyelitis other than diabetes mellitus. The history of a left pectoral muscle tear may contribute to tissue friability and local factors predisposing to infection. The isolated Salmonella strain showed intermediate resistance to quinolones: this could explain the persistence of the infection after the first course of ciprofloxacin. The patient denied recent history of gastroenteritis, abdominal pain, thoracic trauma; he also denied high risk sexual practices. Nasal exudate, stool culture and a liver and bladder ultrasound demonstrated no evidence of chronic colonization. Therefore, we diagnosed the case of a true primary osteomyelitis in the absence of secondary foci. To our knowledge, this is the third reported case of a primary osteomyelitis of the sternum. A high clinical suspicion is needed to diagnose the disease.