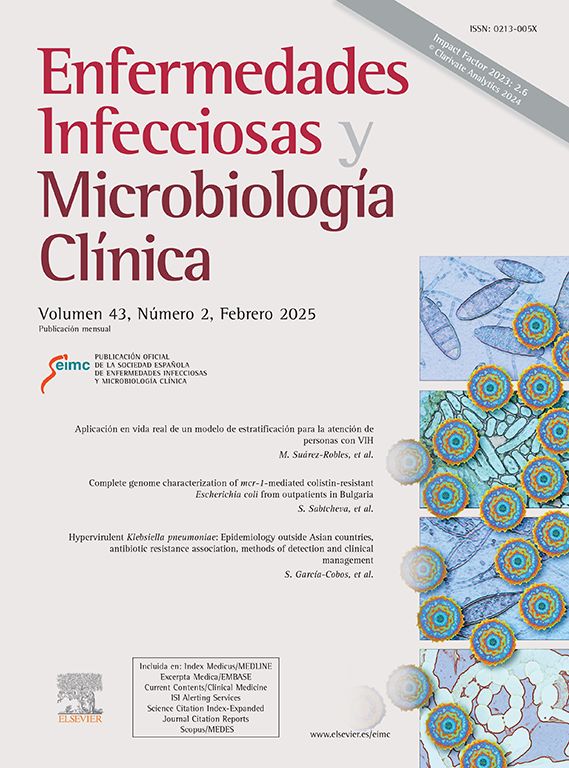
A 17-year-old male presented at the Emergency Department with right knee pain, swelling and fever. The patient reported that the symptons had appeared the previous month. He had suffered two nonspecific acute gastroenteritis episodes during his childhood with no other disease antecedents of interest. Examination revealed pain, warmth and swelling on the anteromedial side of the right knee, with extension limitation. Right knee radiographs were consistent with tibial osteomyelitis (Fig. 1). The laboratory investigations showed a C-reactive protein (CRP) of 65.4mg/L, an erythrocyte sedimentation rate (ESR) of 19mm/h, a total hemoglobin value of 13.8g/dL and a leukocyte count of 14,470cells/μL being 79.2% neutrophils. HCV and anti-HIV 1+2 serological testing proved negative.
EvolutionThe patient was admitted to the Department of Internal Medicine. Magnetic resonance imaging (MRI) of the tibia revealed characteristic features of a Brodie's abscess and a soft tissue abscess (Fig. 2). Surgical curettage and a bone biopsy were performed. The histological examination showed fibrosis and changes suggestive of chronic inflammation. Abscess culture grew Salmonella enterica susceptible to ampicillin, cefotaxime, trimethoprim-sulfamethoxazole, nalidixic acid and ciprofloxacin. The strain was definitely identified at the Spanish National Microbiology Center as Salmonella enterica serotype Rissen. The patient was given cefotaxime and trimethoprim-sulfamethoxazole intravenously. Nine days after admission clinical signs and symptoms improved and the patient was discharged home with a 3-month course of oral cefixime and trimethoprim-sulfamethoxazole. At the follow-up the patient remained asymptomatic, with important radiological improvement.
CommentOsteomyelitis is the most frequent osteoarticular infection during childhood, especially the acute hematogenous form. The subacute form is less frequent and its diagnosis can be complicated.1 Brodie's abscess is a type of subacute osteomyelitis initially described by Sir Benjamin Brodie in 1832 as a localized tibial abscess without systemic signs or fever. Most cases occur before the age of 25 years, and local manifestations typically comprise pain and swelling affecting the metaphysis of the long bones, particularly the tibia.2 Laboratory evaluation is unrevealing with ESR and CRP elevated in about 50% of all cases. Cultures are often sterile.3
The typical radiological image of Brodie's abscess is a single, well-defined lesion with a fine sclerotic margin. Periosteal reaction is mild or absent.2,3 Radiographic appearances mimicking various benign and malignant conditions coupled with a nonspecific insidious clinical course can make its diagnosis difficult. MRI is sensitive, specific and can be helpful in differentiating it from tumors.4–6
Etiologically, Staphylococcus aureus is the organism most commonly associated to Brodie's abscess.3 Osteomyelitis due to Salmonella has a low incidence and is a well-known infection in individuals with sickle cell disease and other haemoglobinopathies, connective tissue disorders or immunosuppression, and also in cases of prior surgery or trauma.1 There are very few reported cases of Salmonella osteomyelitis in healthy patients without risk factors.5–10
Conventional Brodie's abscess treatment involves surgical debridement and appropriate intravenous antibiotic treatment. Bone grafting should be reserved for lesions over 3cm in size or those with fracture risk.1,3 Successful treatment with antibiotics alone has also been reported.7,8
Brodie's abscess in our patient was diagnosed based on the classic clinical and radiological characteristics. The causal agent however was unusual and to our knowledge, this is the first such case reported to date.
We thank the Department of Radiology and Imaging of our institution for the images presented and Dr. Silvia Herrera León from the Enterobacteriaceae Laboratory of the Spanish National Microbiology Center for the full characterization of the strain isolated.