Our aim was to study the proportion of healthcare workers with a positive serology for Influenza A(H1N1)2009 without having flu, in a Spanish hospital at the beginning of the pandemic.
MethodsA survey study carried out during August 2009 (before the peak of the pandemic in Spain) in the Hospital Costa del Sol, a second level hospital with almost 300 beds in the South of Spain. The participants were workers in the following hospital units: Emergencies, Medical Area (Internal Medicine, Chest Diseases), Surgical Area (General Surgery and Anaesthesia) of any professional category. A study was made of the proportion of healthcare workers in our hospital with positive serology for the new influenza A (H1N1)2009 virus, as determined by the haemagglutination inhibition technique (≥1/40). The subjects completed a health status questionnaire, and provided a blood sample for serology testing.
ResultsA total of 239 workers participated, of whom 25.1% had positive serology. The hospital area in which most individuals had positive serology was the Emergency Department (36.6%), while the professional category in which most individuals with a positive serology worked was that of the orderlies (41.7%).
ConclusionAround 25% of healthcare workers in our hospital had positive serology before the peak of the pandemic, none of them had received vaccine for Influenza A (H1N1) 2009 or had been diagnosed of influenza previously.
nuestro objetivo fue estudiar la proporción de trabajadores sanitarios con una serología positivo para Influenza A(H1N1)2009 sin haber tenido síndrome gripal, en un hospital español al comienzo de la pandemia.
Métodosestudio observacional desarrollado durante Agosto de 2009 (antes del pico de la pandemia en España) en el Hospital Costa del Sol, un hospital de Segundo nivel de cerca de 300 camas en el Sur de España. Los participantes eran trabajadores de las siguientes unidades del hospital: Urgencias, Área Médica (Medicina Interna, Neumología), Área Quirúrgica (Cirugía General y Anestesia) de cualquier categoría profesional. Estudiamos la proporción de trabajadores sanitarios con serología positiva para el virus Influenza A (H1N1)2009, determinada por técnica de Inhibición de la Inmunohemaglutinación (≥1/40). Los trabajadores completaron un cuestionario de salud a la par que se les extraía una muestra de sangre para la serología.
Resultadosparticiparon un total de 239 trabajadores, de los que un 25.1% presentaron serología positiva. El area del hospital con mayor porcentaje de individuos con serología positivo fue Urgencias (36.6%), mientras que la categoría profesional con mayor número de individuos positivos fueron los celadores (41.7%).
Conclusionen torno a un 25% de los trabajadores sanitarios de nuestro hospital presentaron serología positivo antes del pico de la pandemia, sin que ninguno de ellos hubiera recibido la vacuna frente al virus Influenza A (H1N1)2009 o hubieran sido diagnosticados de gripe previamente.
In April 2009, the first cases among humans of Influenza A (H1N1) 2009 virus were confirmed in Mexico and the USA,1–3 and in June 2009, a pandemic situation was declared by the World Health Organisation. From the outset, cases of nosocomial transmission were confirmed, affecting healthcare staff.4 Moreover, previous experience with Severe Acute Respiratory Syndrome (SARS) in SE Asia5,6 led researchers to believe that healthcare workers would be particularly vulnerable to the appearance of this new virus.
However, the first series to be published did not show healthcare workers to be over-represented in the incidence of symptomatic cases.4 It is hypothesised that as a result of their greater exposure to the virus at work, they acquire higher immunity than that present in the general population. To date, few studies have been made of seroprevalence among healthcare workers,7,8 and the results reported have been contradictory.
In the present study, we propose to determine the seroprevalence of antibodies to the influenza A virus of the 2009 pandemic among a population of healthcare workers. It is hypothesised that exposure to the virus varies according to the areas of work within the hospital and according to the professional category of the worker, following a gradient of greater to lesser exposure depending on the area of hospital in question (Emergencies>Medical Area>Surgical Area).
Material and methodsStudy population and time horizonThis transversal study was carried out at Hospital Costa del Sol in Marbella (Spain). The hospital has around 350 beds and serves a reference population of 372,964 persons, according to data from the Spanish National Statistical Institute on January 1, 2009.
Participation in the study was proposed at discussions with permanent staff in of Emergency, Internal Medicine and Pneumology departments (medical area) and General Surgery and Anaesthesia (surgical area). Further collaboration was provided by the emergency staff at the High Resolution Specialist Centre (HARE) associated with the hospital. At this latter centre, emergency cases are attended and short-term beds (not exceeding 72h) are available. According to their professional category, the participating personnel were divided into doctors, nurses, nursing auxiliary staff, orderlies and administrative staff.
The participants gave their written signed consent and completed a questionnaire on the presence or otherwise of influenza-related symptoms, and comorbidities associated with a poor prognosis of influenza A.9 Also included were questions on the subject's state of seasonal and pandemic influenza vaccination, any cases of influenza in the immediate family, daily handwashing at work and at home, pharmacological treatment taken for influenza A, a diagnosis of seasonal influenza or of influenza A infection (the latter confirmed by PCR-positive nasal swab). The main study variable was the presence of titres against the new influenza A virus ≥1/40.
Sample collection began on 25 August 2009 and concluded on 16 September 2009. This study was approved by the hospital's ethics committee.
Sample processingThe samples were kept in cold storage at our hospital, before being sent to the National Microbiology Centre at Majadahonda (Madrid, Spain), where they were analysed to detect antibodies against the influenza A virus responsible for the 2009 pandemic; this analysis was performed using the haemagglutination inhibition technique, in a modification of a method previously described.9
The antibody titres for each serum was the greatest dilution presenting inhibition of the haemagglutination power of the viral antigen. Sera were considered positive with titres equal to or greater than 1:40.
Statistical analysisA descriptive analysis was performed, with measures of central tendency and dispersion for the continuous variables, and of frequency distribution for the qualitative ones. In the bivariate analysis, the principle variable was the presence or absence of IHA+ (≥1/40), with the subgroups in the continuous variables being compared by means of the Mann-Whitney U test, while the categoric variables were compared using the chi square test, or Fisher's exact test, when necessary, for the qualitative ones. For the IHA+ result variable, we constructed forward selection multiple logistic regression models, including the variables which in the bivariate analysis obtained p<0.01, with an entry criterion of 0.05 and an output criterion of 0.1, including the odds ratio (OR) values and 95% confidence intervals (95%CI). The level of statistical significance was established at p<0.05.
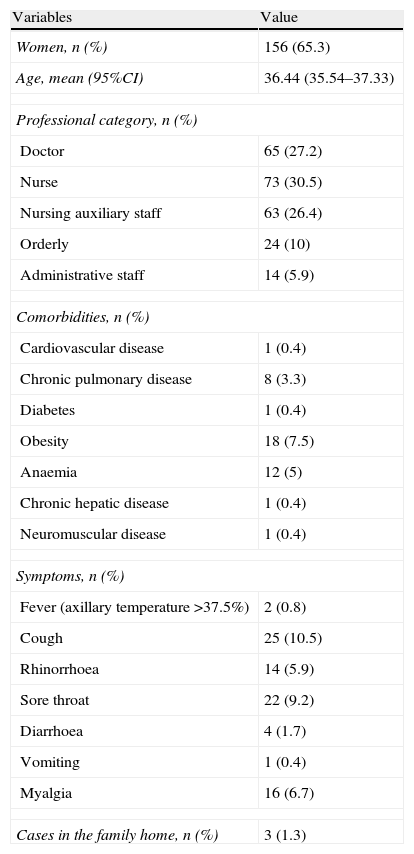
ResultsA total of 239 healthcare workers participated in the study: 113 (47.3%) worked in the emergency department, 49 (20.5%) in the medical area, 46 (19.2%) in the surgical area and 31 (13%) in the emergency department of the peripheral centre associated with the hospital. The principal characteristics of the participants are summarised in Table 1, including the symptoms reported at the moment the blood sample was taken. None of the participants reported suffering dyspnea.
Principal characteristics of the study participants.
| Variables | Value |
| Women, n (%) | 156 (65.3) |
| Age, mean (95%CI) | 36.44 (35.54–37.33) |
| Professional category, n (%) | |
| Doctor | 65 (27.2) |
| Nurse | 73 (30.5) |
| Nursing auxiliary staff | 63 (26.4) |
| Orderly | 24 (10) |
| Administrative staff | 14 (5.9) |
| Comorbidities, n (%) | |
| Cardiovascular disease | 1 (0.4) |
| Chronic pulmonary disease | 8 (3.3) |
| Diabetes | 1 (0.4) |
| Obesity | 18 (7.5) |
| Anaemia | 12 (5) |
| Chronic hepatic disease | 1 (0.4) |
| Neuromuscular disease | 1 (0.4) |
| Symptoms, n (%) | |
| Fever (axillary temperature >37.5%) | 2 (0.8) |
| Cough | 25 (10.5) |
| Rhinorrhoea | 14 (5.9) |
| Sore throat | 22 (9.2) |
| Diarrhoea | 4 (1.7) |
| Vomiting | 1 (0.4) |
| Myalgia | 16 (6.7) |
| Cases in the family home, n (%) | 3 (1.3) |
None of the workers were diagnosed with influenza A, nor had any been vaccinated against this virus. However, 11 (4.6%) workers were diagnosed with seasonal influenza and 40 (16.7%) were vaccinated against seasonal influenza. Only one worker was taking medication (oseltamivir) for this. 60 (25.1%) participants presented antibody titres determined by IHA ≥1/40. The geometric mean of these values was 58.56.
The proportion of positive results was significantly different among the diverse hospital departments: 36.6% in the emergency department, 12.2% in the medical area, 22.2% in the surgical area and 9.7% in the peripheral centre associated with the hospital (p=0.001). We also observed differences by professional category, with positive results among 30.8% of the doctors, 11.1% of the nurses, 30.2% of the nursing auxiliary staff, 23.1% of the administrative staff and 41.7% of the orderlies (p=0.01).
A positive serology was recorded among 31.4% of the women vs. 14% of the men (49 females vs. 12 males, p=0.009). There were no differences in average age between seropositive and seronegative subjects. None of the comorbidities were associated with a greater prevalence of positive serologies. With respect to symptoms, only the presence of rhinorrhoea on the day the serology was determined and was significantly associated with a greater proportion of seropositive subjects (57.1% vs. 23.3%, p=0.009). There were no differences with respect to influenza diagnosed among other family members or whether or not vaccination against seasonal influenza had been received. Of the 11 workers who had been diagnosed with seasonal influenza, 6 (54.5%) presented a positive serology, vs. 23.9% of the other subjects (p=0.03). The geometric mean of the antibody levels in these 6 patients was higher than that of those who had not been diagnosed with seasonal influenza, although without reaching statistical significance (80 vs. 56.56, p=0.32).
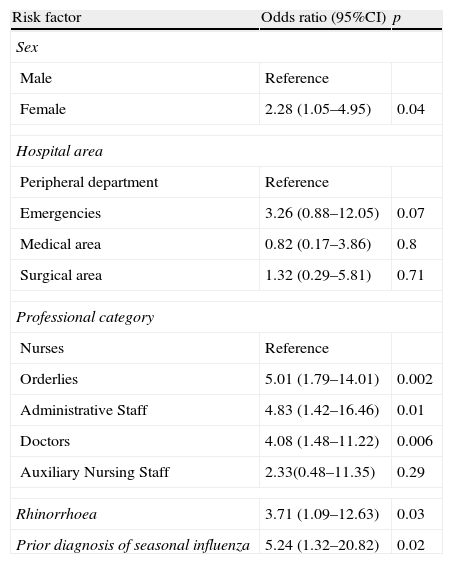
An initial logistic regression analysis was performed, in which the outcome variable was the presentation of positive serology (IHA≥1/40), and in which the independent variables were gender, age, the hospital area in which the worker was active, professional category, the presence of rhinorrhoea, and the prior diagnosis of seasonal influenza. The factors subsequently maintained in the model were female gender (OR 2.28, 95%CI: 1.05–4.95), rhinorrhoea (OR 3.71, 95%CI: 1.09–12.63) and prior diagnosis of influenza (OR 5.24, 95%CI: 1.32–20.82), as well as the professional categories of orderly, administrative staff and doctor. Table 2 summarises the results of the logistic regression analysis.
Results of the logistic regression analysis, including all the study participants.
| Risk factor | Odds ratio (95%CI) | p |
| Sex | ||
| Male | Reference | |
| Female | 2.28 (1.05–4.95) | 0.04 |
| Hospital area | ||
| Peripheral department | Reference | |
| Emergencies | 3.26 (0.88–12.05) | 0.07 |
| Medical area | 0.82 (0.17–3.86) | 0.8 |
| Surgical area | 1.32 (0.29–5.81) | 0.71 |
| Professional category | ||
| Nurses | Reference | |
| Orderlies | 5.01 (1.79–14.01) | 0.002 |
| Administrative Staff | 4.83 (1.42–16.46) | 0.01 |
| Doctors | 4.08 (1.48–11.22) | 0.006 |
| Auxiliary Nursing Staff | 2.33(0.48–11.35) | 0.29 |
| Rhinorrhoea | 3.71 (1.09–12.63) | 0.03 |
| Prior diagnosis of seasonal influenza | 5.24 (1.32–20.82) | 0.02 |
A second model was constructed, excluding the workers who had previously been diagnosed with seasonal influenza. The results of this are shown in Table 3. In this model, the factors subsequently maintained were rhinorrhoea (OR of 3.65; 95%CI: 1.03–12.92), working in the emergencies area (OR of 3.84, 95%CI: 1.04–14.09) and professional category of doctor, administrative staff or orderly (OR of 8.19, 7.22 and 7.21, respectively).
Results of the logistic regression analysis excluding the subjects with prior diagnosis of seasonal influenza.
| Risk factor | Odds Ratio (95%CI) | p |
| Hospital area | ||
| Peripheral department | Reference | |
| Emergencies | 3.84 (1.04–14.09) | 0.042 |
| Medical area | 0.83 (0.17–4.04) | 0.81 |
| Surgical area | 1.93 (0.44–8.43) | 0.37 |
| Professional category | ||
| Nurses | Reference | |
| Orderlies | 7.21 (2.19–23.74) | 0.001 |
| Administrative Staff | 7.22 (1.79–29.06) | 0.005 |
| Doctors | 8.19 (2.47–27.12) | 0.001 |
| Auxiliary Nursing Staff | 3.6 (0.66–19.53) | 0.14 |
| Rhinorrhoea | 3.65 (1.03–12.92) | 0.045 |
In our series, we observed a high prevalence of healthcare workers presenting positive serology for the influenza A virus responsible for the 2009 pandemic, with a quarter of the study subjects being affected. Furthermore, there was a higher prevalence in the emergency department, an area where exposure to respiratory viruses is assumed to be greater. This was aggravated by the constant flow of patients with both severe and banal pathologies, such that exposure to the virus could have been gradual over time.
Our study was carried out between weeks 34 and 37 of the epidemiologic year. Although the pandemic was declared in week 23, penetration of the influenza A virus at that moment was relatively low and had not reached the threshold value of previous years. From week 28 onwards, the pandemic virus was predominant throughout Spain,10 and so the workers who had previously been diagnosed with seasonal influenza had a high probability of presenting non-severe influenza A. The threshold value was exceeded in week 38, and the rising phase of the pandemic wave was verified in Spain from week 40 of 2009, and so our data predate the moment of greatest expansion of the virus.
Our study population was relatively young, and in the absence of influenza symptoms presented humoral immunity levels (measured by IHA) comparable with those of the general population following the first spike of the pandemic in the United Kingdom. In the study by Miller et al.,11 the population group aged 25–44 years presented a prevalence rate of positive serology of 20.3% (95%CI: 12.5–31.2), although it should be observed that the first spike of incidence of influenza A virus had occurred prior to extraction of the samples.
In our study, expansion of the virus in Spain had not even entered the rising phase of the pandemic wave, which supports the hypothesis that, at least among healthcare workers, humoral immunity was acquired, probably as a result of repeated exposure to the virus. The volunteers participating in our study had a mean age of 36 years, which excludes the possibility that the humoral immunity acquired could have been related to historical exposure to the influenza A virus, as was the case with those born before 1957.12 We also reject the hypothesis that immunity is related to prior vaccination for seasonal influenza virus, as its cross-reactivity with pandemic virus is almost non-existent.13 The high seroprevalence observed is coherent with the fact that these healthcare workers did not present a higher incidence of cases of influenza A despite their presumably greater exposure, as a result of their work, because although they were more exposed, the proportion of protected subjects would also have been higher.
It is noteworthy that rhinorrhoea is significantly associated with a positive serology; this is probably the expression of banal respiratory disorders, which could include infections caused by the influenza virus.
When the cases with a prior diagnosis of seasonal influenza (which were very probably oligo-symptomatic influenza A) were excluded from the analysis, the professional categories in our population presenting the highest risk of being seropositive were the doctors, followed by the orderlies and the administrative staff. Although the case of the doctors could be explained by their high rate of exposure to symptomatic cases, this would not be so in the case of the administrative staff. The latter case might reflect an exposure derived simply from their presence in the hospital without having adopted special measures of protection.
In this study, the participants were not selected by random sampling; we recruited volunteers, and therefore selection bias might be present. Moreover, we did not calculate a sample size beforehand, which does limit the power of our conclusions, although at the moment of designing this study there was no prior information on seroprevalence among healthcare workers, and our main goal was to compile information before the pandemic reached its peak.
To date, two series of serologic studies have been published regarding healthcare workers and the influenza A pandemic. One of these studies describes seroprevalence in the context of the pandemic wave in Taiwan,7 and identified a 20% seropositive rate among healthcare workers, vs. 2.9% in the general population. There was also seen to be a higher proportion of seropositive results among workers facing the highest risk (in the emergency and infectious disease departments) vs. those at low risk. These findings are similar to those obtained from our series, although in our case the difference according to the area worked within the hospital was not so clear-cut.
This second such study concerned the incidence of seroconversion among a population of healthcare workers in Singapore.8 This study reported that seroconversion is associated significantly with episodes of respiratory infections, working as a nurse and working in areas where influenza A patients are hospitalised. These findings suggest that exposure in the workplace is associated with a higher rate of seroconversion. This study, too, was carried out during the rising phrase of the pandemic wave in the region.
Our study reveals the high degree of immunisation among healthcare workers before the rise of the pandemic wave in Spain. This type of study, of populations at high risk of exposure, can help contextualise the expansion of emerging viruses such as the influenza A(H1N1) virus, responsible for the 2009 pandemic.
FundingProject funded by Instituto de Salud Carlos III through CIBER de Epidemiología y Salud
Conflict of interestThe authors declare no conflicts of interest.
Project funded by Instituto de Salud Carlos III through CIBER de Epidemiología y Salud.
All authors report no conflicts of interest relevant to this article
Javier García-Alegría, Alfonso del Arco, Javier de la Torre, José Luis Prada, Miguel Marcos, Fernando Fernández, Marta Aranda, Manuel Vergara, Juan Carlos Toribio, José Antonio Rodríguez and Paola Pérez (Hospital Costa del Sol), Antonio Jesús Núñez, José Javier Santos and Francisco Pozo (Hospital de Antequera), José María Quintana, Susana García and Carlota Las Hayas (Hospital de Galdácano), Antonio Escobar, Juan Carlos Fernández and María García (Hospital de Basurto), José Ramón Sáenz, Emilio Pérez-Trallero and Diego Vicente (Hospital de Donosti), Ignacio Sánchez Arcilla, Marina Fernández y Magdalena Muedra (Hospital Ramón y Cajal), Consol Serra, Rocío Villar and Josefina Pi-Sunyer (Hospital del Mar), Pilar Varela, Victoria Oliver and Ana Vileilla (Hospital Clinic de Barcelona), Carlos Pereda and María Angeles Herrería (Hospital de Santa Bárbara), Carmen Valero, Lucía Fernández and María Angustias Romera (Hospital de Santa Ana), Pedro González and José María Jover (Complejo Hospitalario de Jaén), Manuel Zarzuela, José Gutiérrez and María Carmen Lozano (Hospital Puerta del Mar), Fernando Yélamos, Manuel Rodríguez and José Ramón Maldonado (Hospital de Torrecárdenas), María Carmen Ubago, Amelia Fernández and Dolores Torres (Hospital Virgen de las Nieves), Salvador Oña, Juan Arcos and Dolores Lerma (Hospital Materno Infantil de Málaga), David Sadia and José Bascuñana (Hospital Infanta Leonor), Berta Moyano and Elías Rodríguez (Hospital del Tajo), Francisco Martos (Facultad de Medicina, Universidad de Málaga), Antonio Daponte (Escuela Andaluza de Salud Pública), María José Pérez, Encarnación Román, Carmen Escassi and Eduardo Briones (Hospital de Valme, Sevilla), José María Mayoral (Dirección General de Salud Pública, Consejería de Salud de la Junta de Andalucía), and Mónica González Esguevillas, Isabel Pérez Grajera and Jesús María de la Fuente (Centro Nacional de Microbiología, Instituto de Salud Carlos III).