Acute hepatitis due to the hepatitis C virus (HCV) is frequently seen in men who have sex with men (MSM), coinfected or not with HIV, but the presentation as severe hepatitis is extremely uncommon.1 SARS-CoV-2 infection can have different effects on the liver, including direct parenchymal infection, cytokine-mediated tissue injury, etc.2 However, it is not clear whether SARS-CoV-2 could change the clinical expression and/or natural history of viral liver diseases.
Here, we report the case of an HIV-infected man with concomitant SARS-CoV-2 and HCV infection, who developed severe acute hepatitis.
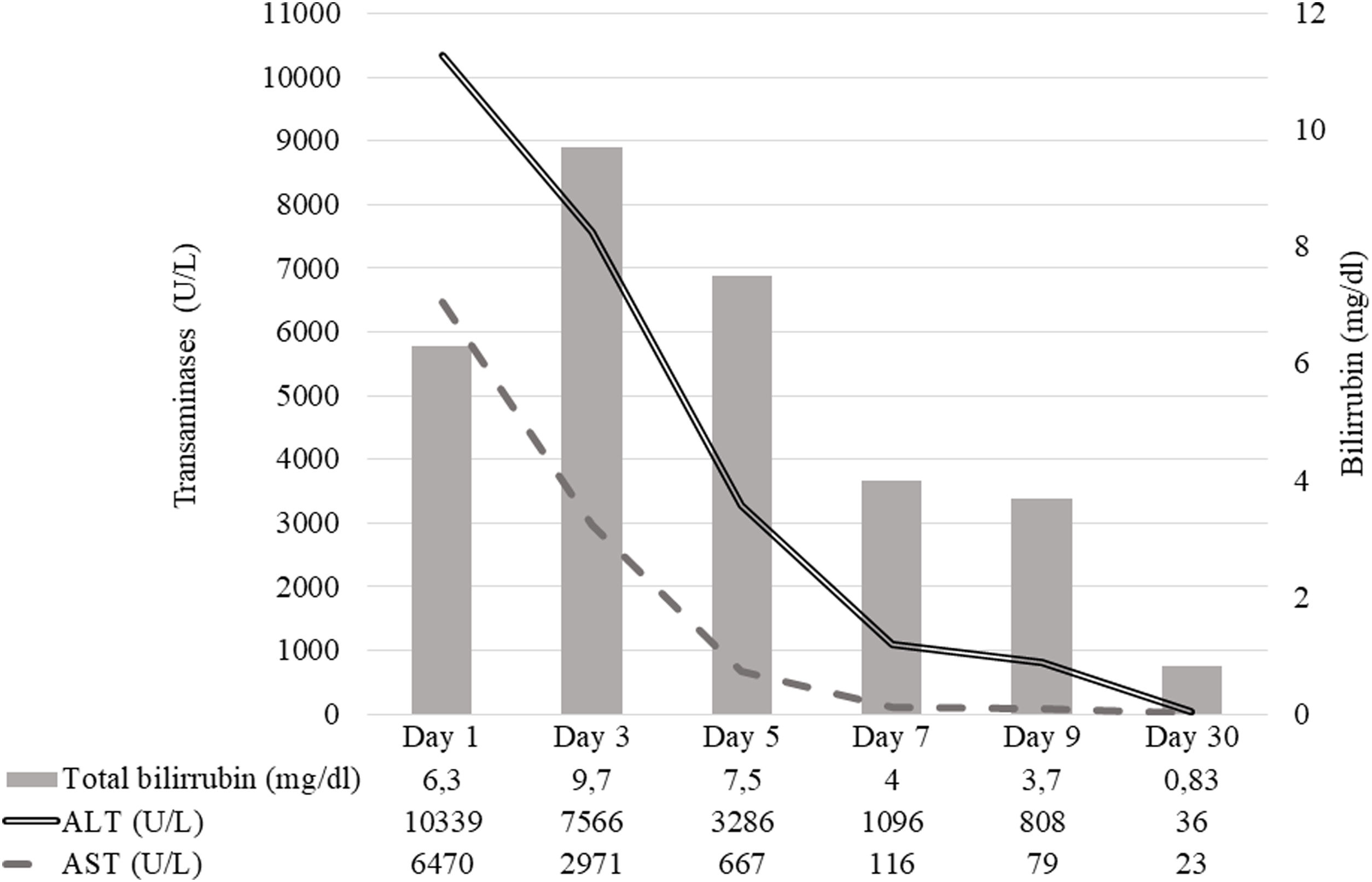
A 44-year-old male infected with HIV, who had been taking antiretroviral treatment with tenofovir disoproxil alafenamide, emtricitabine, and darunavir-cobicistat for 5 years, attended the Emergency Department of our hospital. He was a MSM with an open relationship partner, without regular condom use. He reported not attending chem-sex parties or using intravenous drugs. He showed plasma HIV load below the detection level and 891 CD4 cell/μL three months earlier. He had not been vaccinated against SARS-CoV-2. He complained of a fever and cough of 48h. He reported narrow contact with a relative with COVID-19. Then a SARS-CoV-2 nasopharynx PCR test was performed, with a negative result. An X-ray chest film showed no evidence of pneumonia. He was discharged without treatment. Fifteen days after initial presentation, he returned to the Emergency Department complaining of nausea, fever reemergence, general malaise, diffuse abdominal pain, jaundice, and dark urine for 2 days. Physical examination revealed conjunctival jaundice, without evidence of encephalopathy or ascites. A new nasopharynx SARS-CoV-2 PCR test yielded positive results. Blood analysis showed plasma gamma glutamyl transferase (GGT) 171U/L, alanine aminotransferase (ALT) 10,339U/L, aspartate aminotransferase (AST) 6470U/L, alkaline phosphatase (FA) 201U/L, total bilirubin 6.2mg/dL, INR 1.58 and ferritin 38,009ng/mL. Serum antibodies against HCV, which had been negative 6 months earlier, were then positive. Plasma HCV-RNA level was 219,000IU/mL (genotype 1a). He received intramuscular vitamin K and no other therapy. He did not develop signs of encephalopathy but, on day 3 of admission, total bilirubin rose to 9.7mg/dl, whereas aminotransferases had declined (ALT 7566U/L and GOT 2971U/L). HCV-RNA became undetectable and plasma bilirubin and aminotransferase levels returned to normal values 4 weeks after symptom onset. The evolution of the liver function test in the acute hepatitis episode is shown in Fig. 1.
The vast majority of cases of acute HCV infection are asymptomatic and fulminant hepatitis is an exception.1 The patient reported here developed acute hepatitis C with severity signs, such as increased INR and transaminase levels consistent with massive cytolysis. SARS-CoV-2 has liver tropism that causes liver injury comparable to previously characterized hepatotropic viruses, including acute hepatitis.3 However, to our knowledge, it has not been reported so far that SARS-CoV-2 coinfection could increase the severity of an acute HCV infection, as it seems to have occurred in this case. Two mechanisms could explain this additive or synergistic effect: on the one hand, there could exist a cumulative effect of direct cytopathotoxicity of both viruses. On the other hand, the pro-inflammatory state created by SARS-CoV-2 infection can trigger autoimmune liver damage causing autoimmune hepatitis.4 Consequently, we cannot exclude that an autoimmune component underlies the severe presentation of acute hepatitis C in this patient.
HIV accelerates the progression of HCV infection, but the severity of acute hepatitis C in HIV-infected and non-infected patients is similar.5 Although it could not be completely ruled out, it is unlikely that HIV coinfection would have an impact on the clinical course of acute HCV hepatitis with simultaneous SARS-CoV-2 infection.
This case suggests that SARS-CoV-2 coinfection could increase the severity of HCV infection, especially acute hepatitis. Further studies are needed to confirm this issue. While available, we should keep in mind the possibility of simultaneous acute coinfection with HCV and SARS-CoV-2, especially in COVID-19 surges, because acute coinfection could require closer clinical and biochemical monitoring than acute monoinfection with HCV.