Meningitis, in both its bacterial and viral forms, is a prevalent disease amongst the paediatric population. However, there are few reported cases of simultaneous infection with both aetiological agents.1–6 Here, we describe the case of an infant who presented meningitis caused by both Streptococcus pneumoniae and enterovirus.
An 11-month-old baby with no significant medical history and up-to-date immunisations (including pneumococcal conjugate vaccine PCV13) came to the Emergency Department presenting fever without focus of five days’ duration. During the physical exam, tachypnea, tachycardia and poor distal perfusion were noted. A tense, bulging fontanelle was also observed, along with a stiff neck and Brudziński's sign.
Cloudy cerebrospinal fluid (CSF) was extracted following a lumbar puncture and sent for biochemistry and microbiology testing. On the suspicion of bacterial meningitis, empiric antibiotic therapy was initiated with cefotaxime (300mg/kg/day/8h) and vancomycin (60mg/kg/day/6h), to which corticotherapy with dexamethasone (0.5mg/kg/day/6h) was later added.
Biochemistry testing revealed predominantly polymorphonuclear pleocytosis (653cells/μl: 88% neutrophils and 12% lymphocytes), hypoglycorrhachia (1mg/dl) and hyperproteinorrhachia (259mg/dl). The patient's Gram stain showed gram-positive diplococci, prompting the performance of pneumococcal antigen testing (™ BinaxNow®S. pneumoniae; Alere), which was positive. Moreover, given that the case presented during the peak of an enteroviral meningitis epidemic, detection of the latter was also requested.
After culturing the CSF sample in blood and chocolate agar, growth of S. pneumoniae was observed following 15hours of incubation at 37°C with 5% CO2. An antibiogram was performed with strips of antibiotic gradient (E-test®) in MH-F agar (Oxoid) and proved sensitive to penicillin (MIC: 0.01μg/ml), cefotaxime (MIC: 0.01μg/ml) and vancomycin (MIC: 0.5μg/ml), applying the EUCAST 2016 version 6.0 breakpoints. Furthermore, strain serotyping performed at the Spanish National Microbiology Centre concluded that it belonged to serotype 15B.
Meanwhile, enterovirus detection by means of an in-house end-point PCR technique7 was positive, and this result was confirmed with real-time PCR (RealCycler® ENTV-U/ENTV-G; Progenie Molecular) using the SmartCycler® system.
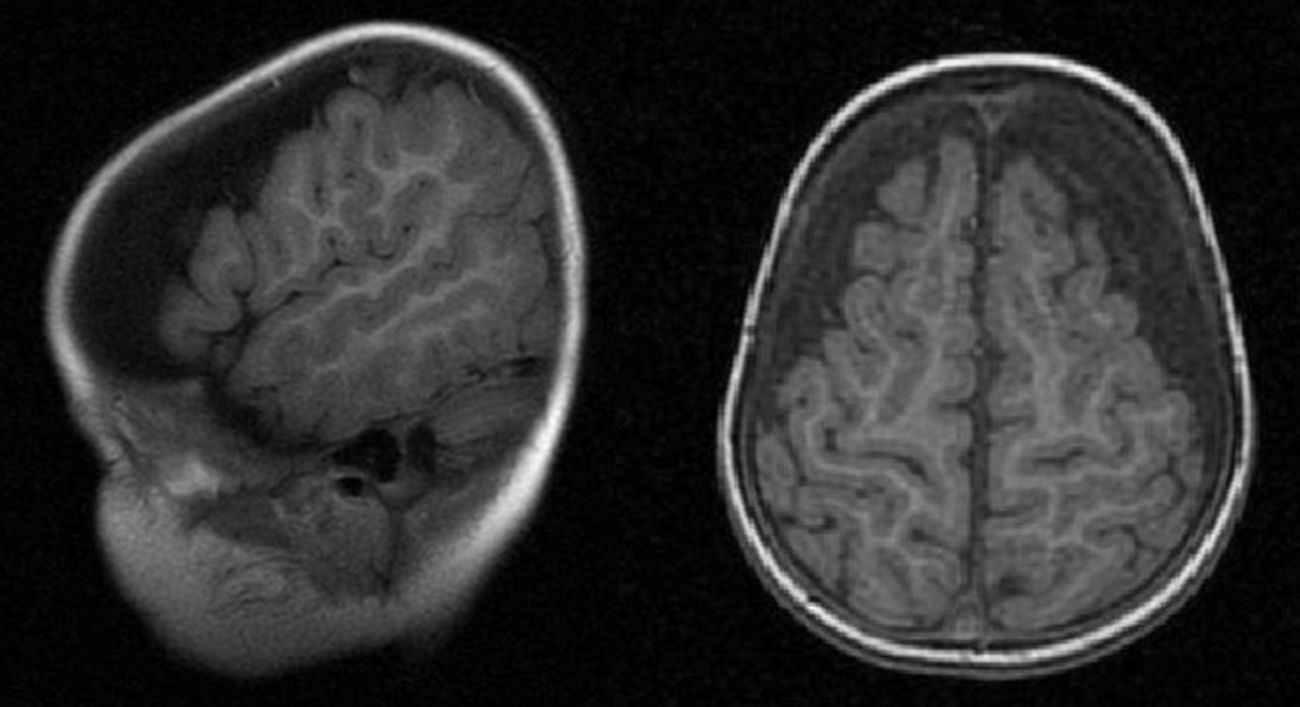
Given the antibiogram result, treatment with cefotaxime was continued and vancomycin was withdrawn. Nevertheless, on the patient's seventh day in hospital, she presented an altered level of consciousness and paresis of the right arm. Subdural hygromas were also visible in both hemispheres on her brain CT and MRI scans (Fig. 1), and she was thus transferred to the ICU. An additional lumbar puncture was performed, which found a reduction in the patient's cell count and negative microbiological culture. Likewise, video-EEG monitoring revealed diffuse slowing of the patient's brain activity, which is indicative of mild to moderate encephalopathy, without epileptiform discharges. Finally, given her good clinical evolution, the patient was discharged after completing 14 days of antibiotic therapy with cefotaxime.
S. pneumoniae is an encapsulated gram-positive diplococcus, the natural reservoir of which is the human nasopharynx. It is responsible for a wide range of childhood conditions, from local diseases (acute otitis media and sinusitis) to invasive systemic diseases (bacterial pneumonia, sepsis and meningitis)8. In fact, in Spain S. pneumoniae is one of the most common causes of bacterial meningitis from the first month of life.9 Its main virulence factor is its capsule, the polysaccharide composition of which allows it to be classified into serogroups and serotypes. There are 48 known serogroups, comprising 91 serotypes.10 As such, preventing the disease through vaccination is complex. The 13-valent pneumococcal conjugate vaccine (PCV13), which was authorised in Spain in June 2010 and has formed part of the Cantabrian children's immunisation schedule since July 2015, includes the 7 serotypes of the heptavalent vaccine PCV7 (4, 6B, 9V, 18C, 19F and 23F) plus serotypes 1, 3, 5, 6A, 7F and 19A. However, in the case presented above, the causal serotype (15B) would only be included in the 23-valent polysaccharide vaccine, which is not indicated in children under two years of age due to its low immunogenicity.
Enteroviruses, on the other hand, are the main aetiological agents of paediatric aseptic meningitis, particularly during the summer and autumn. They are also associated with respiratory and gastrointestinal infections, and routinely present an acute and benign course. Their reservoir is usually the human gastrointestinal tract, with transmission via the enteric route.11
Mixed bacterial and viral meningitis is uncommon. In the medical literature, there are few reported cases of co-infection with enteroviruses and different bacteria,1–6 including S. pneumonia.3,5,6 It is not entirely clear in these cases whether the viral infection precedes the bacterial infection, or if both occur at the same time. Some authors note that there might not be any causal relationship between the two pathogens, and that simultaneous detection could be coincidental.3 This would occur as a result of the high prevalence of enteroviruses within the community, as in our case, where it presented during the peak of the enterovirus epidemic (spring).
However, as other authors suggest,6 prior viral infection could have predisposed our patient to bacterial meningitis, as it would increase the adherence of S. pneumoniae to the nasopharyngeal mucosa given the viruses’ capacity to alter the respiratory epithelium and boost bacteria–cell interaction. This hypothesis is also supported by the fact that we do not know how long PCRs on CSF for the detection of enterovirus and other viruses remain positive following a clinical or subclinical infection12; we mostly tend to make an assumption due to the complex nature of taking CSF samples, which makes it difficult to perform a range of tests. It is also possible that our patient, regarding whom we have discussed co-infection, had a prior enterovirus infection followed by a bacterial infection, as often occurs with community-acquired pneumonia following viral influenza, which is also suggested in the literature.12
Regardless of the pathogenic role of viruses and bacteria in meningitis, the simultaneous isolation of both pathogens in CSF has important implications for clinical management, especially due to the current availability of rapid enterovirus molecular diagnostic testing. The detection of enterovirus in CSF should not be the only factor when deciding whether to introduce or suspend a prescribed antibiotic therapy. The patient's bloods, history and physical exam are also decisive in guiding the diagnosis of meningitis symptoms. Moreover, as occurred in our case, in the management of part-treated meningitis, the clinical interpretation of virus detection in CSF must be performed within the context of a detailed medical history, along with clinical and laboratory findings.5 In our case, both the initial physical exam and the biochemistry CSF analysis seemed to suggest bacterial meningitis. Likewise, the clinical evolution of the mixed infection was no different to classic bacterial meningitis, as noted above.6
Please cite this article as: Angulo López I, González Escartín E, Aguirre Quiñonero A, Ots Ruiz E. Meningitis simultánea por neumococo y enterovirus en lactante. Enferm Infecc Microbiol Clin. 2017;35:128–130.