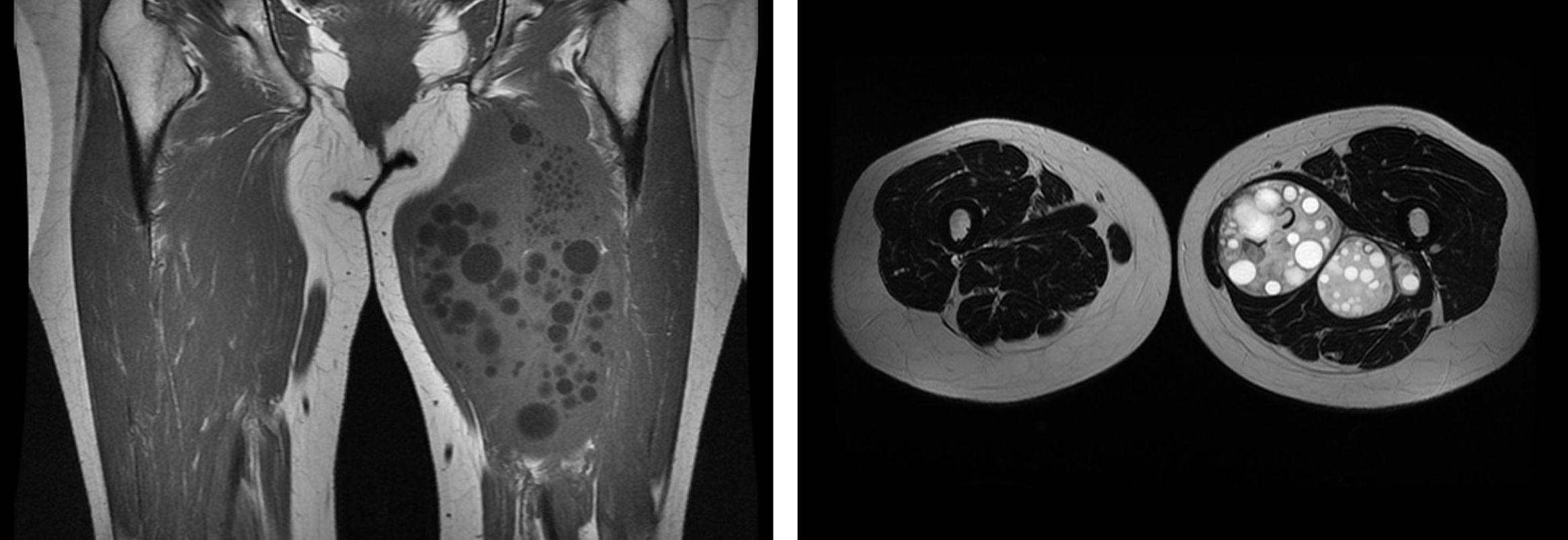
A 57-year-old woman consulted in August 2014 with a painless, slow-growing mass on the anterior aspect of her left thigh. In 1998, she developed a small subcutaneous mass in the left inguinal region. The mass was assessed by physical examination. No investigations were performed, and no aetiological diagnosis made. A “wait and see” approach was decided on. Over the following years, although it remained painless, the mass gradually grew until it had reached such a size that the patient decided to consult once again. She had no relevant medical history and was not taking any medication. She was Caucasian Spanish, and had not travelled abroad. On examination, the patient's general condition was good, she was afebrile and her vital signs were normal. An increase in the size of the left thigh was apparent, caused by a painless, hard subcutaneous mass on the anterior aspect of the thigh extending from the groin to the knee, with normal-looking skin. The rest of the physical examination was normal. Conventional analysis was performed, consisting of full blood count and liver, kidney and metabolic profiles, which were normal. Magnetic resonance imaging (MRI) (Fig. 1) showed multiple space-occupying lesions in the left thigh.
OutcomeThe MRI showed the presence of multiple space-occupying lesions in the adductor muscle compartment (adductor brevis, longus and magnus), causing a significant increase in volume. The lesions were adjacent to each other, some bulky, the largest being 68×61×142mm, and together they extended to a length of approximately 210mm. The lesions showed a hyperintense signal in T2 and isointense in T1, and they had a thin hypointense capsule in T2 sequences that enhanced contrast. Some of the lesions contained round lesions inside, hyperintense in T2 and hypointense in T1 (cysts within the cyst, forming daughter cysts). Radiologically, these findings suggested hydatid cysts at different stages (CE3B and C4). The determination of IgG antibodies against Echinococcus was 2.7 (n<0.9).
The diagnosis of muscle hydatidosis was made. A CT of chest and abdomen showed no hydatid cysts in other locations. Approaching through the thigh adductor compartment, a surgical cyst-pericystectomy was performed and a 190×100×50mm piece with multiple lobules weighing 696g was obtained. The outer surface was completely covered by a fibrous tissue. At the opening, multiple yellowish membranes were observed, some of them forming cysts of varying sizes from 6 to 22mm. These cystic cavities consisted of an external wall corresponding to a germinal layer on which bodies of Echinococcus granulosus were observed.
CommentsEchinococcosis or hydatidosis is a parasitic zoonosis caused by different species of the genus Echinococcus, mainly E. granulosus, responsible for 95% of cases of hydatidosis.1 It can be found anywhere, but it predominates in temperate countries. The highest prevalence in Spain is in the central and northern regions.2–5 From a clinical point of view, it tends to be a silent disease, and the usual symptoms are local pain or discomfort when the cysts grow large. The most common sites are the liver (50–75%) and lungs (20–30%). Hydatid cysts have been described in a multitude of different sites, including musculoskeletal tissue.5–8
Muscle hydatidosis is very rare, and only anecdotal cases or short series have been published.5–8 The most common sites are thigh, buttock, shoulder and paravertebral muscles, and, in 40% of cases, only one site is affected.7,8 As happened in the case described here, it behaves like a very slow-growing painless mass, which is usually asymptomatic until the size of the tumour makes it noticeable. In the differential diagnosis of muscle hydatidosis, chronic osteomyelitis, giant cell tumour of bone, solitary cysts, neurofibromatosis, tuberculosis, fibrocystic disease and certain types of sarcoma should all be considered. Diagnosis can virtually always be confirmed by imaging tests. The recommended treatment is surgical removal. In our case, the excision was not complete in the first surgical intervention. Treatment was started with albendazole, but had to be withdrawn after two months because of severe hepatic toxicity. Finally, a second surgical intervention was successful.
Please cite this article as: Vidal-Gonzalez J, Peraire M, Perpiñán C, Viladés C. Masa indolora en muslo de crecimiento lento. Enferm Infecc Microbiol Clin. 2018;36:196–197.