Echinococcosis is a zoonosis caused by the larval form of the cestode Echinococcus granulosus. The cerebral affectation in the human is uncommon; only in 1–2% cases is observed encephalic involvement. This condition occurs mainly in the pediatric population and it is characterized by the presence of single and unilocular cysts. We report a case of a 29-year-old patient who came to the emergency department with a disabling headache of several weeks of evolution. In the brain imaging study a mass of unknown origin was visualized, finally it turned out to be a bilobed hydatid cyst. Regarding this case, the clinic-epidemiological, diagnostics and treatments aspects of cerebral hydatid disease will be reviewed.
La hidatidosis es una zoonosis causada por la larva del cestodo Echinococcus granulosus. La afectación cerebral en el ser humano es inusual, sólo en el 1–2% de los casos se observa compromiso encefálico. Este cuadro se presenta fundamentalmente en población pediátrica y se caracteriza por la presencia de quistes únicos y uniloculares. A continuación, se presenta el caso de una paciente de 29 años que acude a urgencias por una cefalea invalidante de varias semanas de evolución. El estudio cerebral mediante imagen, revela la presencia de una masa de origen desconocido, siendo el diagnóstico final de quiste hidatídico bilobulado. A propósito de este caso, se revisarán los aspectos clínico-epidemiológicos, diagnósticos y tratamientos de la hidatidosis cerebral.
Cystic echinococcosis or hydatidosis is a zoonosis caused by the larval stage of the Echinococcus granulosus (E. granulosus) parasite, of which 10 different genotypes have been identified. Other clinically relevant species are: Echinococcus multilocularis (E. multilocularis), the causative agent of alveolar echinococcosis, and Echinococcus vogeli and Echinococcus oligarthrus, the causal agents of neotropical polycystic and unicystic echinococcosis, respectively.1 Its definitive hosts are dogs and other wild canids, and sheep predominate as the intermediate host; the human being acts as an accidental intermediary.2 In humans, the most frequently affected organs are the liver and the lung and only in 1%–2% is there brain involvement.3
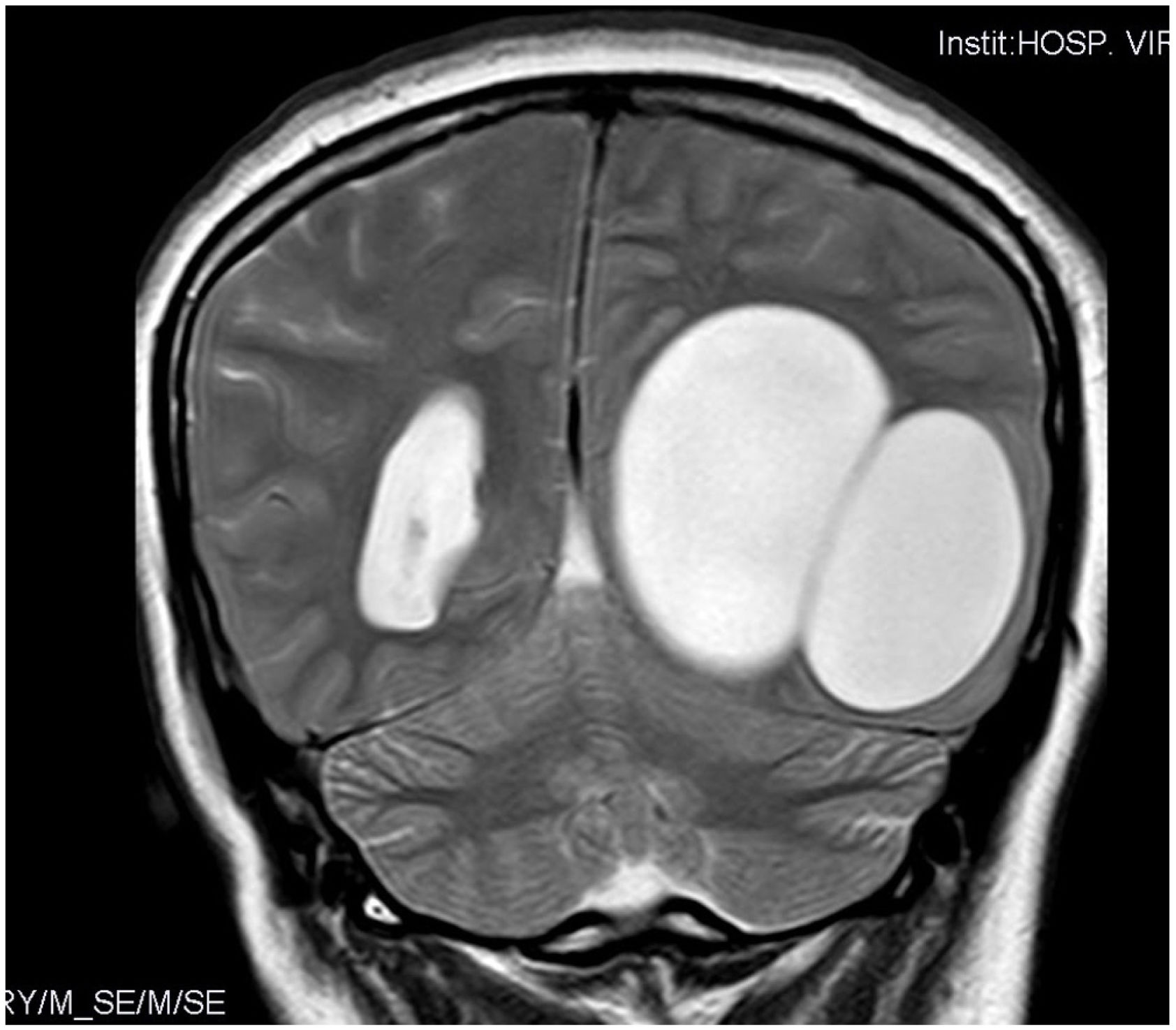
Case reportA 29-year-old woman from Eastern Europe (Romania) who came to the Emergency Room with symptoms of intense left occipital headache radiating to the nape of the neck coursing for several weeks. She reported an intensification of the pain during the previous week until it became crippling, accompanied by vomiting. In the directed anamnesis, she described a progressive loss of vision lasting four months and a right homonymous hemianopsia was detected on physical examination. A neuroimaging study was performed using computed tomography (CT), revealing a large cystic structure in the left temporooccipital region (Fig. 1).
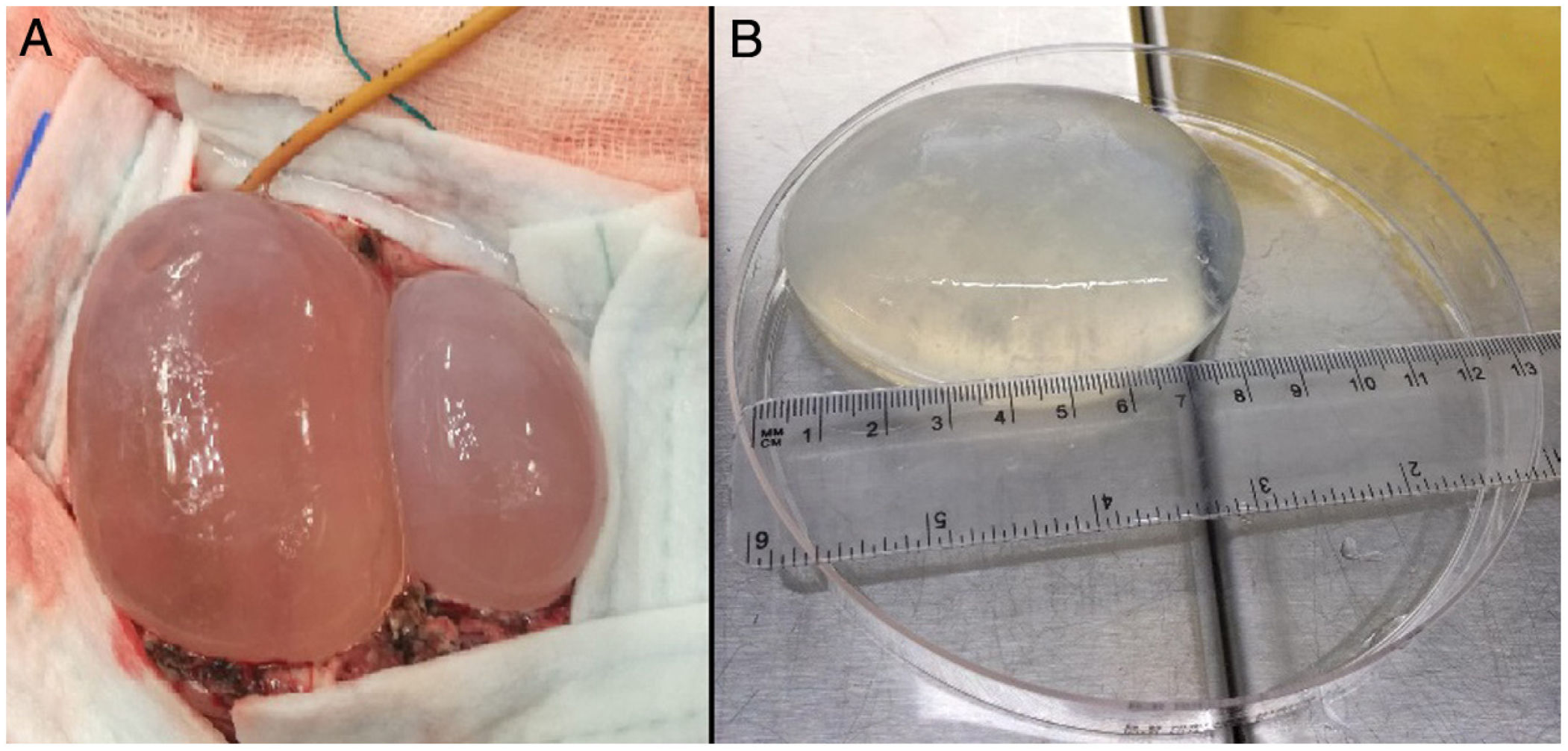
During her hospitalisation, the imaging study was completed with magnetic resonance imaging (MRI), in which a left parietooccipital polylobulated cystic lesion with no surrounding oedema was observed. Another mass was subsequently observed at the level of the mediastinum. In view of the diagnostic suspicion of echinococcosis, an antibody serology test against E. granulosus was conducted by indirect haemagglutination, yielding a negative result. The patient underwent surgery and two brain cysts were resected. The exeresis technique was conducted by performing a cranial linear cortisectomy at the upper limit of the cysts and subsequent resection of the malacic brain parenchymal band that covered their posterior pole, thus exposing both. The next step was the dissection of both cysts from the adhesions of their deep surface from the brain. To do this, the "Dowling technique" was used, consisting of the insertion of a catheter in the virtual plane between the brain and the cyst, and once in place to progressively inject physiological saline through the catheter and thus achieve the gradual separation of the cyst (Fig. 2). Using this technique, both cysts were successfully resected without rupturing either one. One of them was sent to the parasitology laboratory for a definitive diagnosis (Fig. 2).
(A) Dissection of hydatid cysts using the Dowling technique (note the catheter in the upper part of the image, in the deep plane between the medial cyst and the brain). (B) Macroscopic appearance of the largest cerebral hydatid cyst. Measurements: 8.5 cm in length and 110 ml in volume.
Part of the liquid content was extracted by means of cyst puncture for a direct vision microscopic study, with protoscolices with hooks and suckers observed, thus confirming the diagnosis of E. granulosus cerebral echinococcosis (Fig. 3).
Microscopic study of the hydatid cyst content. (A) Protoscolice of Echinococcus granulosus (E. granulosus), showing hooks (indicated with the arrow) (20×). (B) Evaginated protoscolice of E. granulosus de 220 μm, hinting at the crown of hooks and suckers (20×). (C) Close-up of the extended hooks (40×).
After confirmation of diagnosis, and following surgery, treatment was initiated with albendazole 400 mg every 12 h for three months and dexamethasone 1 mg every four hours for three days. The patient evolved favourably and was discharged one month later; one week afterwards, the patient was readmitted for extraction of the cyst at the level of the mediastinum, which was performed by median sternotomy without complications. In the context of the brain cyst, this lesion was diagnosed as hydatid by imaging. At subsequent appointments in the course of the following year, the cystic lesions (cerebral and mediastinal) resolved without visible recurrence.
DiscussionCystic echinococcosis or hydatidosis is a parasitic disease that develops in humans as a result of accidental infection caused by the larva of the E. granulosus2 cestode. Echinococcosis has a universal distribution, with a higher prevalence in temperate climates, with the prevalence in Romania, the patient's country of origin, being 0.41% according to data obtained from the HERACLES project. This project seeks to afford visibility to the real magnitude of this disease and thus avoid underdiagnosis in regions of high prevalence.4 In 2019, the European Union reported a rate of 0.18 cases/100,000 inhabitants, 73.5% of which corresponded to E. granulosus.5 In Spain it is a notifiable disease, hence the data compiled by the Red Nacional de Vigilancia Epidemiológica [National Epidemiological Surveillance Network] between 1985 and 2018 point to a progressive decrease in incidence due to disease control and eradication programmes, falling from 2.52 cases/100,000 inhabitants to 0.15 cases/100,000 inhabitants.6 Currently, there is a vaccine for cattle based on the recombinant EG95 antigen which seems to provide a high degree of protection.7,8
The biological cycle occurs between the dog or other canids, which act as the definitive host, and the intermediate host, which includes sheep, cattle and goats, among others. This infection in humans occurs through the ingestion of water or food contaminated with cestode eggs. In Spain, transmission occurs mainly between dogs, sheep and humans. Once ingested, the egg hatches, releasing the oncosphere, which is a larval stage of the cestode. This larva crosses the intestine until it reaches the blood vessels, settling in any organ or tissue and developing the hydatid cyst.1,8 Structurally, it is comprised of different layers; from the outside to the inside, there is the pericyst, the laminated layer and the germinal layer, where the daughter vesicles are produced.2 The most frequently affected organs are the liver (59%–75%) and the lung (8%–43%); brain involvement is only observed in only 1%–2% of cases.3 The most common location within cerebral echinococcosis is the hemispheres (90%–95%). It has been calculated that the growth rate of brain cysts exceeds that of liver cysts by a ratio of 3:1; this difference is facilitated by their being surrounded by a compressible organ.9 Cerebral echinococcosis has been described mainly in the paediatric population (50%–75%), characterised by the presence of single cysts which are generally unilocular.3 However, this case presents as a multilobulated lesion with multiple locations in an adult patient. Multifocal dissemination can be attributed to fistula formation from spontaneous or iatrogenic ruptures, leading to secondary cysts.9,10
Generally, hosts remain asymptomatic for years until complications emerge. Symptoms vary according to location, the most common ones being headaches and vomiting (87%) and hemiparesis (30%). Other less common symptoms are visual disturbances, cerebellar ataxia, aphasia and seizures.11 Adjacent organs may also become involved due to mechanical compression, and in the case of rupture it can trigger the appearance of fever, eosinophilia, urticaria, dissemination and, as a more serious presentation, anaphylactic shock (1%–7.5%).10
The diagnosis of human echinococcosis is based on clinical-epidemiological criteria, imaging techniques and microbiological studies.2 Although its distribution is universal, some geographical areas are endemic, in which case, in patients from Central Asia, North and East Africa, Australia, South America and the European Mediterranean basin, thus reinforcing the need to maintain a high degree of suspicion.12 Porencephalic and arachnoid cysts, tumours and other cysts of infectious origin (abscesses, neurocysticercosis) can be confused with hydatid cysts, hence it is important to make a proper differential diagnosis. Porencephalic and arachnoid cysts are not spherical and are not completely surrounded by cerebral matter. Tumour cysts present soft tissue, which is enhanced by contrast. And, finally, in other cysts of infectious cause, as in the case of abscesses produced by bacteria such as Streptococcus pyogenes, cerebral oedema and satellite lesions would appear. However, there are times when preoperative differentiation is truly complicated, as is the case of neurocysticercosis.9,11,13,14
The imaging study consists of CT and MRI, which are the main techniques used in cerebral involvement. There is also the possibility of performing a conventional radiograph, although with this technique it will only be possible to detect the presence of calcified cysts, which appear in approximately 1% of cases.15 In the CT and MRI examination, cysts classically have a spherical, occasionally ovoid appearance with a clear, soft and elastic wall and internal fluid whose density resembles that of cerebrospinal fluid. They are also characterised by not being enhanced following the injection of contrast or being associated with perifocal oedema.9,15 The World Health Organization establishes a classification whereby it classifies cyst stage according to its activity and thus assist in the choice of therapeutic strategy and follow-up. This classification is used mainly in cases of hepatic echinococcosis, where the diagnosis can be made by abdominal ultrasound.2
In microbiological diagnostic studies, microscopy provides confirmation of the aetiological agent. Visualisation of the hydatid fluid permits the observation of prolific vesicles, protoscolices and hooks.16 However, doing so entails a high risk of extravasation and the consequent risk of anaphylaxis if it is not extracted once the cyst has been removed, and direct acquisition is therefore restricted to specific cases.17 Additionally, immunodiagnostic tests are available, which not only support the resolution of the diagnosis but can also be used in post-treatment follow-up.18 Among the techniques currently on the market, particular mention may be made of enzyme-linked immunosorbent assays (ELISA), indirect haemagglutination, latex agglutination and inmunoblot. Techniques based on immunochromatography, immunofluorescence and immunoelectrophoresis (double diffusion arc-5) are also available. Antigens have traditionally been acquired from hydatid fluid, although the use of this complex mixture of parasite-derived proteins presents limited specificity and sensitivity. Currently, recombinant proteins or synthetic peptides of antigens derived from hydatid fluid, particularly Ag B and Ag 5 lipoproteins, are used in multiple marketed tests due to their high immunogenicity.7,18 Other antigens under study with serodiagnostic potential are those obtained from somatic extracts or excretory-secretory products of protoscolices and adults.19 All these serological tests have highly variable sensitivity and specificity, since they depend above all on the origin, purity and quality of the antigen extract used, the affected organ, the number of cysts and the disease's evolutionary stage.2,20 In the specific case of brain cysts, the antibody response is low or null, and is positive in less than 10% of cases.11 However, in other involvements, such as the liver and lung, sensitivity can increase to 100% according to some studies.7,18 It is important to rule out possible false positives due to cross-reactions with other helminths, such as E. multilocularis or Taenia solium, in some types of cancer and in the presence of liver cirrhosis.2,7 Currently, few publications have examined the sensitivity and specificity of the different serological techniques on the market versus sera specifically from patients with cerebral echinococcosis due to their low reactivity. With regard to detection using molecular biology techniques, such as the polymerase chain reaction, use is relegated to research laboratories or some third-level centres. It is largely applicable to the molecular characterisation of genotypes.16
Treatment is based on surgery, the PAIR drainage technique (puncture, aspiration, injection and reaspiration) or chemotherapy with benzimidazoles (albendazole, mebendazole). The most beneficial option will be selected, depending on clinical situation and cyst stage.21 In the case of brain cysts, the first therapeutic option is surgery with intact removal of the cyst using the Dowling technique, followed by treatment with anthelmintic drugs. This combination has proven its effectiveness although it can also be administered prior to the operation when the aetiological agent is known. Albendazole is the most widely used benzimidazole due to its greater absorption and bioavailability at a dosage of 10 mg/kg/day for a minimum of one month.15,21 In operations with cyst rupture, the procedure of choice will be rapid aspiration of the cystic content and washing of the surgical bed with hypertonic saline solution. The post-surgery mortality rate is between 10% and 12%.13 The drainage technique is relegated to inoperable cysts or non-responsive recurrences. This consists of the puncture and aspiration of the internal content and the subsequent injection of hypertonic saline combined with 95% ethanol and reaspiration. Other combinations can be used as scolicidal agent.21
Brain echinococcosis is an uncommon serious condition and it should be considered in the presence of consistent cystic brain lesions. Currently, imaging techniques together with microbiological tests play a fundamental role in guiding diagnosis, and microscopy is a crucial tool for obtaining aetiological confirmation, particularly in the case of brain involvement.
Conflicts of interestThe authors have no conflicts of interest to declare.