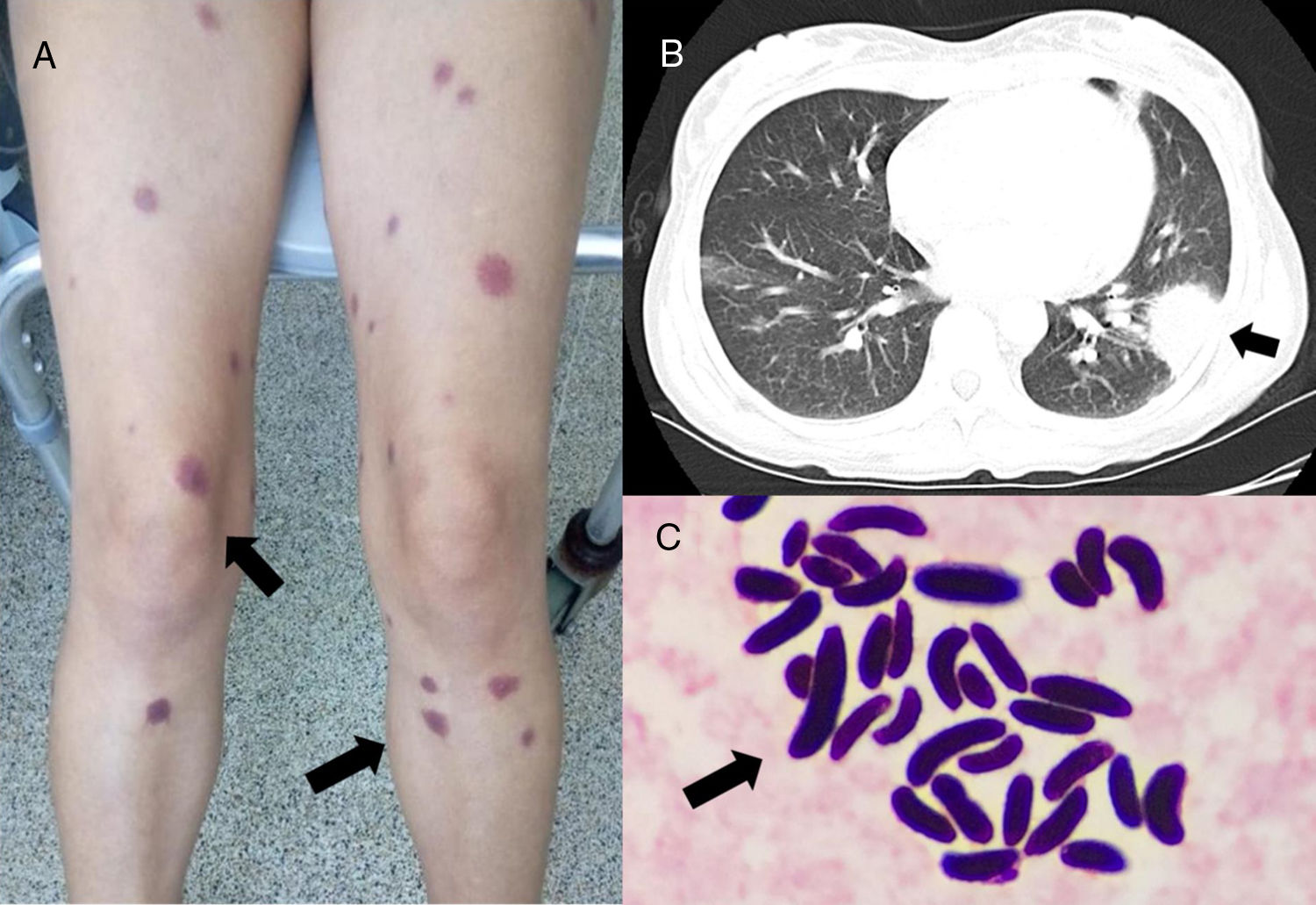
A 32-year-old Colombian woman was hospitalised with a diagnosis of acute myeloid leukaemia for administration of induction chemotherapy with idarubicin and cytarabine. After finishing the first cycle of chemotherapy, she presented febrile neutropenia and grade 1 mucositis. Blood cultures were negative. She received piperacillin/tazobactam and improved. Seven days later, she once again presented with febrile neutropenia, cough, nasal secretion, pain in the paranasal sinuses, generalised myalgia and exanthema in the form of round violaceous macules on the lower limbs and trunk (Fig. 1A). Blood cultures were taken again and treatment was started with meropenem and vancomycin, with no improvement. The patient underwent a chest X-ray and then a computed tomography scan of the chest which showed a consolidation in the left upper lobe with no halo sign or cavitation (Fig. 1B). A computed tomography scan of the paranasal sinuses showed bilateral ethmoid maxillary sinusitis with perforation of the septum. The patient was not receiving antifungal prophylaxis. Due to these findings, an invasive fungal infection was suspected and treatment was started with voriconazole 6 mg/kg every 12 h for the first 24 h and then 4 mg/kg every 12 h, and liposomal amphotericin B at 3 mg/kg/day. The laboratory reported growth in blood cultures and the Gram stain showed the structures presented in Fig. 1C.
Clinical, radiological and microbiological findings. A. Skin lesions in the form of round violaceous macules on the lower limbs. B. Computed tomography of the chest: consolidation in the left upper lobe with no halo sign and no cavitation. C. Gram stain of blood cultures: round and oval structures consistent with macroconidia.
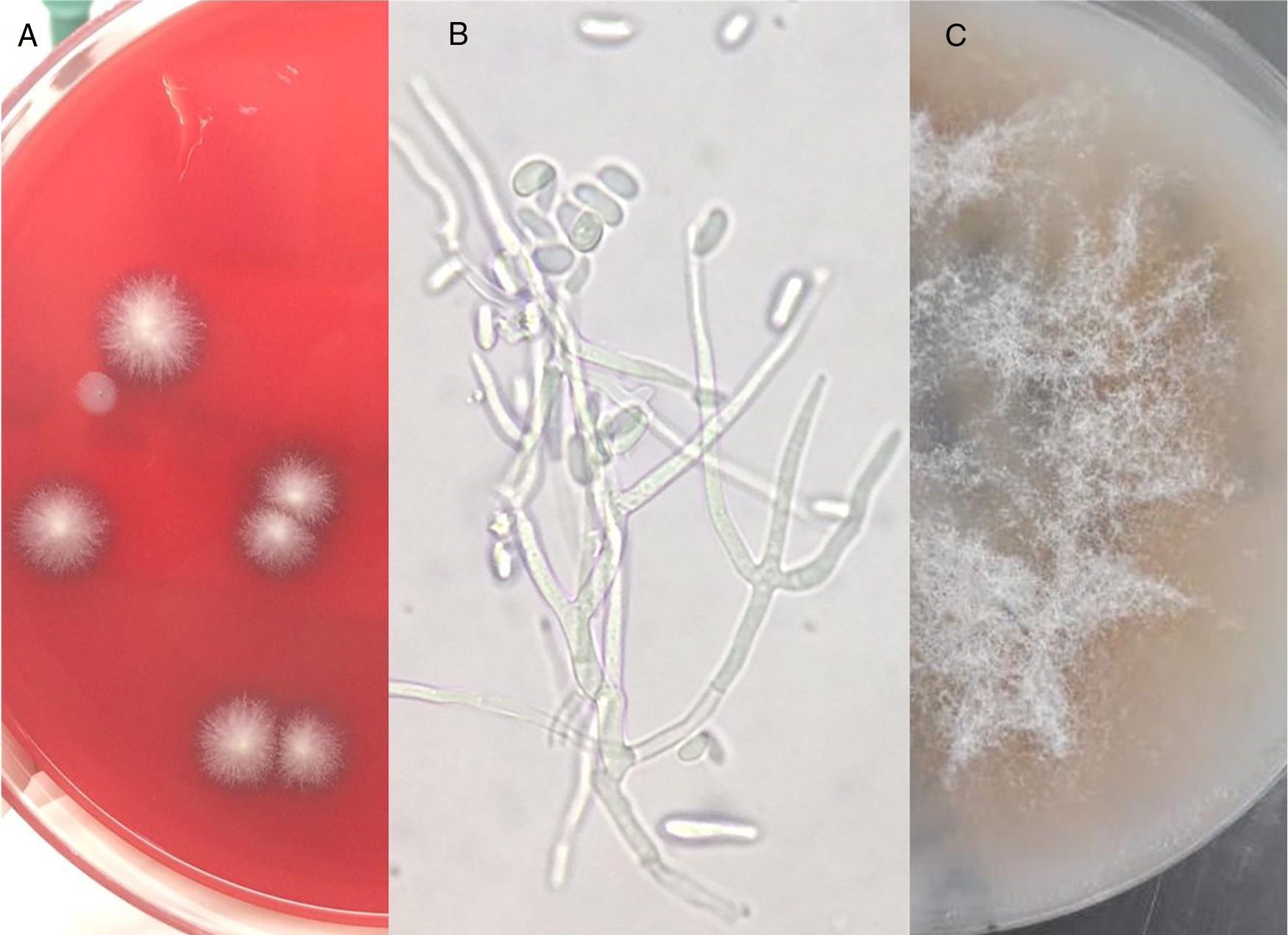
Our centre lacks techniques for galactomannan and 1,3-®d-glucan detection; therefore, they were not used. Skin biopsies were not taken either. Round, white, flat and hairy colonies grew in a blood agar medium (Fig. 2A), and a stain with KOH showed hyaline septate hyphae with branching at an acute angle (Fig. 2B). A differential diagnosis was established between Aspergillus spp., Fusarium spp. and Scedosporium spp., since wide hyaline hyphae with 90° branching are typically seen in mucormycosis.1 The isolate was sent to a reference laboratory (Corporación para Investigaciones Biológicas [Corporation for Biological Research], in Medellín, Colombia), where it was confirmed to correspond to Fusarium spp. (Fig. 2C). The patient showed recovery from neutropenia, and her fever and skin lesions disappeared. A decision was made to complete 6 weeks of antifungal treatment and then continue with voriconazole for a year.
Macroscopic and microscopic findings. A. Blood agar: hairy, flat, white and round colonies. B. Preparation with KOH of the blood agar plate: hyaline septate hyphae with branching at an acute angle and macroconidia are observed. C. Oatmeal agar: greyish-white colonies with a smooth and cottony appearance.
This case presented the typical clinical signs of an invasive fungal infection caused by Fusarium spp.; the finding of macroconidia on the Gram stain of the blood cultures supported this diagnosis. Fusarium spp. and Scedosporium spp. cause intravascular sporulation and skin lesions, and blood cultures are usually positive in both cases but more commonly in infections due to Fusarium spp. Infection with Fusarium spp. presents with myalgia in up to 15% of cases and examination under a microscope reveals macroconidia in the shape of a banana,2 typical findings in our case. Although invasive sinusitis occurs in infections due to Aspergillus spp. and zygomycetes, their clinical behavior is more serious and rapidly progressive; furthermore, Aspergillus spp. rarely presents with positive blood cultures.3
Patients with haematological malignancies are at higher risk of invasive fungal infection due to filamentous fungi and the incidence is highest in patients with acute myeloid leukaemia. In these cases, soft tissue involvement may be a sign of infection with Pseudomonas aeruginosa (ecthyma gangrenosum), Staphylococcus aureus or filamentous fungi such as Aspergillus spp., zygomycetes and Fusarium spp.,4 or due to a non-infectious aetiology such as drug reactions, Sweet's syndrome, erythema multiforme or leukaemia cutis. The presence of skin lesions in a "bull's-eye" pattern may lead to consideration of a diagnosis of disseminated fusariosis.1 Invasive scedosporiosis is also accompanied by non-pruriginous, erythematous and nodular skin lesions, with a necrotic centre.5
Invasive fusariosis is a rare disease, with an incidence of 0.1%, but a high mortality rate, up to 53%.6 Fungaemia is a distinctive characteristic of invasive fusariosis compared to other opportunistic infections caused by fungi. Prompt identification is required to quickly start treatment with effective antifungal agents (voriconazole, amphotericin B or posaconazole), although rates of clinical response are modest.7 We wish to stress the importance of collaboration with the microbiology laboratory and morphological analysis of fungi, which are necessary for differential diagnosis and appropriate treatment in patients with prolonged febrile neutropenia.
We would like to thank the Oncólogos de Occidente [Western Oncologists] health institution.
Please cite this article as: Hoyos-Pulgarín JA, Arias-Ramos D, Gonzalez-Diaz JA, Ramirez NM. Hallazgo inusual en la tinción Gram de hemocultivos en una paciente con neutropenia febril prolongada y leucemia mieloide aguda. Enferm Infecc Microbiol Clin. 2020;38:338–340.