The re-emergence of pertussis and the severity of its complications in infants younger than 3 months were determining factors for starting a vaccination program for pregnant women in the third trimester of gestation in Catalonia in February 2014. This was the first autonomous community to introduce it in Spain. The aim of the study was to estimate the coverage of the program in its first year of implementation.
MethodsA retrospective analysis was performed on the data from the Primary Care Centre computerised medical records of pregnant women attending Sexual and Reproductive Health Care centres of the Metropolitan Nord area of the province of Barcelona, part of the Catalan Institute of Health. The overall coverage was estimated, as well as the sociodemographic variables of Tdap vaccination of women who had registered a delivery of a live birth between August 2014 and August 2015.
ResultsA total of 6697 deliveries of live births were recorded, and 1713 pregnant women were vaccinated, which represented an overall coverage of 25.6% (95% CI; 24.1–26.1). Vaccination coverage was higher in pregnant women under 18 years and Spanish women (p=0.018 and p=0.036, respectively).
ConclusionThe estimation of vaccine coverage against pertussis in pregnant women in the third trimester of pregnancy, after the first year of implementation of the program in a health area of Catalonia was lower than the objective set. Strategies need to be designed in order to improve program coverage.
La reemergencia de la tos ferina y la gravedad de sus complicaciones en lactantes menores de 3 meses de edad determinó el inicio del programa de vacunación de las mujeres embarazadas en el tercer trimestre de gestación, en Cataluña en febrero del 2014, la primera comunidad autónoma que la introdujo de España. El objetivo del estudio fue estimar la cobertura del programa en su primer año de implementación.
MétodosSe analizaron de forma retrospectiva los registros médicos informatizados de los Centros de Atención Primaria de embarazadas atendidas en centros de Asistencia de Salud Sexual y Reproductiva del área Metropolita Nord de la provincia de Barcelona, dependientes del Institut Català de la Salut. Se estimó la cobertura global y según variables sociodemográficas de vacunación con dTpa de las mujeres que tenían registrado un parto de un recién nacido vivo entre agosto del 2014 y agosto del 2015.
ResultadosSe registraron 6.697 partos de nacidos vivos y 1.713 mujeres embarazadas fueron vacunadas, lo que representó una cobertura global del 25,6% (IC del 95%: 24,1-26,1). La cobertura de vacunación fue mayor en las mujeres embarazadas menores de 18 años y las nativas (p=0,018 y p=0,036, respectivamente).
ConclusiónLa estimación de cobertura vacunal frente a tos ferina de embarazadas en el tercer trimestre de gestación, tras el primer año de implementación del programa en un área sanitaria de Cataluña, ha resultado inferior al objetivo marcado. Será necesario diseñar estrategias dirigidas a mejorar la cobertura del programa.
Pertussis is a highly contagious infectious diseases, which has been re-emerging in recent years in most countries and causing high morbidity and mortality.1 In most cases the severity of pertussis and its complications in infants requires hospitalisation and the death rate is high.2,3 Vaccination is the best form of prevention, but the immunity conferred by presenting the disease and by vaccination is of limited duration. In Catalonia, the calendar of systematic vaccinations offers 5 doses of the vaccine (at 2, 4, 6 and 18 months and a booster dose at 4–6 years) with a diphtheria, tetanus and acellular pertussis component since 2002.4
The re-emergence of pertussis, with major outbreaks in many countries, such as those in California and England, and causing a notable increase of deaths in infants under the age of 3 months, has led to the introduction of new prevention and control strategies.5 Contact studies6,7 show that parents and household members are the principal sources of contagion to infants who have not yet their started primary vaccination course. It is now suggested that pregnant women in the third trimester should be vaccinated as the most effective and efficient strategy to protect newborns who have not yet started primary vaccination. This strategy has been shown to be safe and effective in preventing other infectious, vaccine-preventable diseases, such as tetanus or flu.8 The transfer of antipertussis antibodies to the foetus via the placenta will protect the neonate until vaccination starts at 2 months old. The mother will also be protected, which will also provide indirect protection to the newborn child. One single intervention will protect mother and newborn without increasing the risk of adverse effects.9
In a recent study in Catalonia,10 more than 94% of the children of mothers who were given a dTpa vaccine dose during the second or third trimester of their pregnancy presented higher levels of antibodies than those of the mothers who were not.
The programme for vaccinating pregnant women with one dose of dTpa between gestation weeks 27–36 was introduced in the United States in October 2011. Vaccine coverage in 2012 was less than 20%,11 and only 25% of the pregnant women who gave birth in 100 hospitals in California in October 2013 were given a dose of dTpa during pregnancy.12
Vaccinating pregnant women between gestation week 28 and 38 was recommended in October 2012, and achieved 64% coverage in the first year it was implemented.13 The effectiveness of maternal vaccination in preventing pertussis in children under the age of 2 months has been estimated at 91%.14
In Spain, the incidence of pertussis increased from 1.9 cases per 100,000 inhabitants in 2010 to 7.17 cases per 100,000 inhabitants in 2014.15 In children under one year, the incidence reached 226.58 cases per 100,000 inhabitants in 2014.16 The hospitalisation rate for pertussis did not exceed 100 hospitalisations per 100,000 children under one year of age up until 2000. However, from 2011, there were more than 200 hospitalisations per 100,000 in the majority of the autonomous communities.15 In Catalonia, the overall incidence rate was 13.5 cases per 100,000 inhabitants in 2014.17 In the period from 2000 to2013 there were 40 deaths among the cases notified, of 39 of which were children under the age of one year.15 This situation prompted consideration of the need to implement additional vaccination strategies.18
The programme for vaccinating pregnant women was started in Catalonia in February 2014. Catalonia was the first autonomous community to introduce this. The objective was to achieve 50% vaccination coverage in the first year. Information was provided via information sessions, and technical guidelines and information material was given out to the healthcare professionals involved in monitoring the pregnant women. All the professionals involved in prenatal care, midwives and obstetricians, received information on the recommendation to vaccinate expectant mothers in each pregnancy, ideally between gestation weeks 27 and 36.18
Because there is no official registry to enable monitoring of the vaccination coverage of pregnant women, we considered it appropriate to use indirect information sources, such as the electronic health records registries available in the sexual and reproductive health centres (ASSIR). The objective of this study was to estimate coverage of the programme in its first year of implementation to assess whether additional strategies are required to improve results.
MethodsData was analysed retrospectively from the computerised clinical record registries of primary care centres (e-CAP) of pregnant women who attended the 7 ASSIR centres of the province of Barcelona's North Metropolitan Area, which is under the authority of the Catalan Health Institute (ICS). This area includes the 1,383,039 inhabitants of the 71 municipalities of Vallés Occidental, el Vallés Oriental, el Barcelonés and el Maresme. The population of the health area studied is spread over a large geographical area with includes large metropolitan as well as small rural areas, with a proportion of women of fertile age similar to that of the population of Catalonia.19 During 2014, a total of 18,338 deliveries were recorded in this health area, of which 14,336 (77.7%) took place in Integrated Public Use Healthcare System of Catalonia (SISCAT) hospitals and the remainder in private hospitals. Eleven thousand, four hundred and forty-one expectant mothers were monitored in the area's ASSIR centres, but information was available for only 6697 live births (58.5%) to mothers who attended the postnatal monitoring visit.
The women's clinical records are electronically registered using e-CAP. Eighty percent of the population of Catalonia are allocated a primary care centre that uses e-CAP.20 Patients attended in centres not under the authority of the ICS were not included. The socio-demographic data were collected for all of the patients, information on each ante-natal visit and their vaccination record. The ante-natal checks were performed by midwives following Catalonia's protocol for monitoring pregnancy.21 The pregnant women had to have been informed of the new pertussis vaccination protocol during antenatal classes, and at consultations, in order to receive the vaccine between weeks 27 and 36 of their pregnancy. The midwives themselves or the primary care nurses were in charge of giving the vaccination and completing the records, as organised by each centre.
The overall DTPa vaccination coverage was estimated of women registered as having delivered a live newborn between August 2014 and August 2015, during which time all the centres had all the available resources to implement the programme. The variables analysed were the mother's age at the beginning of the pregnancy, her place of origin, level of education (no schooling, primary, secondary or university), number of previous children, date of labour and date of pertussis vaccination. Vaccination coverage was estimated according to the mother's demographic variables. The statistical analyses were performed using SPSS 22.0 for Windows, version 22.0. (SPSS Inc., Chicago, U.S.A.).
The Clinical Research Ethics Committee of the Primary Care Research Institute Jordi Gol assessed and approved the project.
ResultsBetween August 2014 and August 2015, 6697 deliveries of live births were recorded from mothers who attended the post-natal visit in the North Metropolitan Area of Barcelona. The mean age of the women at time of delivery was 30.8 (SD: 5.5) years. Five point four percent of the pregnant women were aged under 18 years or over 40. Sixty-five point six percent were of Spanish origin and 96.6% had some form of education.
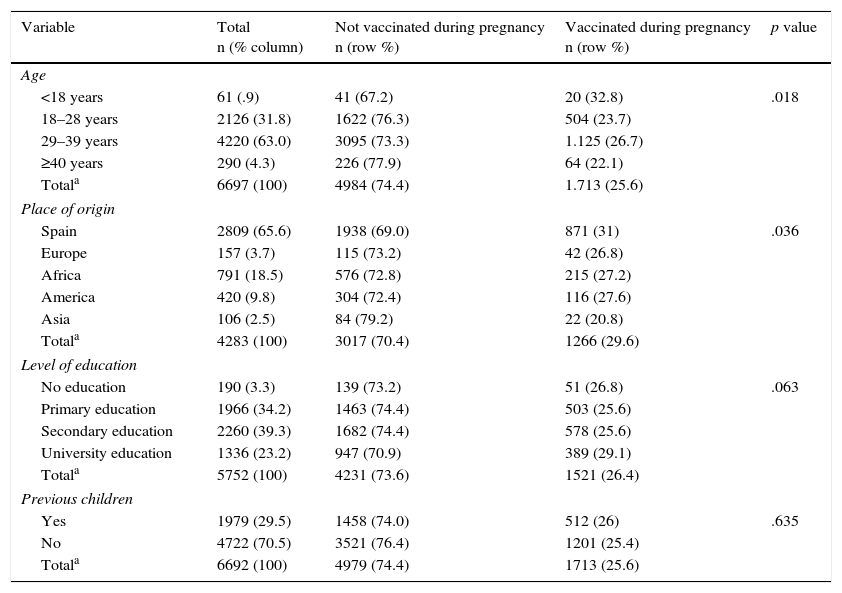
The demographic characteristics of the population studied and the vaccination coverage according to age group, place of origin, level of studies and parity are shown in Table 1.
Distribution of the socio-demographic variables of the population studied.
| Variable | Total n (% column) | Not vaccinated during pregnancy n (row %) | Vaccinated during pregnancy n (row %) | p value |
|---|---|---|---|---|
| Age | ||||
| <18 years | 61 (.9) | 41 (67.2) | 20 (32.8) | .018 |
| 18–28 years | 2126 (31.8) | 1622 (76.3) | 504 (23.7) | |
| 29–39 years | 4220 (63.0) | 3095 (73.3) | 1.125 (26.7) | |
| ≥40 years | 290 (4.3) | 226 (77.9) | 64 (22.1) | |
| Totala | 6697 (100) | 4984 (74.4) | 1.713 (25.6) | |
| Place of origin | ||||
| Spain | 2809 (65.6) | 1938 (69.0) | 871 (31) | .036 |
| Europe | 157 (3.7) | 115 (73.2) | 42 (26.8) | |
| Africa | 791 (18.5) | 576 (72.8) | 215 (27.2) | |
| America | 420 (9.8) | 304 (72.4) | 116 (27.6) | |
| Asia | 106 (2.5) | 84 (79.2) | 22 (20.8) | |
| Totala | 4283 (100) | 3017 (70.4) | 1266 (29.6) | |
| Level of education | ||||
| No education | 190 (3.3) | 139 (73.2) | 51 (26.8) | .063 |
| Primary education | 1966 (34.2) | 1463 (74.4) | 503 (25.6) | |
| Secondary education | 2260 (39.3) | 1682 (74.4) | 578 (25.6) | |
| University education | 1336 (23.2) | 947 (70.9) | 389 (29.1) | |
| Totala | 5752 (100) | 4231 (73.6) | 1521 (26.4) | |
| Previous children | ||||
| Yes | 1979 (29.5) | 1458 (74.0) | 512 (26) | .635 |
| No | 4722 (70.5) | 3521 (76.4) | 1201 (25.4) | |
| Totala | 6692 (100) | 4979 (74.4) | 1713 (25.6) | |
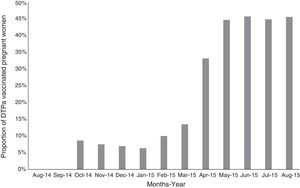
One thousand seven hundred and thirteen pregnant women were vaccinated, which is an overall coverage of 25.6% (95% CI: 24.1–26.1). Vaccination coverage per month varied throughout the study period, the mean was 8.6% (95% CI: 2.9–19.0) in the first 3 months of the study and 44.9% (95% CI: 41.0–48.9) in the final months of the study (Fig. 1).
The vaccine was given between gestation weeks 27 and 36 to 1680 (98%) of the pregnant women who were vaccinated. In 67 cases the vaccine was given at less than 2 weeks before delivery, of which 31 (46.3%) were premature deliveries (at less than 37 weeks’ gestation).
Sixty-five point seven percent of the pregnant women vaccinated were aged between 29 and 39 years, 68.8% were of Spanish nationality and 96.6% had education.
Per age group, the pregnant women vaccinated to the greatest extent were aged less than 18 years (32.8%) and those aged 40 years and above the least (22.1%). The difference between the groups was statistically significant (p=0.018).
According to place of origin, the pregnant women from Asian countries had the lowest coverage (20.8%), the difference was significant from those of other origins (p=0.036).
A greater proportion of the pregnant women with university education were vaccinated (29.1%) although the differences per level of education were not significant (p=0.088). Neither were the differences between those with previous children and primiparous mothers.
DiscussionThis study is the first publication that provides information on adherence to the pertussis vaccination programme by pregnant women in the first year of its implementation in Catalonia. The mean vaccination coverage with a dose of DTPa was 25.6% in the North Metropolitan healthcare area. A gradual increase in the number of pregnant women vaccinated from the beginning of the programme was observed, which reach 45% in the final months of the period analysed (50%).
The results contrast with the estimations of coverage presented in Catalonia by the Regional Ministry of Health (56%)22 and the Osona region (47.3%).23 In the community of Valencia in 2015, the first year of implementation of the vaccination of pregnant women, coverage was 84%.24
Vaccination coverage was also lower than that published in some countries where the DTPa vaccination programme for pregnant women has been implemented. In the United Kingdom between October 2012 and September 2013, vaccination coverage for pregnant women rapidly reached 60%.13 In Belgium,25 a mean coverage of 39% (95% CI: 33.2–45.6%) was achieved in the first quarter after implementation (from December 2013 to February 2014). Coverage of 14% was achieved in the U.S.A. between 2007 and 2013.26,27 However, in recent studies an increase in vaccinations of pregnant women with medical insurance has been observed. Thus, in Wisconsin,28 where public insurance covers the expenses of pregnancy for approximately 49% of pregnant women, vaccination coverage increased to 51% in March 2014.
Ninety-eight percent of the pregnant women were vaccinated between the gestation weeks established in the programme. Vaccination between gestation weeks 27 and 32 ensures coincidence with the highest level of maternal antibodies and most transplacental transfer, although the period can be extended until week 38.15 However, it was observed that in some cases the DTPa vaccine was given less than 2 weeks from the delivery date, and of these cases a major promotion were premature births. This group is one of the most vulnerable and therefore additional measures are necessary to protect them, such as complementing vaccination with the cocoon strategy.
Differences have been observed in vaccination coverage according to some demographic variables. A lower proportion of the pregnant women of Asian origin (the majority from China and Pakistan) were vaccinated than the rest. Differences in vaccination percentages according to the place of origin of the pregnant women have also been observed in previous studies in other countries. In the U.S.A. a greater proportion of pregnant women of white and Hispanic origin were vaccinated against pertussis than those of Afro-American, Asian and Arabic origin.26 In one hospital in the U.S.A. 60% fewer pregnant Afro-American women were vaccinated than women of other origins, followed by women of Asian origin.29 Differences in vaccination coverage were also seen in European countries between pregnant women of European origin and those of non-European origin.25 This same phenomenon has also been observed in studies on flu vaccination coverage in pregnant women.30,31 Linguistic differences and pregnant women's consequent lack of understanding of the vaccination information provided by healthcare professionals are a hypothetical cause put forward by some authors to explain this disparity.25
According to age, a greater proportion of the youngest expectant mothers were vaccinated in this study. These results differ from those presented by other authors where older mothers were vaccinated most against both flu and pertussis.25,28,31
The pregnant mothers with higher levels of education were vaccinated more than the rest, although the differences were marginally significant. This tendency has also been observed in other publications.25,31
There are few studies on the reasons why pregnant women do not get vaccinated. In a qualitative study,32 pregnant women claimed that they were more worried about the potential risk to their children's health than to their own. The mothers perceived influenza as a disease that affected them, while whooping cough was a threat to their children and of greater risk. Therefore, they were more likely to get vaccinated against pertussis than against influenza to protect their children. The perception of the efficacy of the vaccine and the likelihood of contracting the infection were also associated with the decision by the mothers to be immunised.33
The knowledge and attitude of healthcare professionals about vaccinating pregnant women might influence their decision to be immunised. In the U.S.A.34 pregnant mothers’ not being immunised against influenza is attributed to a lack of knowledge about its importance and an unfounded fear regarding its effect on their own health and that of the foetus. In a study performed in Australia,35 80% of the pregnant women surveyed said that they would be vaccinated against pertussis if recommended by their doctor. However, in this same study, 68% of the pregnant women claimed not to have received information on the post-partum pertussis vaccine, even though this strategy is recommended in Australia. It was observed in Turkey that the mothers who received information on immunisation were vaccinated more than those who did not.36
In the U.S.A., gynaecologists and obstetricians recommend vaccination if they have sufficient knowledge about the infection and the characteristics of the vaccine.37 This collective's reasons for not offering the vaccine are related with doubts about its safety, not perceiving vaccination as part of their job38 and problems in managing the costs involved in administering vaccines to adults.39
Midwives display a positive attitude to the vaccination of pregnant women.40 They consider that they are in an ideal position to give expectant mothers information and advice about immunisation and other public health-related issues, yet they flag up the lack of time, training and resources provided to do so.41
The population distribution in the geographical area studied is similar to that of the population of Catalonia. Therefore, it might be considered that the results can be extrapolated. It should be highlighted that a possible limitation of the study is that the results correspond only to the pregnant women attended in ICS centres and therefore shows no information on those attended by other healthcare providers or private centres. However, it is estimated that the ICS covers 80% of the Catalan population (approximately 5.8 million citizens) and that 70% are visited annually in their allocated healthcare centre.20 Another limitation is the quality of the computerised records. There is a lack of information for a significant amount of individuals on some socio-demographic variables, such as place of origin and level of education.
Midwives are the practitioners responsible for pregnancy monitoring and healthcare education of expectant mothers in our country. Further specific studies are necessary in our environment with a view to identifying the barriers to achieving greater coverage of pregnant women, since this is the strategy that offers the best protection to children less than 3 months old from serious infection and death from pertussis.
In conclusion, this study shows the estimated pertussis vaccination coverage of pregnant women in the third trimester of gestation in Catalonia after the first year of implementation of the programme in one healthcare area. The percentage of pregnant women immunised was lower than the target set, although a growing tendency was observed over the months. Therefore strategies need to be designed to overcome the limitations and improve coverage of the programme.
FundingThe study received no funding.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Fernández-Cano MI, Espada-Trespalacios X, Reyes-Lacalle A, Manresa Domínguez JM, Armadans-Gil L, Campins-Martí M, et al. Cobertura vacunal frente a tos ferina en gestantes de Cataluña en el primer año de implantación del programa de inmunización. Enferm Infecc Microbiol Clin. 2017;35:550–555.