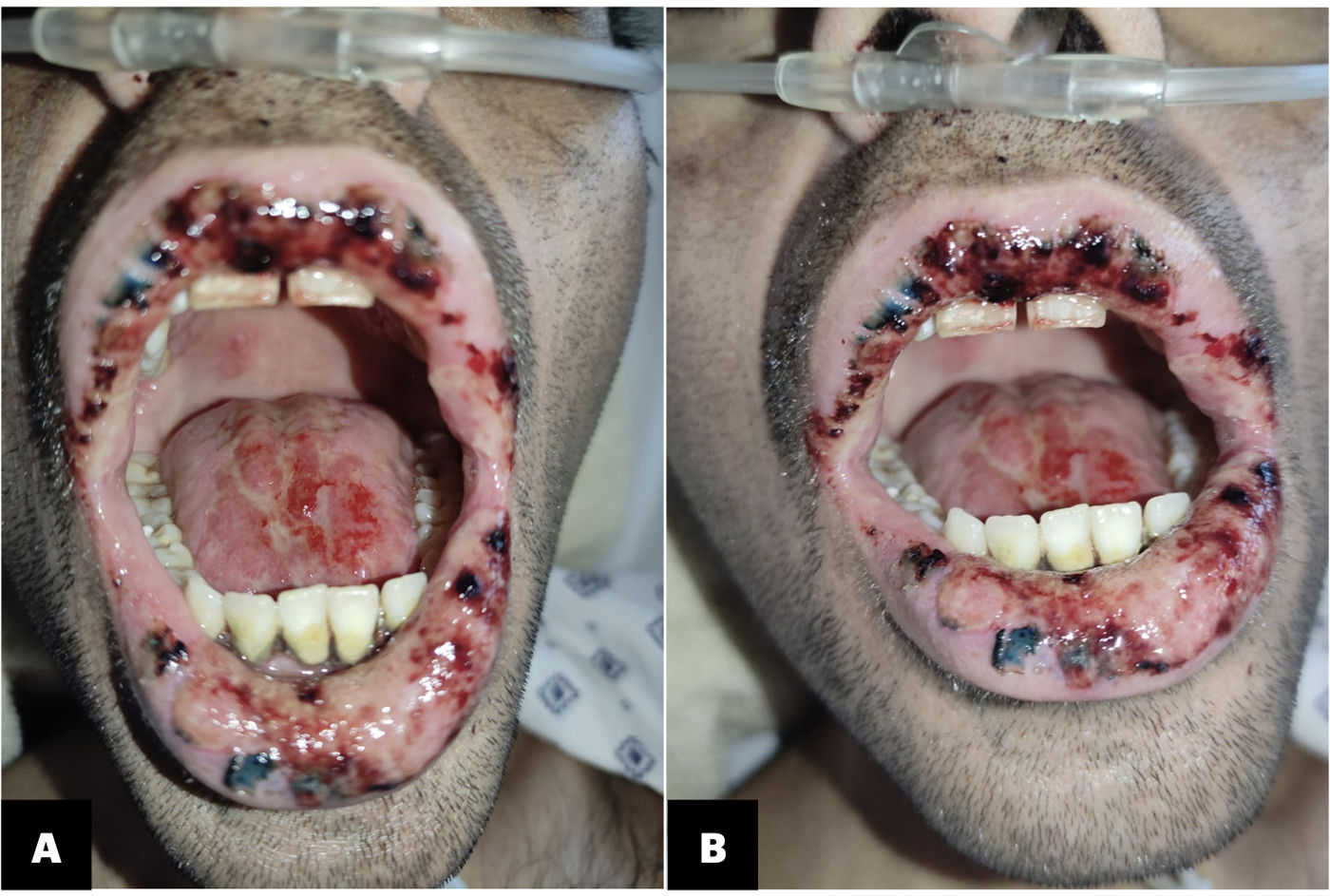
A 28-year-old male patient recently diagnosed with human immunodeficiency virus (HIV) infection and yet to commence antiretroviral therapy, was admitted to the hospital presenting with cough, fever, night sweats, and dyspnea. On initial physical examination, he had hepatosplenomegaly without adenopathies. Laboratory testing revealed pancytopenia, an HIV viral load of 9,900,423copies/ml, lymphocytes T-CD4+ count of 14cells/μL representing 2% of lymphocytes, and Pneumocystis jirovecii pneumonia (PJP) identified in bronchoalveolar lavage and treated with 15mg/kg of trimethoprim, and sulfamethoxazole. The patient tested negative for syphilis, Cryptococcus, histoplasma, and tuberculosis. After 1 week of admission, he developed stomatitis on both lips and the dorsum of the tongue, characterized by numerous painful ulcers with well-defined borders and bloody crusts (Fig. 1). Upon examination, papillary atrophy of the tongue was noted. No specific treatment was initiated based on the unusual lesions observed. The patient was transferred to our medical center for further investigation.
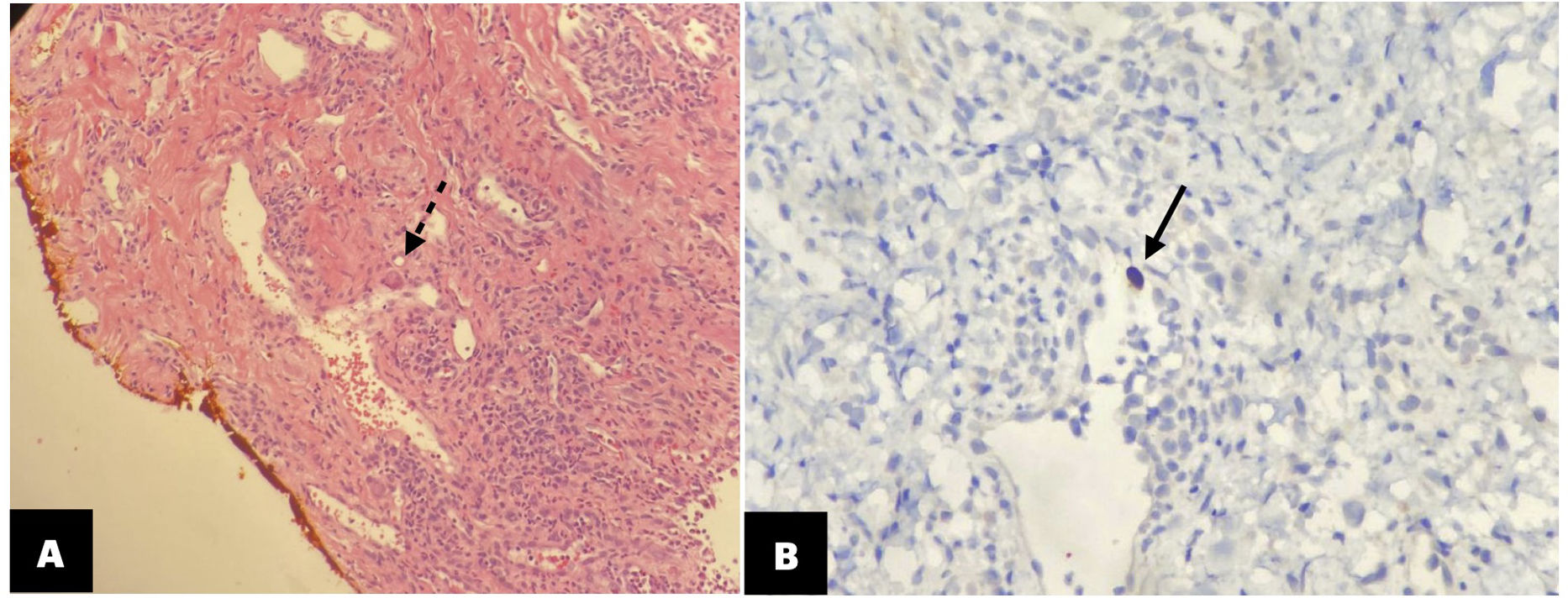
Diagnosis and evolutionThe differential diagnosis of the stomatitis included: infectious, metabolic, and drug-adverse events. A biopsy of the lower lip was performed, revealing a large intranuclear inclusion that was densely eosinophilic. Immunohistochemical reaction confirmed the diagnosis of Cytomegalovirus (CMV) infection (Fig. 2). No CMV viral load was done. Treatment with valganciclovir 900mg every 12h was initiated immediately. Antiretroviral therapy (ART) with bictegravir/tenofovir alafenamide/emtricitabine was started within two weeks for PJP and CMV treatment. After 3 weeks of treatment, the patient demonstrated significant improvement (Fig. 3). It was decided to treat the infection as an invasive Cytomegalovirus infection, despite the absence of demonstration in other tissues, due to the rare circumstances of this CMV infection manifestation, providing a total of 6 weeks of treatment. 4 weeks after the initiation of ART, HIV viral load was 11,801copies/ml demonstrating a reduction of >1log and there was an increased con lymphocytes T-CD4+ count of 84 (11%).
Skin biopsy. (A) Lip epithelium with hematoxylin and eosin stain showed the hallmark histologic feature of Cytomegalovirus infection with a large intranuclear inclusion densely eosinophilic (dotted arrow). (B) Immnohistochemical reaction confirming the presence of the virus (continuous arrow).
Cytomegalovirus (CMV) is a double-stranded DNA virus that is part of the Herpesviridae family. Seroprevalence could be as >90% in people living with HIV.1 CMV infection typically begins as a latent infection that can later reactivate, particularly among individuals with a compromised immune system. Its presentation may include nonspecific systemic diseases like pneumonia, colitis, esophagitis, gastritis, hepatitis, pancreatitis, retinitis and CMV-associated immune reconstitution inflammatory syndrome (CMV-IRIS).2 Cutaneous manifestations of CMV infection are exceedingly rare and may signal an unfavorable prognosis. Skin manifestations are not pathognomonic and can vary widely including purpura, petechiae, nodules, vasculitis, erythema, ulcers, and pustules. Among these, ulcers, as seen in our patient, are the most common and are predominantly found in perianal (18%) and oral (9%) regions.3 Fortunately, in the case of our patient the diagnosis was timely, which improved his prognosis.
One notable aspect of our case is the atypical presentation of the ulcers, which were exclusively confined to the exposed areas of the lips, initially resembling a chemical or solar burn, or even cutaneous manifestations of vitamin deficiencies. However, there were no environmental or dietary factors that could account for such a differential diagnosis.
Notwithstanding the rarity of CMV skin manifestations, they do not necessitate a different therapeutic approach. Ganciclovir and valganciclovir (IV or PO, respectively) remain the primary antiviral agents used to treat CMV infection.4 While deferring antiretroviral therapy (ART) until disease control may reduce the risk of CMV-IRIS, there is no consensus on this approach.5 Our patient did not experience any complications associated with the combination of ART and valganciclovir. Symptoms resolved within 3 weeks, consistent with findings reported in other case reports.3
Conflicts of interestThe authors declare no conflict of interest or have received any sponsorship.