The reasons for the decrease in blood cultures were investigated and the rate and aetiology of bacteremia and contaminated blood cultures collected from COVID and non-COVID patients were assessed.
MethodsWe performed a retrospective analysis in a tertiary hospital in Spain during the COVID period from 4th March 2020 to 21st June 2020.
ResultsThe number of blood cultures processed was 5313, representing 22.7% and 18.8% of decrease compared to the same months of 2019 and 2018, respectively (p=0.173). The rate of bacteremia was 1.2% higher among COVID-patients than among non-COVID patients (p<0.001). COVID patients had a higher proportion of nosocomial bacteremia (95.5%) than non-COVID patients (30.5%) (p<0.001). In COVID-positive patients, the contamination rate was 12.3% vs 5.7% in non-COVID patients (p<0.001).
ConclusionThere was a decrease in the number of blood cultures collected during the COVID period compared to previous years. Bacteremia in COVID patients was mainly nosocomial and catheter-related.
Investigar la causa de la disminución de los hemocultivos recibidos y evaluar la tasa y la etiología de la bacteriemia y la contaminación de los hemocultivos extraídos en pacientes con COVID-19 y sin COVID-19.
MétodosEstudio retrospectivo en un hospital de tercer nivel en España durante el periodo de COVID-19 del 4 de marzo al 21 de junio de 2020.
ResultadosSe procesaron 5.313 hemocultivos, representando una disminución del 22,7 y 18,8% respecto de los mismos meses de 2019 y 2018 (p = 0,173). La tasa de bacteriemia fue 1,2% superior en pacientes con COVID-19 (p < 0,001). Los pacientes positivos en COVID-19 tenían una mayor proporción de bacteriemia nosocomial (95,5%) que los pacientes sin COVID-19 (30,5%) (p < 0,001). En pacientes positivos en COVID-19, la tasa de contaminación fue del 12,3 vs. 5,7% en pacientes sin COVID-19 (p < 0,001).
ConclusiónDurante el periodo de COVID-19 disminuyó el número de hemocultivos recibidos, en comparación con años anteriores. La bacteriemia en pacientes con COVID-19 fue principalmente nosocomial y se asoció con el catéter.
The first patient in Spain with novel coronavirus SARS-CoV-2 infection was reported on January 31st: a German tourist who had been in contact in his country with a patient diagnosed with coronavirus.1 In our Autonomous Community, Aragón, the first COVID-positive was detected on March 4th.
Patients with suspected infection usually show symptoms such as a fever over 38.5°C, dry cough, shortness of breath and diarrhoea.2 In patients presenting severe febrile illness, blood cultures are still essential in ruling out bacterial infection.
The objectives of this work are to quantify the number of blood cultures received, and to investigate the rate and aetiology of bacteremia and contaminated blood cultures collected from COVID and non-COVID patients.
MethodsStudy designA retrospective cohort study was conducted on patients with blood cultures performed at Miguel Servet University Hospital in Zaragoza, Spain from 4th March to 21st June, 2020. Corresponding data from the same period in 2018 and 2019 were collected to establish a seasonal historic baseline of blood culture ordering.
Laboratory methodsBlood cultures were incubated on BD BACTEC™ FX during 5 days. When a positive blood culture was detected, a Gram stain and identification by mass spectrometry (MALDI-TOF MS) (MaldiBiotyper® Bruker Daltonics) of the subculture was performed.
Samples used for the determination of COVID-19 consisted mainly in nasopharyngeal swabs. For RNA targeting, VIASURE (CerTest, BIOTEC, Spain), Allplex™ (Seegen, Korea) and COBAS 6800tm (Roche, Switzerland) were used mainly.
Data analysisBlood withdrawals were grouped into three groups, depending on the year of extraction (2018, 2019, or 2020). The origin of withdrawals was also taken into account, grouping them into four categories (medical wards, surgical wards, ICUs and emergency departments). Further analysis was done in the specific case of the Emergency Department, where the number of patients admitted during the years 2018, 2019, and 2020 was accounted.
Blood culture contamination was defined as the presence of one or more of the following organisms found in only one blood culture set and only one of a series of two or three blood culture sets: coagulase-negative staphylococci, Micrococcus spp., viridans group streptococci, Propionibacterium acnes, Corynebacterium spp. and Bacillus spp.3
Finally, a review of clinical data in COVID-positive and COVID-negative patients with bacteremia was done.
All data analysis was performed with IBM SPSS 19. Differences in continuous data between groups were assessed by one-way analysis of variance (ANOVA), whereas categorical data were analyzed by Pearson's χ2 analysis.
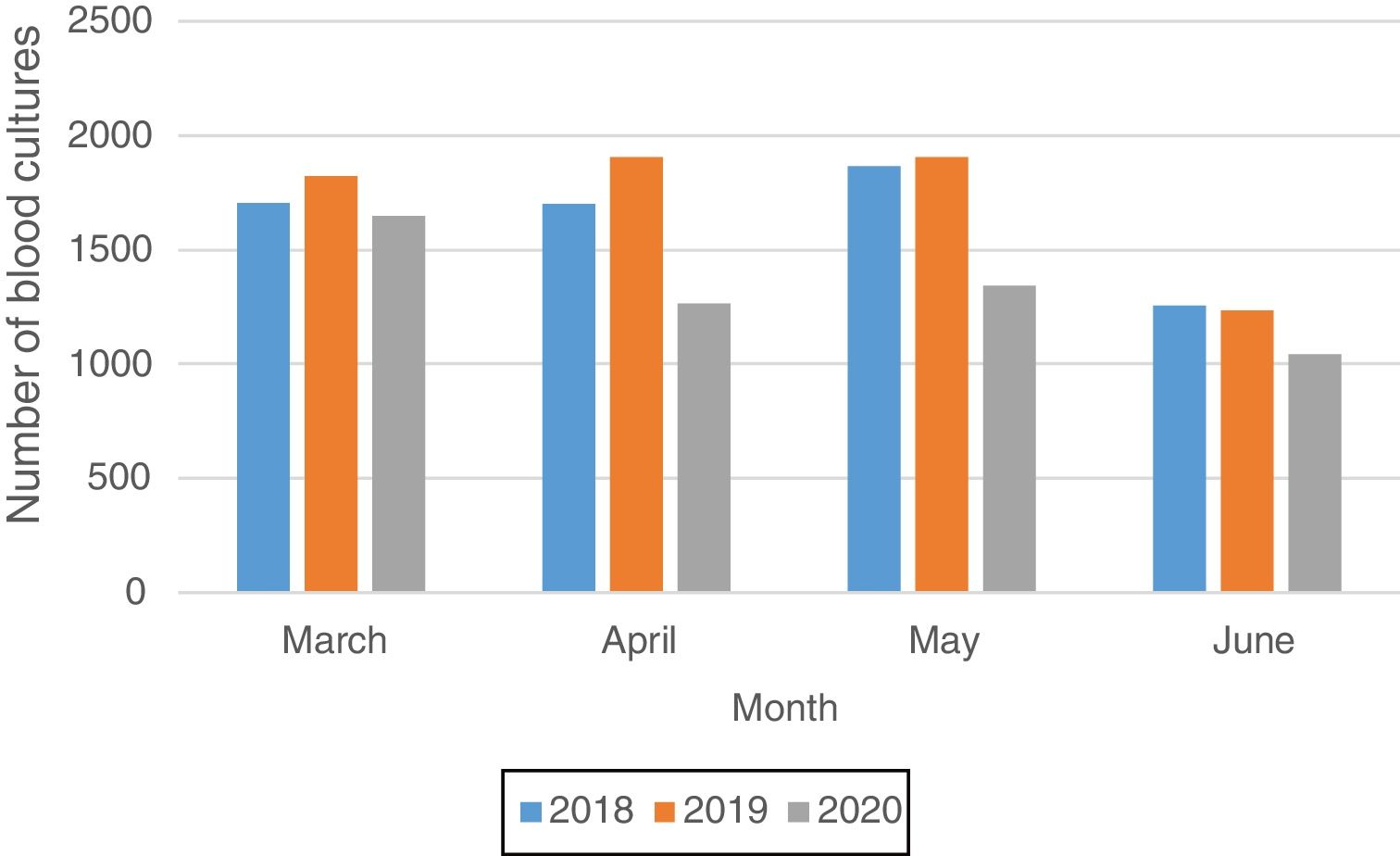
ResultsNumber of blood cultures setsThe number of blood cultures processed during the study period was 5313 in 2020, 6876 in 2019 and 6541 in 2018, representing 22.7% and 18.8% of decrease, respectively (p=0.173). Fig. 1 shows the number of blood cultures processed by month from 4th March to 21st June during 2018, 2019 and 2020.
With regard to requesting services, the adult Emergency Department showed a decrease in the number of blood cultures sets of 35.5% and 12.3% compared to 2019 and 2018, respectively (p=0.044). In surgical wards the decrease was 35% and 36.4% (p=0.054), and in medical wards the decrease was 20% and 28.3% (p=0.091). On the other hand, the increase in the intensive care units were 10.5% and 3.2% compared to 2019 and 2018 (p=0.738) and in Children's Emergency Department the increase was 32.4% and 35.8% (p=0.021).
In the specific case of adult Emergency Department, the number of patients who went to this department was 24980 in 2020, 43580 in 2019 and 41656 in 2018, representing a decrease of 42.7% and 40%, respectively (p=0.005).
COVID positivity rateDuring the study period, 2923 patients tested positive (9.1%) for COVID and 29314 patients tested negative (90.9%). The highest peak of positivity was reached the week from March 23rd to March 29th (39.5% of positivity).
Blood culture positivity rate and etiologies of bacteremia during COVID periodDuring the period of study, there were 282 cases of bacteremia belonging to 258 patients, accounting for a positivity rate of 10.7%. Among COVID-positive patients, 44 had bacteremia (positivity rate 12.5%), and among non-COVID patients 170 had bacteremia (positivity rate 10.2%) (p<0.001); 68 bacteremia cases occurred in untested SARS-CoV-2 RT-PCR (positivity rate 13.3%).
Among patients with positive blood cultures, COVID patients had a significantly higher proportion of nosocomial bacteremia (95.5%) than non-COVID-19 patients (30.5%) (p<0.001) being catheter-related bacteremia the main origin. Furthermore, while in most of bacteremia cases in COVID patients the requesting service was the ICU (70.5%), in the non-COVID patients it was the Emergency Department (45.3%). In fact, community-acquired bacteremia was the main origin in non-COVID patients (p<0.001). In relation to one month mortality rate, no significant difference was found (p=0.101).
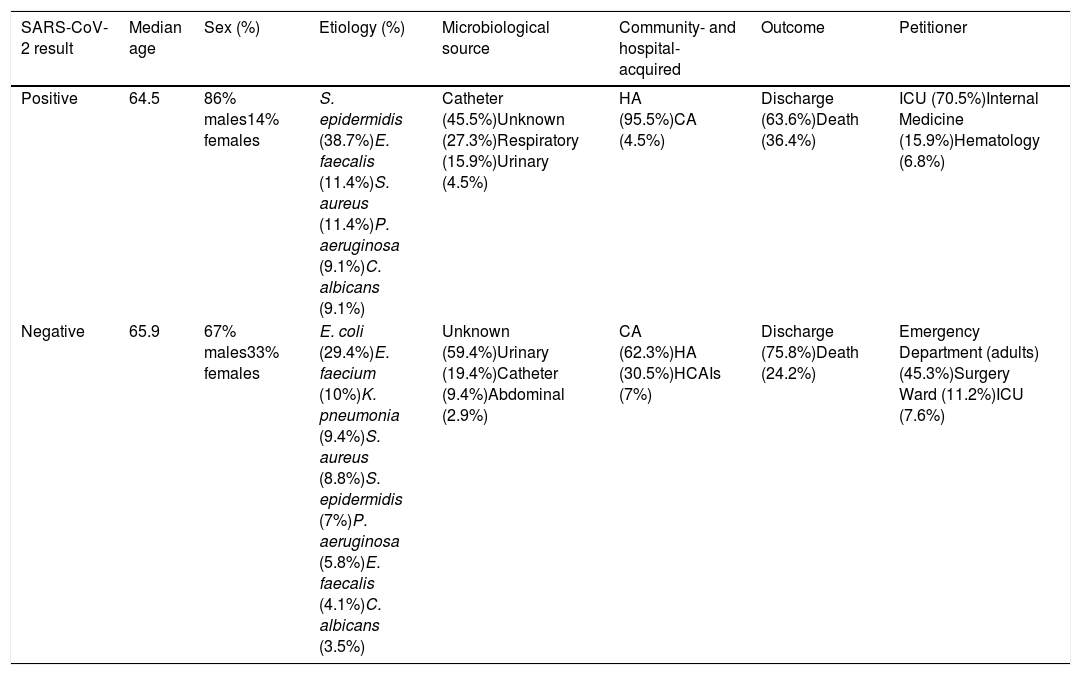
The most common etiology of bacteremia, source, outcome and requesting service are summarized in Table 1.
Characteristics of bacteremias in COVID-positive and COVID-negative patients.
| SARS-CoV-2 result | Median age | Sex (%) | Etiology (%) | Microbiological source | Community- and hospital-acquired | Outcome | Petitioner |
|---|---|---|---|---|---|---|---|
| Positive | 64.5 | 86% males14% females | S. epidermidis (38.7%)E. faecalis (11.4%)S. aureus (11.4%)P. aeruginosa (9.1%)C. albicans (9.1%) | Catheter (45.5%)Unknown (27.3%)Respiratory (15.9%)Urinary (4.5%) | HA (95.5%)CA (4.5%) | Discharge (63.6%)Death (36.4%) | ICU (70.5%)Internal Medicine (15.9%)Hematology (6.8%) |
| Negative | 65.9 | 67% males33% females | E. coli (29.4%)E. faecium (10%)K. pneumonia (9.4%)S. aureus (8.8%)S. epidermidis (7%)P. aeruginosa (5.8%)E. faecalis (4.1%)C. albicans (3.5%) | Unknown (59.4%)Urinary (19.4%)Catheter (9.4%)Abdominal (2.9%) | CA (62.3%)HA (30.5%)HCAIs (7%) | Discharge (75.8%)Death (24.2%) | Emergency Department (adults) (45.3%)Surgery Ward (11.2%)ICU (7.6%) |
CA, community-acquired; HA, hospital-acquired; HCAIs, Health care-associated infection.
There were 322 isolates considered contaminants belonging to 261 patients. The contamination rate was 12.3% in COVID-positive, 5.7% in COVID-negative patients, and 4.5% in untested patients (p<0.001).
The most common causes of contamination were coagulase-negative Staphylococcus species, among both COVID-19 patients (86.7%) and non COVID-19 patients (65.7%).
DiscussionDuring the study period, an important decrease in the number of blood cultures was observed in our laboratory. This phenomenon could be explained by the decrease in the number of patients who went to the Emergency Department, as well as the decrease in scheduled surgeries caused by the pandemic. The single exception was ICUs and Children's Emergency Department, which showed a marked increase when compared to previous years.
One of the measures that was carried out during the pandemic was to replace the face-to-face consultations by telephone consultations in primary care centres. It is possible that in patients with fever, medical care was focused on whether the patient had COVID, recommending isolation at the slightest suspicion and possibly forgetting other causes of fever, such as bacteremia. Besides, fear of contracting COVID-19 could also lead patients to stay longer at home. This would explain the decrease in the number of patients that went to the Emergency Department, the largest source of blood culture sets, and consequently the lesser number of blood withdrawals.
When comparing our results to previous literature, we found very few data. A research was performed in New York City4; however, a very different situation was described, with a dramatic increase in the use of blood cultures, which overwhelmed the capacity of their automated blood culture instruments, which was translated into the incubation period, having to be reduced from 5 days to 4 days. In our case, due to the decrease in the number of blood cultures received, it was not necessary to decrease the incubation time.
Regarding the etiology of bacteremia, a different trend was observed between COVID-positive and non-COVID patients. COVID-positive patients had bacteremia caused mainly by healthcare-associated organsims, such as coagulase-negative Staphylococcus species and Candida spp; by contrast, non-COVID patients had bacteremia caused more frequently by community-acquired pathogens. Again, this is different from the aforementioned New York City study4 and the UK study,5 where, among COVID-positive patients with true bacteremia, the distribution of clinically important organisms was similar to patients without COVID. The exception to this was Candida spp, which was notably isolated in both groups of patients. Although the results suggest a higher rate of candidemia than during previous years, this affirmation would require further study, as the short time of study accounts for a small sample relative to the low annual incidence.
It can also be concluded, along with the New York research,4 that the bacterial infection rate - bacteremia in our case- is low, but the pandemic may have led, as an undesired consequence, to a limited care in some patients in a process as relevant as sepsis.
A high proportion of blood culture contamination was identified, especially in COVID-positive patients. It could be explained by unfamiliarity of additional personal protective equipment worn by healthcare workers taking blood cultures.
It is worth mentioning, however, that the high number of blood cultures in the New York study4 (over 88,000 patient cultures) was also one of its major strengths. In comparison, our study is much smaller with only 5313 cultures, which allows for a worse generalizability. The multicentre analysis from a wide geographic catchment area was also mentioned as another strength, in contrast to ours, which consisted of a single hospital.
Sepsis is a time-dependent disease, and prognosis may improve if early diagnosis and appropriate treatment are achieved.6 All of this makes us rethink whether during the epidemic the anamnesis of the patients was correct, not focusing entirely on COVID-19 but instead paying attention to other diseases such as bacteremia.
Ethical approvalInstitutional ethical review board approval was not required.
Informed consentThis analysis does not contain patient data; therefore, informed consent was not required.
Conflict of interestThe authors declare that they have no conflict of interest.