We present two cases of lung involvement after travel to Peru.
Case 1: a 29-year-old female with a history of hypothyroidism and allergic rhinitis. The patient and her companion (case 2), both of Spanish nationality and residence, presented as a determinant a recent three-week stay in Peru, starting in the southern region and then in the Amazon area. She reported having stayed overnight in huts with adequate sanitary conditions, contact with amphibian and ophidian species and bathing in fresh water. She had no direct contact with birds. She had not taken traveller's advice or undergone any prophylaxis. Valid childhood vaccinations.
She consulted with a 40°C fever, which started 10 days after her return, associated with a productive cough and exertional dyspnoea. She was assessed initially at another centre, with antigenuria (Streptococcus pneumoniae, Legionella) and negative blood cultures, and chest X-ray with bibasilar interstitial pattern. Treatment was started with amoxicillin and azithromycin. After one week, she consulted at our centre for a persisting fever and was admitted to complete testing.
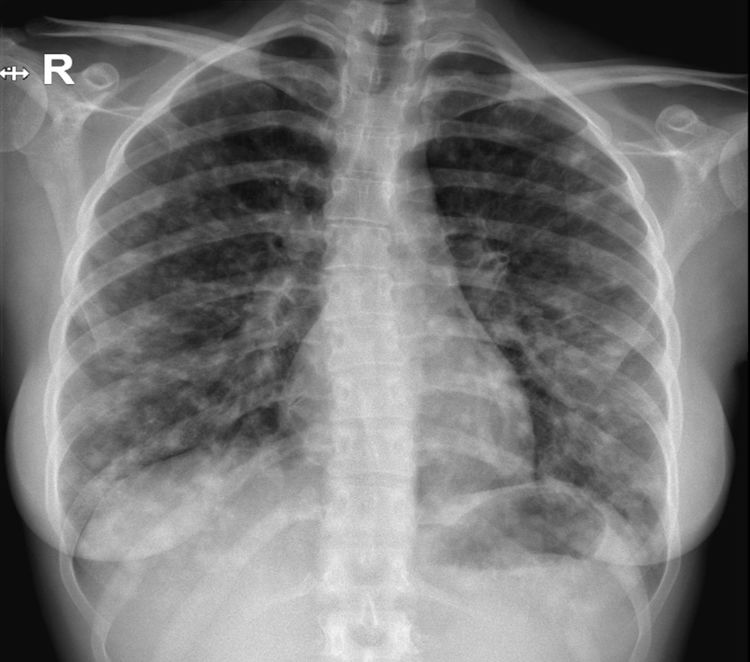
At admission, the presence of bibasilar crackles was of note. The rest of the examination was normal. The blood tests revealed: PCT 0.1 and CRP 80. Normal general blood chemistry. ABG: hypoxaemia without hypercapnia. Hb: 14.1; platelets 274,000; 8420 white blood cells (67.5% N; 22% lymphocytes; 8.9% monocytes; 0.8% eosinophils). The chest X-ray (Fig. 1) revealed poorly defined bilateral nodular infiltrates. Plasmodium antigen testing and the thick drop test were performed, with a negative result.
Treatment was started with ceftriaxone and levofloxacin, and extended microbiological testing, CT scan and fibrobronchoscopy were requested.
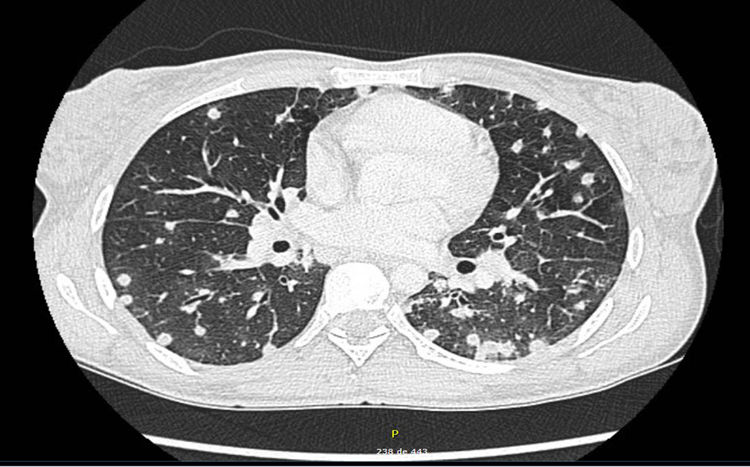
The CT scan (Fig. 2) showed multiple bilateral lung nodules; mediastinal and pathological bilateral hilar lymphadenopathies; hepatic hilar lymphadenopathies of a limited size, as well as small retroperitoneal, pelvic and inguinal lymphadenopathies. The sputum culture was negative for common bacteria, mycobacteria and fungi. The pharyngeal smear and QuantiFERON-TB Gold test were negative. Serological testing for hepatitis B and C, HIV, CMV, Epstein–Barr virus, varicella-zoster, IgM, Zika, chikungunya, dengue, hantavirus, Coxiella burnetii, Mycoplasma pneumoniae and Leptospira were negative. The video bronchoscopy did not reveal macroscopic findings. Bronchial aspirate and bronchoalveolar lavage were collected, with the Gram stain, KOH test, specific cultures for common bacteria, mycobacteria, Nocardia and fungi and molecular techniques for Pneumocystis and CMV being negative. Serology was ordered for endemic mycoses.
When the fever disappeared and the dyspnoea improved, she was discharged on treatment with levofloxacin.
Clinical courseAfter a few days, the serology determined a positive result for Paracoccidioides brasiliensis (P. brasiliensis) and a negative result for Histoplasma, Blastomyces and Coccidioides. Treatment was started with itraconazole 100mg/24h, following the Brazilian guidelines.1 The subsequent clinical course was favourable, completing six months of treatment with no incidents. The patient remained asymptomatic, with normalisation of the acute phase reactants and disappearance of the lung lesions.
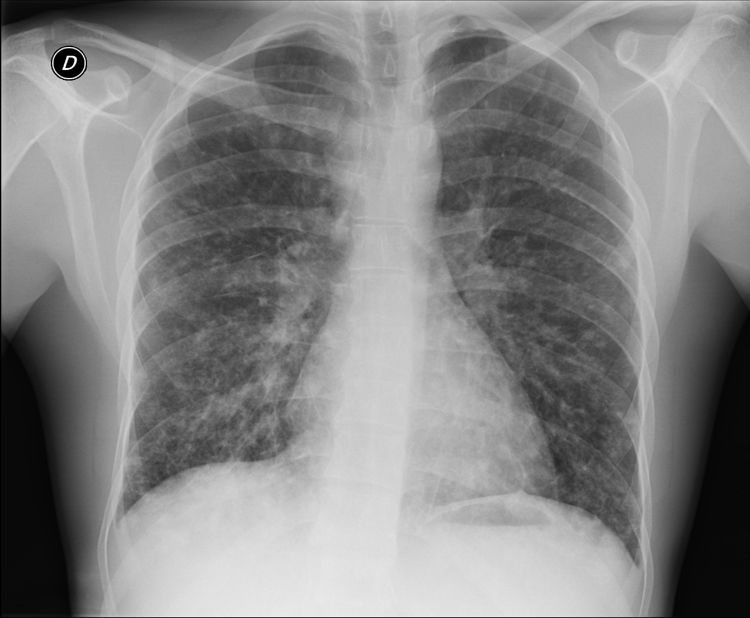
Case 2: male, 31-years-old. No relevant history. He was admitted at another centre due to fever, myalgia and asthenia in the same time frame as the patient in case 1. An X-ray was performed with a diffuse bilateral reticulonodular interstitial pattern (Fig. 3). Testing was completed with a video bronchoscopy (BAS and BAL), CT scan and microbiological testing similar to that of case 1, with no aetiological result. Serology was ordered for endemic mycoses. This was initially negative, but turned positive for P. brasiliensis after 10 days. He received treatment with itraconazole, with a satisfactory clinical course.
CommentsParacoccidioidomycosis is a fungal infection caused by the fungus P. brasiliensis which is considered endemic to the American continent, with cases reported from Mexico to Argentina. Brazil is the country with the greatest endemicity.2,3
The infection is caused by inhalation of spores when exposed to the rural environment. The majority (96–98%) of those infected never develop the disease. Among symptomatic individuals, the most common form (90%) is the chronic one, with periods of latency of years/decades, with predominance of lung and mucous membrane involvement. The acute/sub-acute form happens after incubation for 30–60 days,4 occurs predominantly in individuals under the age of 30 and the involvement of the reticuloendothelial system (hepatosplenomegaly and lymphadenopathies) and of the skin.5
The diagnostic techniques with the best performance are direct vision in samples prepared with KOH and serology by means of double immunodiffusion.6
On a state level, there are 34 cases reported to date, 21 of which are published. All of them are of chronic presentation in long-term travellers or immigrants.7,8
Our case presents various particularities: (a) it is the first case in short-term travellers of which we are aware at state level; (b) to date acute forms had not been reported in Spain; (c) significant lung involvement despite being an acute form, in which this involvement is rare (10%), and (d) absence of direct diagnosis by means of cultures or direct vision.
Finally, we would like to highlight that, although it is rare, there is a maintained incidence of paracoccidioidomycosis and other endemic mycoses, both in travellers and in immigrants,9 which makes it necessary to maintain a high level of suspicion in patients with a history of compatible geographic exposure.10
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Agirre E, Osorio A, Casas Fernández de Tejerina JM, Rodríguez-Arrondo F, Salicio Bermejo Y. Neumonía intersticial bilateral tras viaje reciente a Perú. Enferm Infecc Microbiol Clin. 2019;37:609–610.