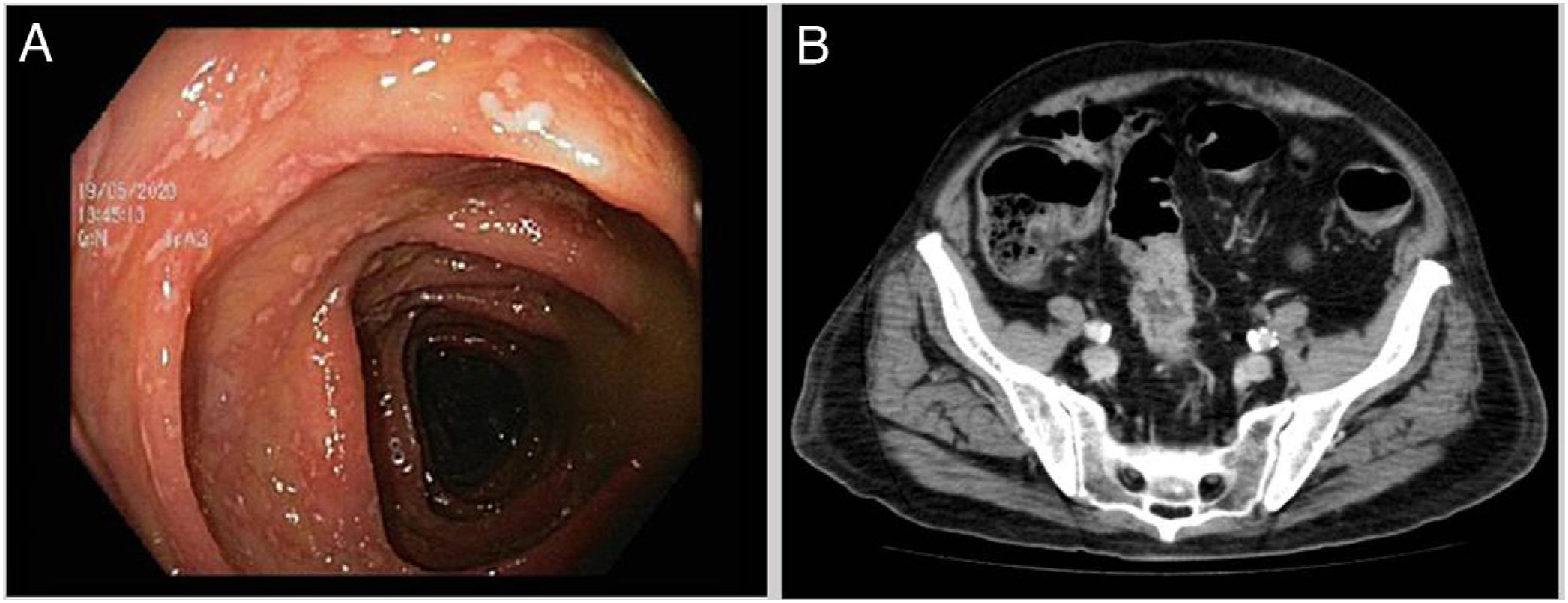
We report the case of a 65-year-old man with a history of hypertension, dyslipidaemia and ischaemic cardiomyopathy who visited the accident and emergency department due to diarrhoea for the past three weeks, with 10-12 liquid bowel movements per day with no pathological products or abdominal pain. This was associated with peripheral polyarthritis in the past two weeks, initially in the left knee and ankle and subsequently in the right carpus and first metacarpal bone; fever spikes at 38 °C; and 6 kg of weight loss. Prior to the onset of his signs and symptoms, he had suffered from two urinary tract infections secondary to Escherichia coli. These infections had been treated with trimethoprim/sulfamethoxazole for five days. The latter infection had occurred approximately a month earlier. Initial laboratory testing revealed elevated acute-phase reactants with a C-reactive protein level of 19 mg/dl. As inflammatory bowel disease was clinically suspected, the patient was given corticosteroid therapy (inappropriately, in the absence of an aetiological diagnosis), with initial but only temporary improvement. An outpatient colonoscopy showed areas of erythematous mucosa covered in whitish formations throughout the colon, indicative of infectious disease rather than inflammatory bowel disease (Fig. 1A). Colon biopsy was inconclusive, although it did point to an infectious origin. Given the patient's poor clinical course, with increased numbers of bowel movements and affected joints, and in the absence of an aetiological diagnosis, a decision was made to admit him to hospital.
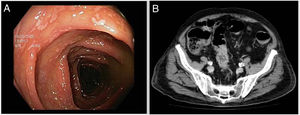
At the beginning of his hospital stay, laboratory testing showed elevated C-reactive protein (31 mg/dl), an erythrocyte sedimentation rate of 120 mm/h, 17,700 leukocytes/mm3 (75% neutrophils) and normocytic normochromic anaemia of 9.8 g/dl. Abdominal computed tomography was ordered and revealed concentric wall thickening 5 cm long in the sigmoid colon (Fig. 1B). A stool analysis testing for Clostridioides difficile found antigen and toxin positivity by means of enzyme immunoassay (glutamate dehydrogenase [GDH], C. Diff Quik Chek Complete®, Alere). Thus a diagnosis of colitis due to C. difficile was confirmed. The rheumatology department was consulted for joint assessment of articular disease. Rheumatology reported symmetric polyarthritis in both elbow, carpal, metacarpophalangeal, proximal interphalangeal, knee, ankle, tarsal and metatarsophalangeal joints. Arthrocentesis of the patient's left knee, in which clear synovial fluid was extracted, with laboratory testing revealing 12,112 leukocytes/mm3 and negative cultures, was consistent with arthritis with inflammatory characteristics. A rheumatoid factor test and serologies for human immunodeficiency virus (HIV), syphilis and hepatotropic viruses were negative, and stool culture and urethral discharge both showed no microbiological growth. With other causes having been ruled out, the patient was diagnosed with C. difficile-associated reactive arthritis secondary to colitis. After the patient started oral vancomycin 125 mg every six hours for 10 days, non-steroidal anti-inflammatory drugs and corticosteroids (both intra-articular and ultimately systemic, for lack of initial improvement), he followed a satisfactory course in terms of both diarrhoea and joint disease.
Reactive arthritis is commonly associated with genitourinary and gastrointestinal infections caused by Chlamydia, Salmonella, Shigella, Campylobacter or Yersinia. C. difficile is a less recognised cause of colitis, with 50 case reports since the first of them in 1976. It pathogenesis is probably due to an autoimmune response to bacterial antigens that gain access to the bloodstream through the intestinal mucosa and affect joints and other tissues in genetically predisposed patients.1 The lapse of time between diarrhoea and arthritis varies (from one to four weeks). It presents as acute migratory polyarthritis of medium and large joints, especially in the legs. The diagnosis is a diagnosis of exclusion, after diseases such as gout, rheumatoid arthritis and other infections that tend to precede reactive arthritis have been ruled out.2 The diagnostic criteria proposed by Putterman and Rubinow in 1993 consist of sterile inflammatory arthritis with preceding diarrhoea following prior antibiotic exposure, a positive C. difficile test in faeces and the absence of other causes of colitis and arthritis that might account for the process.3 Treatment is based on antibiotic therapy for C. difficile infection and analgesics, intra-articular or even systemic corticosteroids, and disease-modifying antirheumatic drugs. In general, the prognosis is good, with complete resolution of symptoms in four to six weeks, and no relapses of joint disease documented to date.4
C. difficile-associated reactive arthritis is thought to be potentially underdiagnosed. In conclusion, this case illustrates the importance of including it as a possible causal agent in the evaluation of inflammatory arthritis associated with diarrhoea.
Please cite this article as: de los Mozos-Ruano A, Casas-Deza D, Calvo-Galindo R, García-López S. Artritis reactiva asociada a Clostridioides difficile: un caso clínico inusual y revisión de la literatura. Enferm Infecc Microbiol Clin. 2022;40:338–339.