Hepatitis C treatment with direct-acting antiviral agents successfully cures over 95% of patients.1 Providing access to treatment for all patients with chronic hepatitis C virus (HCV) is a priority in all plans to eliminate hepatitis C. To this end, suitable strategies are required for the diagnosis of active HCV infection.
The diagnostic algorithm for hepatitis C starts with the detection of antibodies. However, antibody detection techniques do not distinguish an active infection from a resolved infection.2 The detection of HCV RNA indicates viral replication, which is why it is the most commonly used marker to diagnose and confirm active HCV infection. Patients with positive HCV RNA are candidates to be assessed for antiviral therapy. HCV core antigen forms part of the internal structure of HCV. As with HCV RNA, its detection indicates viral replication.3
During the period from 2015 to 2017, at the Hospital Universitario San Cecilio in Granada and the Complejo Hospitalario Universitario de Santiago, we performed an ambispective and observational pilot study to evaluate the impact of the joint implementation of reflex testing, accompanied by the implementation of alerts for the requesting physician, on the referral of patients to be assessed for treatment.
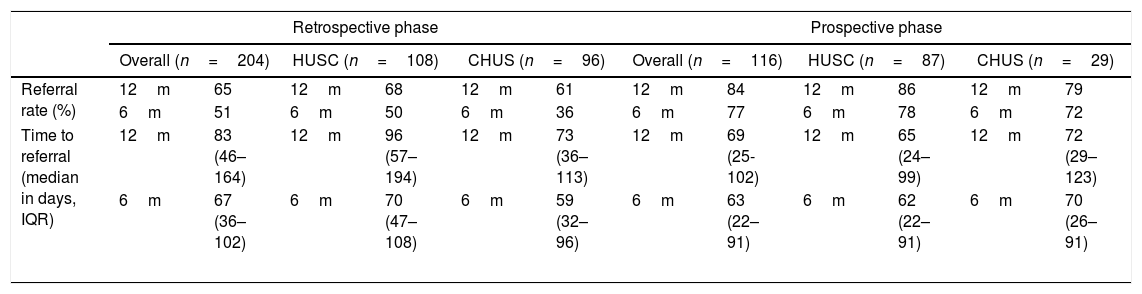
In the retrospective phase (January–December 2015), 204 new patients diagnosed with HCV were identified (108 from the Hospital Universitario San Cecilio, 96 from the Complejo Hospitalario Universitario de Santiago, 69.6% males, with a mean age of 54.0±13.28 years) by means of the traditional system (HCV serology and, in positive tests, confirmation with immunoblotting techniques and issuance of a report to the requesting physician). Following consultation of the electronic medical records and data in the laboratory information systems, and after one year of follow-up since diagnosis, we determined that 65% (133 patients) visited an infectious/gastrointestinal diseases specialist for a treatment assessment, after a median of 83 days (IQR: 46–164). Of these 133 patients, 68% were referred from Primary Care. The remaining 71 patients (35%) were not seen for a treatment assessment. A total of 65% of the patients had been diagnosed by Primary Care. Of all the patients who were assessed for treatment, 88% were viraemic.
The prospective phase was performed in the period from March to December 2016 and consisted in implementing reflex testing, by incorporating the detection of viraemia using core antigen testing (Architect HCV Core Ag Assay®, Abbott Diagnostics, Germany) on the same sample in which the positive serology result was obtained for all new diagnoses, so that patients with previous positive serological tests were excluded. In addition, a comment was included systematically in the reports, in which it was advised to refer patients with active infections to the specialist in order for them to be assessed for treatment. In this period, we analysed 116 new HCV diagnoses in Primary Care (87 from the Hospital San Cecilio, 29 from the Complejo Hospitalario Universitario de Santiago, 67% males, with a mean age of 56±14 years). There were no differences in terms of age and gender at the two centres included in the study, neither in the retrospective nor prospective phase, although a greater number of patients included from the Hospital Universitario San Cecilio came from Primary Care. After one year of follow-up, 84% of the patients were assessed to start treatment, after a median of 69 days (IQR: 25–102) from diagnosis to the consultation with the specialist. Only 18 patients (16%) were not seen by the specialist. Table 1 summarises the frequency and times to referral in both phases of the study, with the details of the referral at one year and at six months from diagnosis. These data reveal that reflex testing is an alternative which improves the traditional diagnosis, as it allows a greater number of losses in referral to be avoided.4–6 Furthermore, reflex testing avoids overloading specialist consultations with patients whose infections have already resolved spontaneously.7,8
Characteristics of patient referrals in the retrospective and prospective phases of the study.
| Retrospective phase | Prospective phase | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall (n=204) | HUSC (n=108) | CHUS (n=96) | Overall (n=116) | HUSC (n=87) | CHUS (n=29) | |||||||
| Referral rate (%) | 12m | 65 | 12m | 68 | 12m | 61 | 12m | 84 | 12m | 86 | 12m | 79 |
| 6m | 51 | 6m | 50 | 6m | 36 | 6m | 77 | 6m | 78 | 6m | 72 | |
| Time to referral (median in days, IQR) | 12m | 83 (46–164) | 12m | 96 (57–194) | 12m | 73 (36–113) | 12m | 69 (25-102) | 12m | 65 (24–99) | 12m | 72 (29–123) |
| 6m | 67 (36–102) | 6m | 70 (47–108) | 6m | 59 (32–96) | 6m | 63 (22–91) | 6m | 62 (22–91) | 6m | 70 (26–91) | |
CHUS: Complejo Hospitalario Universitario Santiago de Compostela; HC: hospital care; HUSC: Hospital Universitario San Cecilio; m: months; PC: primary care.
In conclusion, our study shows how the implementation of reflex testing has a real impact on the treatment cascade for hepatitis C, by allowing a greater number of patients to be assessed for treatment. We believe that these diagnostic strategies should be incorporated by Microbiology Departments, to help eliminate hepatitis C.
Please cite this article as: Casas P, Navarro D, Aguilera A, García F. Diagnóstico tradicional versus diagnóstico en un solo paso del virus de la hepatitis C. Estudio piloto en 2 centros asistenciales. Enferm Infecc Microbiol Clin. 2019;37:348–349.