The burden of disease from sexually transmitted infections (STI) undermines sexual and reproductive health and the health of newborn infants. The presence of some STI facilitates the transmission of others, such as HIV, and cause cellular changes that precede some types of cancer. For all these reasons STIs are a first order uncontrolled public health problem. In Spain, gonococcal infection has been on rising since the beginning of 2000, while syphilis has remained stable at high levels since 2011. Both infections are more common in males. Chlamydia trachomatis is the most common STI, and principally affects females between the ages of 20 and 40.
STI units are an essential instrument to tackle this problem. They deal with populations that are particularly vulnerable to these infections and are essential for their control by means of interventions that reduce their transmission efficiency and infectivity duration. They are also the principal source of epidemiological information about these infections.
La carga de enfermedad derivada de las infecciones de transmisión sexual (ITS) compromete la salud sexual, reproductiva y del recién nacido. La presencia de unas ITS facilita la transmisión de otras, como el VIH, y provoca cambios celulares que preceden algunos tipos de cáncer. Todo ello hace de las ITS un problema de salud pública de primer orden no controlado. En España, la infección gonocócica sigue creciendo desde el inicio de la década del 2000, mientras que la sífilis se mantiene estable en unos niveles altos desde el 2011. Ambas son más frecuentes en varones. Chlamydia trachomatis es la ITS más prevalente, afectando principalmente a mujeres de 20-24 años.
Las unidades de ITS son el instrumento fundamental para abordar este problema. Tratan con poblaciones especialmente vulnerables a estas infecciones y son esenciales para su control mediante intervenciones que disminuyen la eficiencia de su transmisión y la duración de la infectividad. Además, son la principal fuente del conocimiento epidemiológico de las mismas.
It is estimated that one million new gonococcus, Chlamydia trachomatis, Treponema pallidum and Trichomonas vaginalis infections arise each day and that 357 million new cases of infections caused by these four microorganisms are recorded every year in people aged 15–49.1 Around 417 million people are carriers of herpes simplex virus type 2 and 291 million women are carriers of the human papillomavirus.2
STIs do not just cause acute conditions like vaginitis, cervicitis, urethritis, proctitis and genital ulcers, but they may also give rise to chronic and serious complications such as pelvic inflammatory disease (PID), infertility, ectopic pregnancy, chronic pelvic pain, neonatal death, preterm birth, reactive arthritis and cancer, as well as an increased risk of transmission and acquisition of HIV.
The European Centre for Disease Prevention and Control (ECDC) has been coordinating the epidemiological surveillance of STIs in the European Union since 2009. In Spain, the epidemiological data for the general population pertaining to these infections is provided by the Sistema de Enfermedades de Declaración Obligatoria [Notifiable Diseases System] (EDO) and the Sistema de Información Microbiológica [Microbiological Information System] (SIM), that form part of the Red Nacional de Vigilancia Epidemiológica [National Epidemiological Surveillance Network] (RENAVE). In 2015, the number of notifiable STIs increased from three (syphilis, congenital syphilis and gonococcal infection) to five with the addition of C. trachomatis (serovars D–K) and lymphogranuloma venereum (LGV) (C. trachomatis, serovars L1, L2 and L3). The reporting of all five diseases is required by law, although this has not been fully implemented.3,4
GonorrhoeaIn 2016, the ECDC recorded 75,249 cases of gonococcal infection (incidence: 18.8/100,000), 46% of which occurred in men who have sex with men (MSM).5
In Spain, the incidence of gonococcal infection has been on the rise since 2001, increasing from a rate of 2.02/100,000 to 13.89/100,000 in 2016. 83.7% of the 6456 cases reported in Spain in 2016 were in men, with a male to female ratio of 5.1:1. The incidence in men was 23/100,000 versus 4.32/100,000 in women. By age, the highest incidences were recorded in the 20–24-years age group (89.2/100,000 in men and 21.5/100,000 in women), consistent with the rest of Europe.6
SyphilisIn 2016, 29,365 cases of syphilis were recorded in the European Union (incidence: 6.1/100,000). Incidence was eight times higher in men than women and 66% of cases involved MSM. Its incidence across Europe has been on the rise since 2010, primarily in MSM.7
In 2016, 3357 cases of syphilis were recorded (incidence: 7.22/100,000). In 2001, the incidence was 1.77/100,000, which steadily increased until 2011 before stabilising. 89.9% of the cases reported in 2016 were in men, with a male to female ratio of 9:1. As with gonococcal infection, incidence was significantly higher in men (13.32/100,000) than in women (1.43/100,000). The highest incidence was recorded in the 25–34-years age group, with rates of 35/100,000 in men and 4.6/100,000 in women.6
Congenital syphilisIn 2016, 37 cases of congenital syphilis were reported in the European Union, representing a rate of 1.1 cases per 100,000 live births.8 In Spain, four confirmed cases of early congenital syphilis were recorded (0.97 per 100,000 live births) and all were diagnosed in the first month of life.6
ChlamydiaIn 2016, 403,807 cases of C. trachomatis infection were reported to the ECDC, representing an overall rate of 184/100,000. Incidence was highest among young and heterosexual women (just 9% of cases were recorded in MSM).9 In Spain, 7162 cases were recorded and the overall incidence for the 15 autonomous communities with an established surveillance system for chlamydia infection was 17.85/100,000. The highest rates were recorded in Catalonia (46.4), Navarre (29.6), the Basque Country (27.1) and the Community of Madrid (18.4). As with the rest of Europe, incidence was higher in women (18.43/100,000) than in men (17.09/100,000) and in the 20–24-years age group (93.97/100,000).6
Lymphogranuloma venereum (LGV)In 2016, 22 European countries reported 2043 cases of LGV, 87% of which from the United Kingdom, France and the Netherlands. The number of cases rose by 15% compared to 2015. Almost all reported cases involved men who have sex with men and, of those whose HIV status was known, 70% were HIV+. As many countries still do not have LGV surveillance systems in place, the actual number of cases may exceed this figure.10 In Spain, 248 cases were reported in 2016 in five autonomous communities, the majority of which were in Catalonia (122) and Madrid (119). 94.4% were men, with a median age of 37. The incidence was 1.39/100,000 in men and 0.08/100,000 in women, respectively. By age group, the highest incidences were recorded among 25–34-year-olds (1.84/100,000) and 35–44-year-olds (1.77/100,000).6
Surveillance and various epidemiological studies suggest that LGV transmission primarily occurs among HIV+ MSM who engage in high-risk sexual practices.11,12
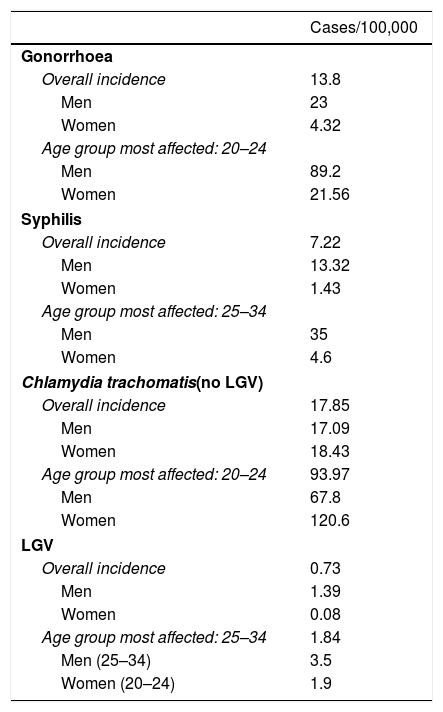
In conclusion, of all the STIs reported to the various surveillance systems, C. trachomatis infection is the most prevalent throughout Europe and Spain, with a higher incidence among women and among 20–24-year-olds. Incidence of gonorrhoea and syphilis is increasing in most of the European Union countries, primarily among men who have sex with men. The 2016 incidence of notifiable STIs in Spain is shown in Table 1.
Incidence of notifiable STIs in Spain in 2016.
| Cases/100,000 | |
|---|---|
| Gonorrhoea | |
| Overall incidence | 13.8 |
| Men | 23 |
| Women | 4.32 |
| Age group most affected: 20–24 | |
| Men | 89.2 |
| Women | 21.56 |
| Syphilis | |
| Overall incidence | 7.22 |
| Men | 13.32 |
| Women | 1.43 |
| Age group most affected: 25–34 | |
| Men | 35 |
| Women | 4.6 |
| Chlamydia trachomatis(no LGV) | |
| Overall incidence | 17.85 |
| Men | 17.09 |
| Women | 18.43 |
| Age group most affected: 20–24 | 93.97 |
| Men | 67.8 |
| Women | 120.6 |
| LGV | |
| Overall incidence | 0.73 |
| Men | 1.39 |
| Women | 0.08 |
| Age group most affected: 25–34 | 1.84 |
| Men (25–34) | 3.5 |
| Women (20–24) | 1.9 |
Source: HIV surveillance and risk behaviours.6
Vulnerability to STIs is determined by socio-economic factors (poverty, gender inequality), cultural factors (age of first sexual encounter, feminine hygiene washes, “dry sex”, etc.), biology (gender, age) and sexual behaviour (multiple sexual partners, type of sexual practice, use of drugs or alcohol, etc.). It is the responsibility of each country to identify the specific populations most at risk from these infections and to intensify prevention and care strategies. The expression “specific populations” includes those people more likely to have a high number of sexual partners, such as sex workers and their clients. Other possible high-risk populations include MSM, transgender people and people who already have an STI or HIV. Other particularly vulnerable groups are young people and adolescents, drug users, the homeless, prisoners and immigrants.2
In order to plan effective strategies, information is required on three populations: the “nuclear” or “core” population, consisting of the most vulnerable people where transmission is at its highest due to high-risk behaviour; the “bridge” population, comprising the sexual partners of the nuclear population; and the general population.
STI clinics treat populations that are highly vulnerable to STIs. In Spanish STI clinics, sex workers, men who have sex with men, transsexuals and immigrants are over-represented compared to the general Spanish population.13 In addition to this “nuclear” or “core” population, they also treat their contacts (the “bridge” population), which is why these clinics play a fundamental role in establishing not only the incidence and prevalence of various STIs in both populations, but also pertinent information about their characteristics and sexual practices. One example of the contribution of STI clinics in this field are the epidemiological studies conducted by HIV and STI prospective prevalence study groups, which are made up of specialist HIV and STI diagnosis and treatment centres located throughout Spain.13–17 STI clinics also play a crucial role as “lookouts” in the detection of unexpectedly high caseloads (epidemic outbreaks)18–20 or the detection of emerging diseases, as was the case with LGV.21,22
STI clinics in the prevention and control of STI transmissionThe spread of STIs is measured by the basic reproduction number or basic reproductive ratio of an infection (Ro), which is defined as the average number of new infections caused by an infected individual over a set period of time.
Ro=β×c×D
β=likelihood of transmission by sexual contact
C=average number of partners per unit of time
D=duration of infectivity
The basic reproduction number (Ro) must fall in order to control STIs, and STI clinics play an irreplaceable role in reducing the likelihood of transmission and the duration of infectivity.
Reducing the likelihood of transmission by sexual contact (β)There are a variety of treatments or strategies to reduce STI transmission that are or may be offered by STI clinics.
- 1.
Vaccines: Vaccines are currently available for hepatitis A, hepatitis B and HPV.STI clinics should offer free hepatitis B vaccinations to all unvaccinated patients and hepatitis A vaccinations to MSM, parenteral drug users and anyone susceptible to acquiring this infection due to their sexual practices (in Catalonia, Ceuta and Melilla, the hepatitis A vaccine is already included in the vaccination schedule). In Spain, the HPV vaccine was introduced in 2007–2008 but is only indicated and funded for 12-year-old girls. In 2014, vaccination coverage from one autonomous community to another ranged from 53.8% to 95.9%.23 STI clinics should inform unvaccinated women, MSM and transgender people up to the age of 26 of the HPV vaccine.24–26 For HIV+ patients aged 26 or younger, the vaccination is already recommended by the Spanish HPV infection control and monitoring guidelines.27
- 2.
Promotion of the consistent and correct use of condoms.
- 3.
Non-occupational post-exposure prophylaxis (nPEP) for HIV, which should also include screening for all other STIs.
- 4.
Pre-exposure prophylaxis for HIV (PrEP). Because STI clinics or units have enormous experience dealing with high-risk sexual behaviour and managing populations that are particularly vulnerable to HIV infection, they are the ideal setting in which to offer PrEP, not least because its implementation also requires regular kidney function monitoring and STI check-ups. PrEP is associated with lower condom use and a significant increase in rectal STIs.28 PrEP should form part of a “package”, which includes:
- -
Safe sex counselling.
- -
Provision of condoms.
- -
nPEP counselling.
- -
Specialist care, if required, to modify high-risk behaviour or drug (chemsex) or alcohol problems.
- -
Periodic screening for HIV and other STIs, including hepatitis C.
- -
Hepatitis A, hepatitis B and HPV vaccination.
- -
- 5.
Antiretroviral therapy in HIV patients.
- 6.
Suppressive therapy for recurrent genital herpes.
Access to an effective treatment is the most important factor to reduce the duration of infectivity. The early detection and treatment of infected individuals prevents transmission to other people, providing primary prevention of infection to the general population while offering secondary prevention against possible complications in individuals. The treatment is prevention, and a lack of appropriate sexual health services increases the duration of infectivity.
A poignant example around the world of the repercussions of the delayed diagnosis and treatment of an STI is the late diagnosis of HIV, with its implications on the person infected (late treatment increases patient morbidity and mortality) and on public health (the risk of transmitting the virus increases the longer a person is unknowingly infected and the longer the infection goes untreated). In Spain, STI clinics have proven to be effective in reducing the late diagnosis of HIV infection.29 In 2012, 48% of new HIV diagnoses reported to the SINVIH [information system on new HIV diagnoses] had CD4 levels below 350, and 28% had levels below 200.30 In comparison, of all the cases diagnosed in STI clinics between 2003 and 2013, 26.4% had CD4 levels below 350 and 8.8% below 200.31
A rapid diagnosis also facilitates the implementation of a contact investigation to offer diagnostic and treatment services as promptly as possible to other people at high risk of having an STI. There are three partner notification methods: “information from the patient”, when the index case reports the infection; “information from the healthcare provider”, when a healthcare professional reports the infection; and “contractual information”, when the patient reports the infection, but if he or she fails to do so within a given time, the healthcare professional undertakes the responsibility. There is no definitive evidence as to the most effective method for each STI.32 In Spain, recommendations and official guidelines on how to conduct contact investigations are extremely limited and “information from the patient” tends to be used. A study conducted in Barcelona on partner notification in patients with HIV, which combined “information from the patient” and “information from the healthcare provider” strategies, found a high level of user acceptance and effectiveness in detecting new HIV infection diagnoses.33
As well as being responsible for the diagnosis and treatment of symptomatic patients, STI clinics also actively search for cases by screening high-risk populations: contacts, sex workers, MSM and anyone who requests to be screened.
Average number of partners by unit of time or rate of partner change (c)The rate of sexual partner change varies widely within a population. Most studies suggest that there is significant heterogeneity, with a large group of people who report having had few sexual partners and a small group that reports having had a large number of partners. Strategies aimed at this nuclear or “core” group of highly sexually active individuals to promote condom use or to reduce the number of sexual partners should have a significant impact on the rate of STI transmission.
In 2012, the Clinical Effectiveness Group of the British Association for Sexual Health and HIV (BASHH) and the British HIV Association (BHIVA) reviewed the evidence concerning the effectiveness of safe sex counselling, in order to draft guidelines for UK genitourinary medicine specialists on how to offer such counselling in STI consultations and HIV check-ups. The review concluded that although behavioural interventions may effectively reduce the number of sexual partners, there is no direct evidence to support the effectiveness of strategies to reduce the number of partners implemented in the clinical setting. Even so, it concludes that consultations should include a discussion about reducing the number of partners or the number of unprotected sexual encounters, and particularly the risks associated with concurrent partners (two or more partners at the same time). Safe sex counselling should form part of all sexual health consultations, adapted to the individual based on their risk level, and it should also include information on the risks associated with various sexual practices (oral, genital, rectal, “fisting”, sex toys, etc.), as well as a recommendation to use a condom and information on its proven efficacy, limitations and correct use.34,35
ResearchResearch is an essential part of any quality clinical department and the questions that we are trying to answer in STI clinics are numerous, starting with the evaluation of our results. The establishment of national research priorities, implemented by multicentre studies conducted as part of an STI research network, is vital.
TrainingSTI clinics should provide resident physicians and nurses with the necessary training to ensure the greatest possible competency in the field of infectious diseases. Regular training should also be offered to primary care professionals, establishing fluent dialogue with them that facilitates patient and contact access to STI consultations.
ConclusionsDespite the fact that the primary role of STI clinics or units is the appropriate management of STIs, the range of services they offer varies considerably, from centres that only offer diagnosis and treatment to symptomatic patients, to clinics that offer HIV patient follow-up, nPEP, screening of high-risk populations, contact investigations, research, etc.
Effectively controlling STIs requires quick action, which is why it is essential to equip STI clinics and units with the necessary resources to ensure rapid and easy access to quality care. The European recommendations proposed by the International Union Against Sexually Transmitted Infections (IUSTI) on the organisation of STI clinics lists the staff that are essential for the effective operation of the clinic: administrative staff, qualified and auxiliary nurses, a medical team that may include several complementary specialties (infectious diseases, dermatology, gynaecology, urology, family medicine, etc.), laboratory staff and staff trained in partner notification. The support of research staff, educators and clinical psychologists is also recommended.36
A change of clinical focus from an individual approach to population-based strategies is vital if we really want to manage STIs. This would require bolstering integration between STI units and other departments (primary care, reproductive health, drug addiction centres, mental health, health education, school health, etc.) to improve both its impact as well as its effectiveness, establishing links with community organisations and facilitating the participation of the most vulnerable. One example is the Umbrella model in the United Kingdom, which, in 2015, redesigned the traditional sexual health services on offer in Birmingham and Solihull from fragmented, treatment-based services offered at specialist medical centres to a community-based prevention model with a focus on the education, empowerment and self-care of those most affected.37
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: López de Munain J. Epidemiología y control actual de las infecciones de transmisión sexual. Papel de las unidades de ITS. Enferm Infecc Microbiol Clin. 2019;37:45–49.
Section accredited by the Catalan Council for the Continuing Education of Health Professions. Consult questions for each article at: http://www.elsevier.es/es-revista-enfermedades-infecciosas-microbiologia-clinica-28-formacion.