This article aims to review the main information taken into account for the update of the GESIDA PLWH quality indicators.
Finally 54 indicators covering a major part of the clinical activity in PLWH were defined.
They evaluate the detection and diagnosis of PLWH, their follow-up and prevention, initiation and adaptation of ART, women's specific aspects, comorbidities, hospitalization, and AIDS-related mortality.
Este artículo tiene como objetivo revisar la principal información que se tuvo en cuenta para la actualización de los indicadores de calidad de PVV de GESIDA.
Finalmente, se definieron 54 indicadores que cubren la mayor parte de la actividad clínica en PVV. Los indicadores evalúan la detección y el diagnóstico de los PVV, su seguimiento y prevención, la iniciación y adherencia al TAR, aspectos específicos de la mujer, comorbilidades, hospitalización y mortalidad relacionada con el sida.
Consensus clinical guidelines for the diagnosis, care, follow-up, and antiretroviral treatment of patients with human immunodeficiency virus (HIV) infection provide recommendations for good clinical practice. Like other scientific associations, the Spanish AIDS Study Group (GESIDA) has been developing and updating consensus documents covering various and complex areas of care of people living with HIV (PLWH)1 In addition, goals related to diagnostic capacity and continued care have also been set, providing national AIDS programmes and UNAIDS with indicators that serve to monitor the HIV pandemic both at local and worldwide levels.2 Such indicators are necessary not only for countries and health administrations but also for care providers. Antiretroviral therapy (ART), prophylaxis for opportunistic infections, treatment of comorbidities, vaccinations, and promotion of healthy lifestyles have enabled people with a well-controlled HIV infection to have a life expectancy similar to the general population.3 However, early diagnosis, early ART initiation, and good adherence to treatments and health programmes require coordinated efforts of all healthcare and social agents involved in these patients’ care.
Although many articles on healthcare quality have been published, they are very heterogeneous, have generally been conducted in the United States or sub-Saharan Africa, and use different indicators.4 Some authors like Catumbela have suggested core indicators based on literature reviews.5 In 2015, Johnston et al. identified 558 potential indicators in a detailed review of the literature, but only 43 recurred in more than 3 studies and the most common ones were: continuous patient care, prophylaxis against Pneumocystis jiroveci, CD4 cell count, syphilis serology, and request for HIV viral load tests.6
Scientific societies such as the US Department of Health and Human Services (DHHS) or organizations such as the US Veteran's Administration, the New York State Department of Health AIDS Institute [NYSAI], and Kaiser Permanente7,8 have established quality of care indicators for PLWH. In 1992, the NYSAI developed the first quality of care programme for PLWH, which has been used in New York's hospitals, health facilities, drug treatment programmes, and community-based organizations. In 2010, in one of the most coordinated efforts to develop HIV care quality measures, the National Committee for Quality Assurance (NCQA) together with the American Medical Association (AMA), the Infectious Diseases Society of America (IDSA), and the HIV Medicine Association (HIVMA) developed 17 indicators addressing processes of care, including patient retention in care, appropriate health screening, prophylaxis, immunizations, and prescription of ART, which were later endorsed by the National Quality Forum.9 The British HIV Association (BHIVA) standards of care for PLWH were published for the first time in 2007 and subsequently updated twice. The 2018 BHIVA standards were written for service providers responsible for delivering healthcare and also for people receiving HIV care, and include measurable and auditable outcomes.10
GESIDA 2010 quality of care indicators: methodology, feasibility, and implementationIn 2010, a group of healthcare professionals was invited by the SEIMC-GESIDA Foundation to take part in a project to develop quality of care indicators for PLWH. The purpose of the project was to create a monitoring system measuring the most relevant aspects of these patients’ care by means of a number of quality indicators. The methodology used has been described in a study already published elsewhere.11 A total of 66 indicators were selected, of which 22 were considered relevant for the clinical management of PLWH and deemed by the SEIMC-GESIDA Foundation as applicable in all HIV Units.
GESIDA's indicators promoted the subsequent development of follow-up indicators for paediatric patients and hospital pharmacy care. Several GESIDA indicators were subsequently validated, their feasibility established, and adherence measured in multicentre studies.12 In line with other studies, it was found that certain relevant indicators could not be assessed in some centres and that information systems and activity data collection needed improvement.12 Electronic medical records and databases available in many units could generate these indicators automatically. In 2013, a section on quality of care indicators for patients with HIV infection was added to GESIDA's website. Hospitals could follow the link http://www.fundacionseimcgesida.org/indicadoresdecalidad/index.asp to conduct a self-assessment of the 22 relevant indicators included and compare themselves with similar-size hospitals.
Although quality indicators are developed to identify problems or care processes that may be improved, a number of studies that have used GESIDA's indicators or other indicators have shown that some are also associated with improved life-expectancy, better virological control, reductions in admissions and healthcare resource use, or improved patient-reported satisfaction with the quality of care.13,14
Revision of quality indicatorsAs stated in our previous paper, just as healthcare practice and scientific evidence change, so too do quality indicators which should be reviewed and adapted periodically as no one version of indicators can be definitive.
Thus, in 2019, at the initiative of GESIDA's management boards, a new working group was formed—advised by the University Institute-UAB Avedis Donabedian—to revise the 2010 version of quality indicators. The new document was drafted based on the review, update, and development of new indicators undertaken by different working groups and subsequently adopted by consensus. The actual usefulness of the indicators in measuring and establishing improvements in prevention, early detection, treatment, and management of associated comorbidities was taken into account during the revision. As a result, we have developed standards of care for PLWH from acquisition, across the life course, to end of life. In recent years, as we have learned that an undetectable viral load means that the virus is untransmittable and that it is particularly important to start ART as early as possible to prevent infection progression, new indicators such as time to ART initiation have been included. The measurement of variables associated with ART adherence such as socio-economic status and active substance use has also been added. Finally, comorbidity variables, such as frailty in adults over 60 years old, polypharmacy, obesity, metabolic syndrome or fatty steatosis, and patient-perceived quality of care have been included. The feasibility of their measurement was also considered and therefore indicators assessable in specific databases, thus enabling their regular monitoring, were promoted.
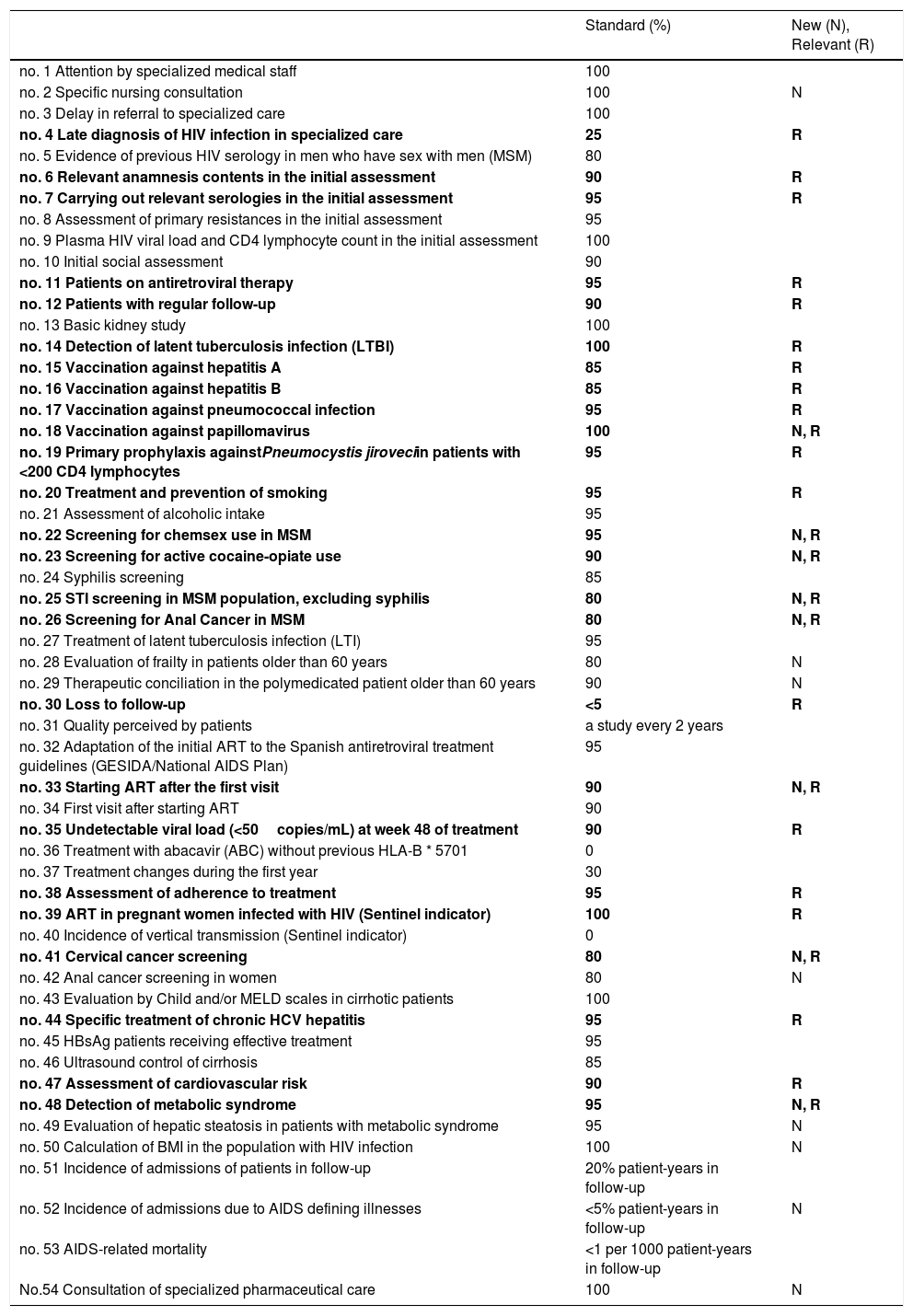
During the revision process, 54 indicators covering a major part of the clinical activity in PLWH were defined, of which 25 were considered relevant by the working group based on clinical relevance, health consequences, and quality of evidence (Table 1). In total, 28 indicators were removed and 16 were added. Thus, the final version includes 3 indicators measuring structure, 42 addressing processes of care, and 9 assessing outcomes. They evaluate the detection and diagnosis of PLWH, their follow-up and prevention, initiation and adaptation of ART, women's specific aspects, comorbidities, hospitalization, and AIDS-related mortality.
Quality indicators relevant for care of persons living with HIV.
| Standard (%) | New (N), Relevant (R) | |
|---|---|---|
| no. 1 Attention by specialized medical staff | 100 | |
| no. 2 Specific nursing consultation | 100 | N |
| no. 3 Delay in referral to specialized care | 100 | |
| no. 4 Late diagnosis of HIV infection in specialized care | 25 | R |
| no. 5 Evidence of previous HIV serology in men who have sex with men (MSM) | 80 | |
| no. 6 Relevant anamnesis contents in the initial assessment | 90 | R |
| no. 7 Carrying out relevant serologies in the initial assessment | 95 | R |
| no. 8 Assessment of primary resistances in the initial assessment | 95 | |
| no. 9 Plasma HIV viral load and CD4 lymphocyte count in the initial assessment | 100 | |
| no. 10 Initial social assessment | 90 | |
| no. 11 Patients on antiretroviral therapy | 95 | R |
| no. 12 Patients with regular follow-up | 90 | R |
| no. 13 Basic kidney study | 100 | |
| no. 14 Detection of latent tuberculosis infection (LTBI) | 100 | R |
| no. 15 Vaccination against hepatitis A | 85 | R |
| no. 16 Vaccination against hepatitis B | 85 | R |
| no. 17 Vaccination against pneumococcal infection | 95 | R |
| no. 18 Vaccination against papillomavirus | 100 | N, R |
| no. 19 Primary prophylaxis againstPneumocystis jiroveciin patients with <200 CD4 lymphocytes | 95 | R |
| no. 20 Treatment and prevention of smoking | 95 | R |
| no. 21 Assessment of alcoholic intake | 95 | |
| no. 22 Screening for chemsex use in MSM | 95 | N, R |
| no. 23 Screening for active cocaine-opiate use | 90 | N, R |
| no. 24 Syphilis screening | 85 | |
| no. 25 STI screening in MSM population, excluding syphilis | 80 | N, R |
| no. 26 Screening for Anal Cancer in MSM | 80 | N, R |
| no. 27 Treatment of latent tuberculosis infection (LTI) | 95 | |
| no. 28 Evaluation of frailty in patients older than 60 years | 80 | N |
| no. 29 Therapeutic conciliation in the polymedicated patient older than 60 years | 90 | N |
| no. 30 Loss to follow-up | <5 | R |
| no. 31 Quality perceived by patients | a study every 2 years | |
| no. 32 Adaptation of the initial ART to the Spanish antiretroviral treatment guidelines (GESIDA/National AIDS Plan) | 95 | |
| no. 33 Starting ART after the first visit | 90 | N, R |
| no. 34 First visit after starting ART | 90 | |
| no. 35 Undetectable viral load (<50copies/mL) at week 48 of treatment | 90 | R |
| no. 36 Treatment with abacavir (ABC) without previous HLA-B * 5701 | 0 | |
| no. 37 Treatment changes during the first year | 30 | |
| no. 38 Assessment of adherence to treatment | 95 | R |
| no. 39 ART in pregnant women infected with HIV (Sentinel indicator) | 100 | R |
| no. 40 Incidence of vertical transmission (Sentinel indicator) | 0 | |
| no. 41 Cervical cancer screening | 80 | N, R |
| no. 42 Anal cancer screening in women | 80 | N |
| no. 43 Evaluation by Child and/or MELD scales in cirrhotic patients | 100 | |
| no. 44 Specific treatment of chronic HCV hepatitis | 95 | R |
| no. 45 HBsAg patients receiving effective treatment | 95 | |
| no. 46 Ultrasound control of cirrhosis | 85 | |
| no. 47 Assessment of cardiovascular risk | 90 | R |
| no. 48 Detection of metabolic syndrome | 95 | N, R |
| no. 49 Evaluation of hepatic steatosis in patients with metabolic syndrome | 95 | N |
| no. 50 Calculation of BMI in the population with HIV infection | 100 | N |
| no. 51 Incidence of admissions of patients in follow-up | 20% patient-years in follow-up | |
| no. 52 Incidence of admissions due to AIDS defining illnesses | <5% patient-years in follow-up | N |
| no. 53 AIDS-related mortality | <1 per 1000 patient-years in follow-up | |
| No.54 Consultation of specialized pharmaceutical care | 100 | N |
In bold type relevant indicators.
The complete document with the review of the GESIDA quality of care indicators in PLWH can be visited at https://gesida-seimc.org/wp-content/uploads/2021/04/indice_calidad_Guia_GeSIDA.pdf.
We hope these indicators will be useful in healthcare practice and that their implementation will help improve the collection of data on PLWH care, monitoring, and follow-up.
Conflict of interestThe authors declare not to have any interest conflicts.
For this publication, no specific aid has been received from agencies of the public sector, commercial sector or non-profit entities.