The case of a 38-year-old male with a history of mild bronchial asthma and non-gonococcal urethritis is reported. The patient attended due to a 10-day history of symptoms, consisting of erythematous papules and multiple ulcerative-necrotic lesions on his face (Fig. 1), torso (Fig. 2) and limbs. He had poor general condition, odynophagia, cervical lymphadenopathies and a fever of up to 40°C. The fever and general involvement were self-limited in 48h, after empirical antibiotic therapy was started with amoxicillin-clavulanic acid, with the number of ulcerated lesions persisting and increasing.
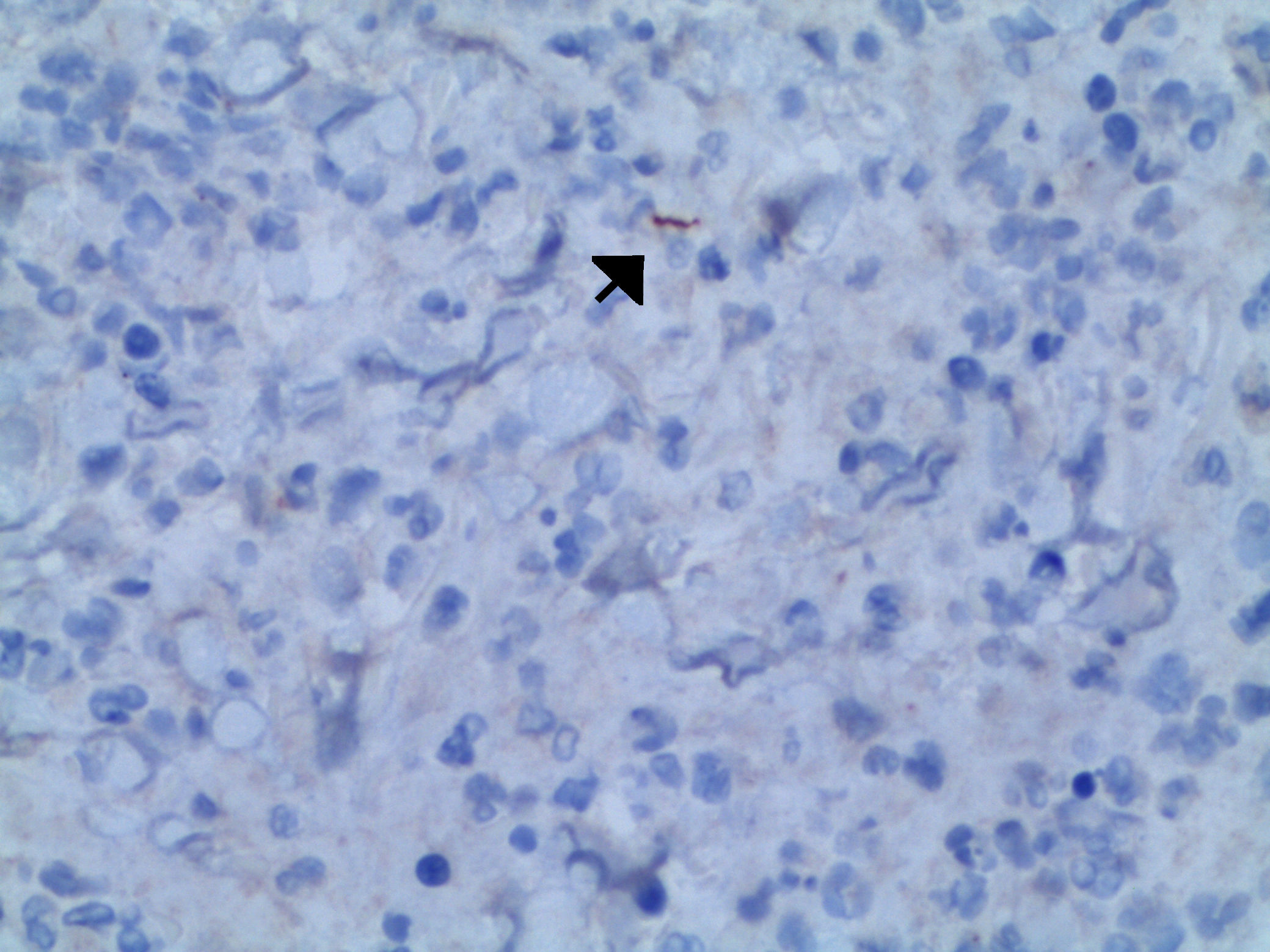
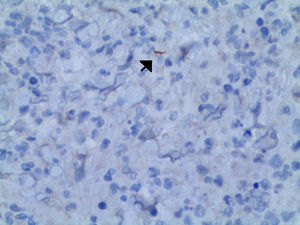
The biochemistry profiles, differential blood count and red blood cell count showed ranges within normal limits. A skin biopsy was performed using haematoxylin and eosin staining, which showed an inflammatory infiltrate with abundant polymorphonuclear leukocytes and plasma cells. Anti-treponemal antibodies were detected using immunohistochemistry (Fig. 3). The Gram stain of the sample was negative, and Staphylococcus epidermidis was isolated in the culture. The treponemal and non-treponemal tests were positive, with an RPR titre of 1/8. The remaining serology tests requested (human immunodeficiency virus, hepatitis B and C viruses, cytomegalovirus, Epstein–Barr virus) were normal or negative.
Clinical courseWith all the findings reported, the patient was diagnosed with malignant syphilis and treatment was established with benzathine benzylpenicillin 2,400,000IU via the intramuscular route in a single dose. The result of the positive culture for S. epidermidis was interpreted as a colonisation. The response to treatment was favourable, with resolution of the skin lesions in three weeks, and the reaginic tests became negative. Infection associated with HIV was ruled out in the initial study. However, the patient was retrospectively lost to medical follow-up. We interpreted the detected RPR titres, atypically low in this form of presentation in an immunocompetent patient, as a prozone phenomenon due to lack of dilution. We believe that the hypothesis that he is an HIV-infected patient in the window period is less likely.
CommentsMalignant syphilis is a rare condition and is generally considered a variant of secondary syphilis.1 It is characterised by generalised papulonodular lesions which typically become ulcers. It is generally accompanied by systemic symptoms, consisting of poor general condition, fever, headache, myalgia and arthralgia.
Most of the cases reported in the literature are associated with patients with HIV.2–5 Its presentation is less common in immunocompetent individuals.6 It is estimated that its presentation is 60 times more common than in patients not infected with HIV.2 The aetiopathogenesis of malignant syphilis is unknown. It is suggested that its presentation is related to the presence of virulent strains, combined with immunosuppression status which determines an inappropriate immune response.3
Malignant syphilis has a wide differential diagnosis, including pyoderma gangrenosum, skin lymphoproliferative processes, varicella-zoster virus infection, pityriasis lichenoides et varioliformis acuta, vasculitis or bacterial, fungal or mycobacterial infections.2,4
Diagnosis was based mainly on clinical findings and serological tests. Immunohistochemical staining using monoclonal antibodies against Treponema pallidum is a useful diagnostic tool which has high sensitivity and specificity,7 and which facilitated the diagnosis of the case report that we present. There are no differences to the therapeutic management of this form of syphilis compared to other clinical forms of secondary syphilis, with good response to standard treatment regimens.1,2,7
We presented a case of malignant syphilis in an immunocompetent male, a rare form of luetic secondary syphilis typical of HIV-infected patients. Based on our case, we would like to highlight the role of immunohistochemistry to support the diagnosis of this entity, along with clinical and serological findings, which can sometimes suffer a diagnostic delay due to their unusual presentation.
Please cite this article as: Cabrera-Fuentes R, Ortiz-Prieto A, Zulueta-Dorado T, Conejo-Mir J. Fiebre y lesiones ulceronecróticas en un varón de 38 años. Enferm Infecc Microbiol Clin. 2018;36:386–387.