A 13-year-old male, previously healthy, came to the emergency room due to a global headache of moderate intensity and present for 15 days, fever and vomiting for 3 days prior to admission, presented sudden and progressive onset oedema in the left fronto-orbital region (Fig. 1).
On physical examination, we found increased volume in the left frontal-orbital region of the skull, painful on superficial palpation, no subsidence or exostosis felt, no crackling, presented halitosis. Rest of physical examination normal, neurologically intact.
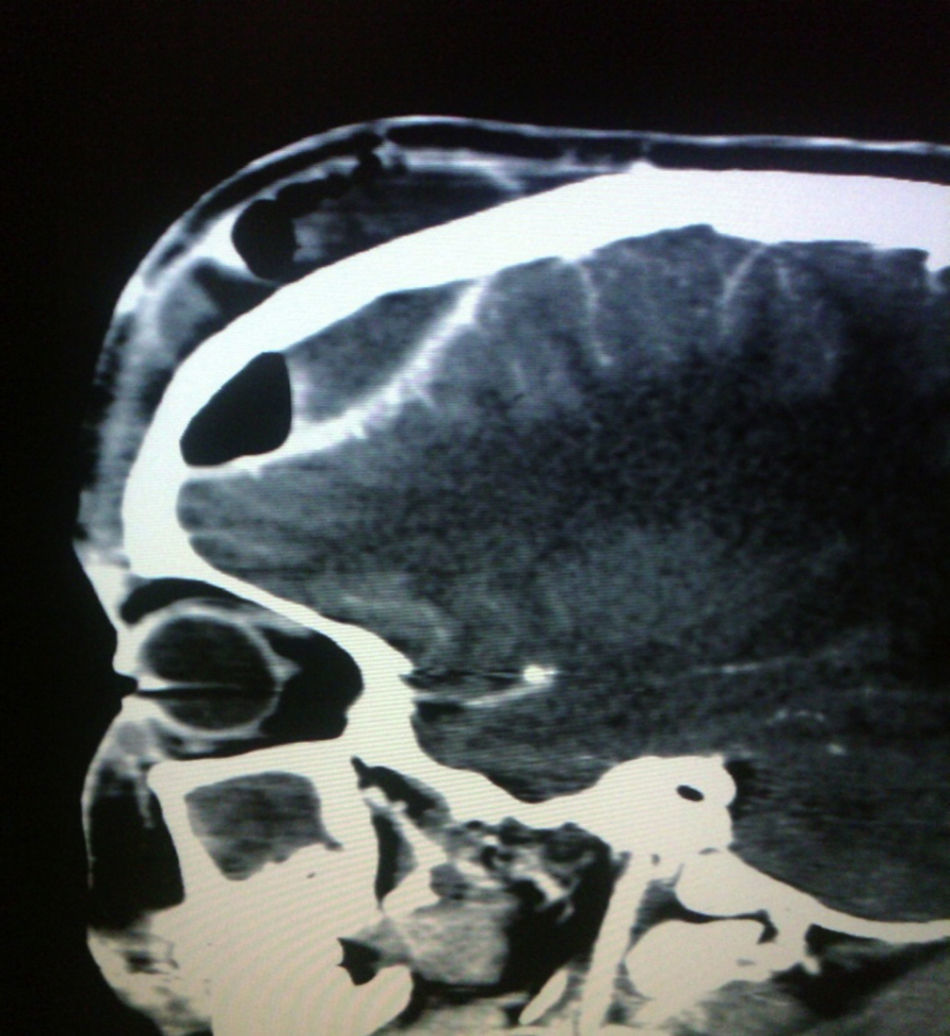
The CBC reported: leukocytes 17,900 mm3 (range: 4500–14,000), N 77%, B 7%, L 13% and M 3%. Cranial computerised tomography (CT) scan revealed frontal epidural empyema, left pansinusitis and frontal soft tissue involvement (Figs. 2 and 3). Treatment was started with cefotaxime 200mg/kg/day, vancomicine 60mg/kg/day and metronidazole 30mg/kg/day to cover gram-positive cocci including pneumococci, staphylococci, gram-negative and anaerobic bacilli; vancomycin was indicated to cover methicillin-resistant Staphylococcus aureus and penicillin-resistant pneumococcus. Six hours later he was admitted to the operating room by neurosurgery, which drained a purulent epidural and subgaleal collection by evacuation craniotomy. At 24hours, otorhinolaryngology performed endoscopic surgery on the nose and sinuses, finding left pansinusitis and findings compatible with Pott puffy tumour; cultures were taken in the two surgical acts, in the culture from the epidural empyema Group C haemolytic Streptococcus B grew. The patient continued antibiotic treatment for 4 weeks and was discharged.
Pott puffy tumour is a rare condition, with approximately 50 cases described, due to the antibiotic era and the antimicrobial management of sinusitis, which are generally related to its genesis. It is characterised by a well circumscribed mass in the frontal area, inflammation of the skin and collection of pus below the periosteum, which leads to osteomyelitis in the anterior table of the frontal sinus.1–4
It has an acute or subacute presentation, adolescents are most affected due to the development of the frontal sinus at the end of this stage and the characteristics of the diploic veins, which are a long venous system, without valves, with thinner walls that are more active in this period.1,2
The causes associated with its onset include: frontal sinusitis, maxillary, dental abscess, cocaine use, frontal trauma, fibrous dysplasia, malignant frontal sinus tumour, immunocompromised patients, late complication of a neurosurgical procedure and recurrences may occur after erosion of the bone table.1,5–7
The microorganisms related to the disease are generally the same ones that produce sinusitis, many of these of polymicrobial origin including: Streptococcus (alpha and beta haemolytics), gram-negative bacteria such as Haemophilus influenzae, anaerobes (Bacteroides, Prevotella, Fusobacterium and Peptostreptococcus spp.), and with lesser frequency Staphylococcus aureus. It is important to take cultures during surgical drainage, looking for microbiological identification to evaluate whether the treatment established is appropriate regarding the sensitivity profile of the microorganism.1–3,7
In the patient, a group C haemolytic Streptococcus B was isolated, related to contact with cattle and sheep, although the patient did not have contact with animals. Recent reports associate it with pharyngitis, bacteraemia, endocarditis or meningitis, although it is rare as a cause of frontal sinusitis.
Symptoms may be subtle, or oedema may suddenly develop in the frontal or orbital region, fever, headache, hyaline or purulent rhinorrhea. In some cases, there is an increase in intracranial pressure.1–3
For the diagnosis we rely on CT and MRI scans.1,7
The study of cerebrospinal fluid is performed when meningitis is suspected.
Intracranial complications are meningitis, epidural, subdural or intracerebral abscess, and thrombosis of the dural sinuses. The mortality rate has been estimated between 5% and 10%.2,7
Treatment includes surgical and medical management; surgical management includes sinus drainage, sequestrectomy, and subperiosteal abscess evacuation; empirical antibiotic treatment should be adequate, covering the bacteria associated with sinusitis, at high doses, and able to adequately penetrate the CNS; antibiotic treatment should be completed within 6–8 weeks after surgical drainage.1–3,7
Please cite this article as: Pérez-Yepes CA, Avilés-Robles M. Cefalea y edema fronto-orbitario de aparición súbita en un adolescente. Enferm Infecc Microbiol Clin. 2017;35:386–387.