Immigrant populations, especially those from endemic countries, living in the European Union (EU) suffer a disproportionate burden of HIV, delayed diagnosis and poorer access to antiretroviral treatment. While International Organisations are developing recommendations aimed at increasing the uptake of HIV testing, the feasibility and real outcomes of these measures remain unexplored. The aim of this review was, firstly to identify the recommendations of the main International Organisations (IO) on HIV testing in immigrants. Secondly, to describe the challenges for implementing and expanding HIV testing and counselling interventions targeting immigrants by interviewing key informants. The importance of HIV testing in immigrants is discussed, along with the appropriateness of universal HIV testing approaches vs most at risk targeted approaches. Also addressed is, pre- and post-HIV test counselling characteristics and community initiatives suitable to reach this population and, finally the legal issues regarding access to treatment for illegal immigrants.
Las poblaciones inmigrantes que viven en la Unión Europea, especialmente las originarias de países endémicos, sufren una carga desproporcionada de VIH, retraso diagnóstico y barreras de acceso al tratamiento antirretroviral. Mientras las organizaciones internacionales desarrollan recomendaciones para expandir el test de VIH, la factibilidad y los resultados reales de las medidas propuestas están aún por explorar. El objetivo de esta revisión es, en primer lugar, identificar las recomendaciones de los organismos internacionales sobre prueba de VIH a poblaciones inmigrantes. En segundo lugar, nuestro objetivo es describir los retos para implementar y expandir la prueba y el consejo de VIH dirigido a inmigrantes a través de entrevistas con informantes clave. En este artículo describimos la importancia de realizar la prueba en inmigrantes y discutimos la adecuación de las estrategias de cribado de VIH universal, frente a las estrategias de prueba dirigidas a colectivos en situación de especial vulnerabilidad. También se abordan las características del consejo previo y posterior a la prueba y las iniciativas desde la comunidad para alcanzar a esta población. Finalmente, analizamos cuestiones legales sobre el acceso al tratamiento de los inmigrantes en estatus ilegal.
HIV delayed diagnosis remains a major public health issue across Europe and worldwide.1,2 In many EU countries, migrants in particular have been found to be diagnosed late with HIV and to have poorer access and/or uptake of combination antiretroviral therapy (cART) than native populations.3–6 Data from the European Centre for Disease Prevention and Control (ECDC) shows that in 2013 the proportion of late HIV diagnosis (CD4 count <350cells/mm3 at diagnosis) was higher among migrants from countries with generalized epidemics (59%) compared to people who inject drugs (52%) and men who have sex with men (MSM) (37%).1 Several international organizations have recently published guidelines that underline the importance of promoting HIV testing as the basis for ensuring universal access to treatment and care.3,7,8 Administrative,9–12 legal,13,14 language13–18 and cultural barriers9,11,14,15,19 have been reported as obstacles in accessing HIV testing services among migrant populations.
In the European Union/European Economic Area (EU/EEA), two main approaches have been identified aimed at promoting HIV testing20: general population approaches in health-care settings and targeted approaches aimed at key populations. The first approach is based on the success of antenatal screening – a strategy that has achieved excellent coverage of HIV testing including migrant and ethnic minority women.21 Within the second approach, different and innovative interventions have been developed including offering HIV rapid testing in non-traditional health-care settings and outside normal working hours22; provision of point-of-care testing by non-governmental organizations (NGOs) and community-based organizations (CBOs) and testing by outreach services, mobile clinics and other non-clinical settings, such as hair salons or sporting events among others.23–25 The feasibility and benefits of targeted approaches however remains largely unexplored.
This review firstly aims to identify the main International Organizations (IO) recommendations about HIV testing in migrants. Reviewed documents were issued by World Health Organization,8,26,27 ECDC,7 International Organization for Migration (IOM)28 and International Labour Organization (ILO), IOM and Joint United Nations Programme on HIV/AIDS (UNAIDS).29 Secondly, this article intends to describe the challenges for implementing and expanding these strategies interviewing 24 key informants from both governmental and non-governmental organizations. Participants were mainly academicals researchers with a recognized career, policy makers from EU countries and NGO's representatives working on HIV from Belgium, France, Germany, Italy, Portugal, Spain, Sweden USA and UK. Individual and group interviews were performed.
The importance of HIV testing in migrants: universal HIV screening vs targeted approachesMost documents explicitly identify the benefits of HIV testing at individual and community level. The benefits derived from cART uptake are noted; overall increase of life expectancy, decrease of morbidity and mortality and reduction of mother to child transmission; testing HIV positive can also lead to behaviour change and prevention of further HIV transmission. On the same line, the reduction in HIV viral load – and thus transmission risk – derived from cART uptake is one of the main benefits at community level. The 2010 WHO Guide8 states: “the importance of this for HIV prevention is enhanced in settings where antiretroviral treatment (cART) is available and accessible to all who need it, given its value in reducing viral load and the amount of virus circulating in the community”. This recommendation is not necessarily directed towards the whole population, but can target people with high risk exposure when the HIV epidemic is concentrated in “key populations at risk”.
Key informants from Belgium, Italy, Portugal, and Spain said they were discussions at country level as to whether move towards incorporating opt-out routine HIV testing for the general population. In general, participants underlined the need to frame at a global level the aforementioned initiatives and to address other complex issues as well:
“Individual strategies to fight HIV are necessary but not sufficient. We must address the social determinants of health such as poverty, access to health care, racism and discrimination” (Policy Maker).
Targeted approaches were considered as more cost effective by some of the interviewees. However, a number of participants believed that a general population approach may be more acceptable to service providers and users. Service providers prefer to offer screening for medical reasons. Service users may perceive HIV testing that is offered to people on the basis of the colour of their skin or their country of origin as discriminatory.
“Epidemiologically and financially it makes sense to talk of high prevalence groups – for example, migrants from SSA (Sub-Saharan Africa) and MSM – but it does not make sense in terms in delivering services and the risk of discrimination and stigma. The history of migrants is different from that MSM. The latter had a solid network of solidarity that helped them to withstand potential stigma and discrimination, whereas migrants do not. Although it is tempting epidemiologically to target them as a group, the strategy needs to be embedded in the general population” (Group interviewee).
In fact, a number of respondents identified the success of antenatal testing of HIV as a good example of how an opt-out approach was a strategy that has led to dramatic reductions in mother to child HIV transmission across Europe. It was also pointed out that recommendations based on HIV testing within health care settings may not reach the most vulnerable as often people may not access health care services.
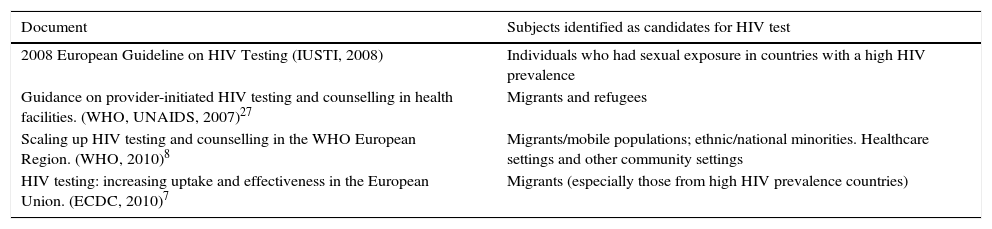
Identifying migrants as candidates for HIV testAll reviewed international guidelines identify migrants as at risk for HIV infection but only three8,27,28 explicitly recommend testing them for HIV infection, as seen in Table 1.
Documents that recommend HIV testing migrants and ethnic minorities.
| Document | Subjects identified as candidates for HIV test |
|---|---|
| 2008 European Guideline on HIV Testing (IUSTI, 2008) | Individuals who had sexual exposure in countries with a high HIV prevalence |
| Guidance on provider-initiated HIV testing and counselling in health facilities. (WHO, UNAIDS, 2007)27 | Migrants and refugees |
| Scaling up HIV testing and counselling in the WHO European Region. (WHO, 2010)8 | Migrants/mobile populations; ethnic/national minorities. Healthcare settings and other community settings |
| HIV testing: increasing uptake and effectiveness in the European Union. (ECDC, 2010)7 | Migrants (especially those from high HIV prevalence countries) |
The 2010 ECDC guideline in the chapter “Whom to test?” recommends each country to know its epidemic and identify groups most at risk. Among the groups considered especially at risk for HIV, migrants are included (especially those from countries with higher prevalence).
However, targeting migrants for HIV testing has potential disadvantages, especially for migrants who may face unique legal and administrative barriers compared to the general population. Among the disadvantages described were the dangers of coercive testing, with implications on residency permits, fear of deportation and lack of rights to access treatment and care for irregular migrants. Fear of discrimination and deportation were quoted by various interviewees as the strongest barrier to HIV testing in migrant populations. Discussions around the stigma and fear of discrimination surrounding HIV infection repeatedly came up. This is a particular concern in migrant communities where many rely on the support from their own community network for day to day survival. Criminalization of HIV transmission was also mentioned and how legal rulings were felt to have disproportionally affected migrants from Sub-Saharan Africa (SSA) in some countries.
“Stigma around HIV in the countries of origin of some migrants is very strong and perhaps they bring it with them when they move to a new country. (…) When an HIV-positive result is given, there is a brutal drop in self-esteem, because the previous concept that they had had about HIV was so negative. If this can be true for most of the population, for some immigrants it is even worse.” (NGO representative).
The importance of counselling, pre and post-test informationGuides elaborated by IUSTI, IOM, WHO, ECDC and UNAIDS collect practical information about the desirable contents of pre- and post-test counselling. IOM has developed a specific document for counsellors: IOM Guide for HIV Counsellors,28 in which the characteristics and content of counselling process are carefully specified.
Regarding pre-test counselling, ECDC considers that a brief pre-test discussion, about the benefits of testing and practical arrangements for taking the test and giving results, would be effective to increase HIV testing uptake. IUSTI states that the main objective of this phase is to obtain informed consent and establish a pre-test discussion about HIV issues with the client, while IOM considers that pre-counselling is the best opportunity to educate and inform individuals on HIV and AIDS. In the IOM guide, this moment is weighed up as a process that can help to reduce stigma in the community. Guidelines developed by WHO and UNAIDS are based on PITC (Provider-initiated testing and counselling), and the principal aim of this stage is to discuss with the patient the reasons of HIV testing recommendation. This guide states that counselling can be performed both individually and in a group session.
Among key informants there were mixed opinions about pre-test counselling length. Many participants felt it was a good strategy as lengthy pre-test counselling may dissuade people from testing. Some participants consider that migrants can be overwhelmed by the different issues and events related to their adaptation to a new country making them avoid time-consuming activities; besides, the concept of counselling might not necessarily be understood by most of them. On the other hand, some participants fear that an abbreviated counselling might be insufficient to tackle migrants’ misconceptions regarding HIV infection.
Guidelines consider post-test counselling as a part of HIV testing process regardless of test result, although content varies depending on the result. Overall, for those testing negative, this moment would be employed to stress health benefits of prevention strategies. For positive results, post-counselling has to satisfy all questions related with care referral, information about transmission routes and risk behaviours. Moreover, at this stage the individuals should be given information on key institutions or other resources that can provide them with emotional support to cope with the result.
Legal issues regarding access to treatmentOne of the objectives proposed by the Dublin Declaration (2004)26 was “By 2005, provide universal access to effective, affordable and equitable prevention, treatment and care including safe anti-retroviral treatment to people living with HIV/AIDS in the countries in our region”. Despite efforts made in this direction, there are still many countries in which migrants of uncertain status have no formal access to HIV treatment.
The 2010 WHO guidelines8 and the ECDC guidance7 state that testing by itself is not the goal: countries have to provide treatment, care and support to all individuals diagnosed with HIV. Countries have to ensure care and referral to those individuals tested. The document oh WHO expresses concern about the lack of treatment in many countries of the region, especially for the most marginalized populations like migrants, and stresses the need to expand cART coverage to these vulnerable populations.
In this same sense, participants felt that promotion of HIV testing for migrants of uncertain residency when access to ART is not guaranteed was an important issue that raised a number of ethical questions. The unanimous feeling was that HIV testing must be linked to care for the programme to be effective. However, interviewees also acknowledged that, unfortunately even in Europe, there are some irregular migrants that are not entitled to antiretroviral treatment. There were mixed views on what to do in these circumstances which ranged from not recommending HIV testing unless access to antiretroviral medication can be guaranteed to recommending the test in spite of this while highlighting the need of trust building and avoidance of paternalism.
“It makes no sense to perform the test when the disclosure of a positive result does not guarantee access to care (…). Denying access to care is opposite to Human Rights Declaration, in which access to health care is guaranteed to all individuals. It is a paradox to allow the person to access the test and then not allowing them to be treated” (Academic researcher).
“HIV testing on its own has been proven to be good, it has been shown to be beneficial in reducing unsafe sexual behaviour and thus, decreasing HIV transmission. Besides, even if cART may not be entitled, other supportive care aspects can be provided such as prophylaxis and treatment against opportunistic infections” (Policy maker).
On-going initiatives promoting HIV testing in the community targeting migrants and ethnic minoritiesECDC guidance consider that to reach migrants will require expanding testing not only in clinical settings but in a number of community settings.7 The document “Scaling up HIV testing and counselling in the WHO European Region”8 points out the existing barriers to access traditional health services for most-at-risk populations. Strategies aimed at increasing access and uptake of HIV testing has to be developed. The community's participation in the design of interventions is necessary in order to identify adequate and acceptable practices related with HIV testing.27 Examples proposed by documents, based on client-initiated strategy, include outreach programmes: services by mobile clinics or in community settings. The principle behind it is to offer the HIV test “where they are”, through non-governmental and community-based organizations.
ILO guide addresses the importance of “ensuring, through funding public-health services, non-governmental and private organizations that international labour migrants and their families have the same access as nationals to HIV prevention, treatment, care and support programmes which are sensitive to gender and culture, and in a language or medium the migrant worker can understand”.29
Promoting HIV testing in the community was viewed as one of the key aspects to the success of the implementation of guidelines for interviewed participants. Developing point of care testing (POCT) within CBOs and NGOs was seen as an excellent initiative by most respondents. Participants stressed the need to find strategies that were flexible, allowing migrants to access HIV tests in their community organizations’, while ensuring quality across the testing process. Confidentiality, post-test counselling and immediate linkage to specialist HIV care were identified as needing to be guaranteed and all testing initiatives should fulfil all ethnical and technical requirements. Some participants consider confidentiality concerns are behind some people not wanting to be tested in their own community, preferring to attend an STD clinic far from their homes. Developing more CBO POCTs that provide people with information about where these sites are located is essential. Unsupervised HIV testing could lead to irregular migrants being forced into being tested without appropriate counselling and health care referrals.
ConclusionsBenefits of expanding HIV testing to reach migrant populations have been recognized by all participants. However, reaching migrants and ethnic minority populations with HIV testing and counselling programmes remains a challenge. Migrants and ethnic minorities are very heterogeneous populations, determined by country of origin, ethnicity, gender, sexual orientation, religion, legal status and time in the country of destination. While some groups of migrants will be reached through general population programmes, other groups of migrants may be reached through more targeted approaches.
Several studies have shown the differential burden of HIV late diagnosis among migrants compared to the autochthonous population,1 which is of critical importance as it is well-known that late diagnosis is associated with increased morbidity and mortality. Implementing effective and non-discriminatory HIV testing programmes is of utmost importance. HIV testing strategies directed towards the general population have been successfully implemented in antenatal settings, in which HIV testing uptake in migrant women is not different from non-migrants.30 In other settings where strategies for general populations are being implemented,12 uptake of HIV-test by migrants seems to be successful, though little data are available so far. This strategy avoids the perception of stigmatization associated with risk-group targeted programmes.10 In most clinical settings HIV testing is offered together with pre-test information and no lengthy pre-test counselling. Interviewees expressed ambivalence as to whether this is adequate for migrant populations as it is felt that a lot of misconceptions regarding HIV infection can be tackled during counselling sessions, particularly those related to the stigma within the community.
Participants stated engagement with the communities and building partnership is fundamental for testing at community sites and for developing cultural sensitive interventions. The documented barriers to accessing HIV testing services are linked with the overall vulnerability of migrants and ethnic minorities. Additionally, poverty and socio-economical disadvantages result in low priority assignation to health in general and HIV in particular.10,13 General population approaches should deal with the heterogeneous sub-population groups of migrants and their perceptions about these general interventions. Traditional gender roles culturally assigned to men and women in some migrant communities may deter heterosexual men and women as well as MSM from HIV testing. While women are reached through antenatal testing, reaching men is more challenging and various initiatives to stimulate partner testing in the context of antenatal testing have been proposed.
Innovative strategies are needed to emphasize community participation. Mentioned options include broadening the scope of facilities performing the test, strengthening proactive testing strategies, putting in place outreach programmes based on community approaches, which could rely on POCT and rapid testing, offering the test where people live, work or spend their leisure time, expanding testing hours and involving NGOs and CBOs. Several studies have shown the benefits of this type of interventions and de-stigmatization of HIV testing within the communities.22,23,25 Innovative interventions have demonstrated their effectiveness particularly among migrant MSM, a particularly at-risk group traditionally invisible to HIV prevention activities and facing various and multiple forms of discrimination.24
However, care has to be taken into account when designing an HIV testing programme targeting migrant communities not to further stigmatize this group and to assure that testing is performed with maximum quality.
All interviewees insist in the need of linking HIV testing with care and treatment. The HIV treatment cascade – also referred as “HIV care continuum” – developed in 2010 by Gardner et al.31 aimed to identify chances to improve services for people living with HIV across the HIV continuum of care. The final objective of this model would be to achieve hypothetical scenario in which all HIV positive individuals are in treatment, community viral load is suppressed and infectivity of new individuals does not take place. The benefits of HIV testing at the community level is also supported by International Organizations such as WHO and ECDC in their respective HIV testing guidelines.7,8 The biggest benefit of HIV testing is attained through universal access to treatment and care, prevention and support services, which must be the basis of the national HIV testing strategies. Furthermore, adequate treatment of HIV does not only have individual benefits, but also prevents HIV transmission and has been demonstrated to be a cost-effective intervention.32–34
FundingThis work was supported by the European Centre for Disease Prevention and Control under Grant (OJ/2009/04/02-PROC/2009/009), Spanish Network of HIV/AIDS Research [RIS-RD12/0017/0018] and the Biomedical Research Centre Network for Epidemiology and Public Health [CIBER de Epidemiología y Salud Pública].
Conflict of interestThe authors declare no conflict of interest.
We would like to thank all the experts participating in the interviews for their valuable input into this work.