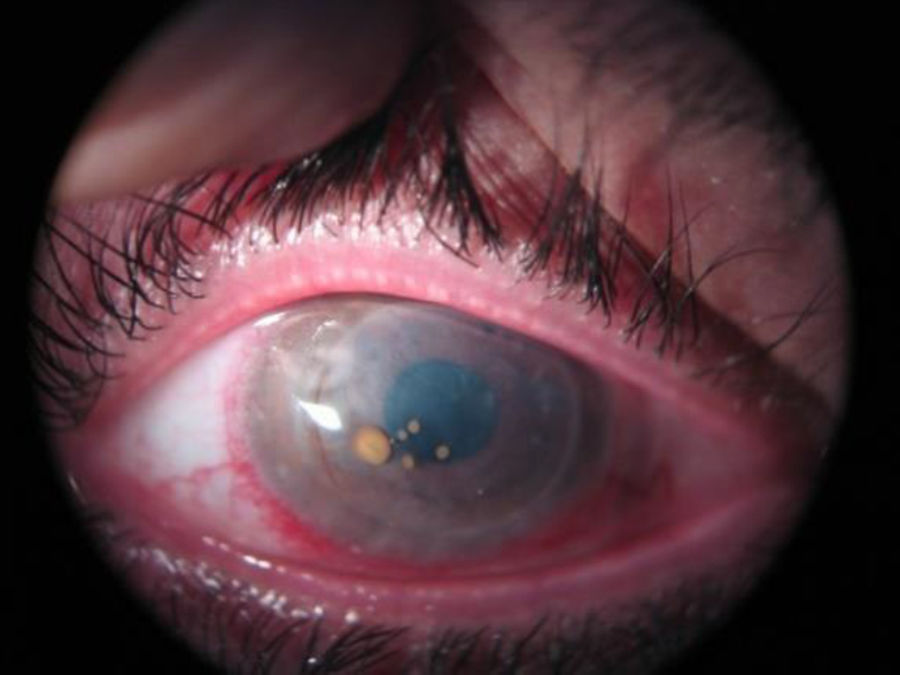
A 36-year-old man diagnosed with Keratitis-Ichthyosis-Deafness (KID) syndrome who had loss of vision in his right eye. He had been treated with penetrating keratoplasty on four previous occasions (the last time four years earlier) because of ulcers, corneal leucoma and infections caused by Candida albicans and Pseudomonas aeruginosa. The patient is forced to wear permanent contact lenses because of corneal epithelialisation problems related to his illness. Slit lamp examination revealed diffuse opacification of the corneal graft, with spontaneous opening of the previous surgical incision. Several bright, brownish, nodular lesions were observed closely attached to the surface of the cornea (Fig. 1). After no response to the usual antibiotic treatment with topical vancomycin and ceftazidime, penetrating keratoplasty was performed once again, this time for therapeutic and diagnostic purposes.
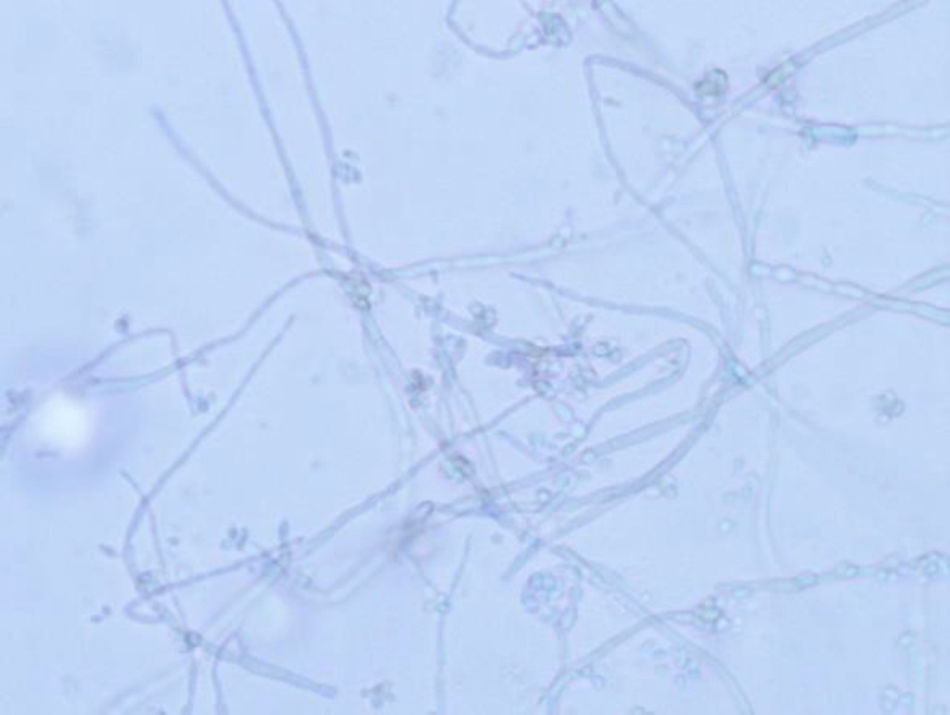
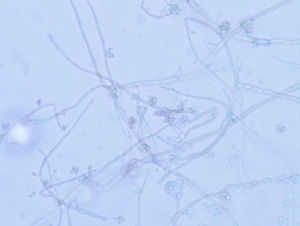
The cornea was processed for culture of bacteria, mycobacteria and fungi. At three days, a number of colonies were observed on Sabouraud agar, acquiring an olive-black colour as they grew (Fig. 2). The same colonies were also isolated in the Lowenstein medium incubated at 30°C. Microscopic examination revealed thick, irregular septate hyphae with hyaline or light brown, oval or circular, single-celled conidia arranged in groups attached to the hyphae, multiplying by budding (Fig. 3). Identification was performed by MALDI-TOF mass spectrometry (Bruker, Germany) from the isolated colonies and the result obtained was Exophiala dermatitidis, with a score higher than 2. The strain was sent to the Spanish National Microbiology Centre, where the identification was confirmed through the sequencing of the Internal Transcribed Spacer region, and antifungal susceptibility testing was carried out using the European Committee for Antimicrobial Susceptibility Testing reference technique.
OutcomeAs fungal infection was suspected, after the keratoplasty, the patient was treated with oral voriconazole (200mg twice daily) for three weeks, 1% voriconazole eye drops every two hours for one week and then every four hours for three weeks, and 0.5% levofloxacin eye drops hourly for two weeks and then every four hours for another two weeks. During that time, oral corticosteroid therapy was used to prevent corneal rejection. There was no relapse of the infection, with a transparent corneal graft after one year.
CommentsExophiala dermatitidis (E. dermatitidis), also known as Wangiella dermatitidis and one of the so-called “black yeasts”, is a dematiaceous fungus which, like all of this group, has a dark pigmentation as a result of its melanin content. These fungi are widely distributed in the environment, mainly in the soil, and can produce a wide range of diseases. Infection usually occurs by inoculation or trauma and generally affects the skin and soft tissues, although central nervous system, lung and systemic infections have also been reported, the latter mainly in immunosuppressed patients.1 Various studies have described corneal infections, usually after surgery, caused by E. dermatitidis and other species in the same genus.2–5
In the culture of the sample in Sabouraud agar the colonies of Exophiala spp. can be detected in less than 7 days, although they sometimes require more time, and they acquire a characteristic olive-black or dark brown colour. Although E. dermatitidis has some peculiar morphological and physiological characteristics (the conidia form aggregates, it grows at over 40°C, it does not use nitrites), traditional identification of these fungi at a genus and species level using morphological or biochemical criteria only is very difficult, because of the variable manner in which they express their characteristics and the low degree of differentiation.1
Over the last twenty or so years, molecular techniques have facilitated the identification of these fungi, as well as detecting new species and reorganising their classification,6 but they are complex and expensive techniques that are not available to all laboratories. Mass spectrometry (MALDI-TOF) has proven to be a powerful tool for the identification of bacteria and fungi, especially yeasts and, although with greater difficulty for the moment, filamentous fungi. Several recent studies have demonstrated that mass spectrometry is a reliable, rapid and cost-effective tool for the identification of E. dermatitidis and other fungi in this genus which are difficult to identify by conventional methods.7–9
In terms of treatment, although efficacy in vivo has not yet been determined, in vitro susceptibility tests demonstrate that E. dermatitidis is susceptible to amphotericin B, itraconazole, voriconazole and posaconazole, while the echinocandins show low activity.10–12 In our strain, low MIC (mg/l) values were obtained for voriconazole (0.12), itraconazole (0.12), posaconazole (0.06) and amphotericin B (0.25), and high MIC values for caspofungin (16), micafungin (2) and anidulafungin (>4).
This case demonstrates the need to think of uncommon opportunistic microorganisms in patients with keratitis with chronic corneal problems, immunosuppressed patients and contact lens wearers, as well as the importance of sending appropriate samples to the laboratory to allow the recovery of these microorganisms. We also want to highlight the great advances that the use of mass spectrometry (MALDI-TOF) in microbiology laboratories has meant for the rapid identification of these fungi.
To Dr Ana Alastruey, of the Spanish National Centre of Microbiology's Mycology Laboratory, for her collaboration in the molecular identification and susceptibility study of this strain.
Please cite this article as: Bermúdez-Ruiz MP, Gómez-Moyano E, Sainz-Rodríguez R, Garín-Ferreira R. Queratitis infecciosa en paciente con síndrome KID. Enferm Infecc Microbiol Clin. 2019;37:56–57.