The COVID-19 pandemic has changed the circulation of some viruses associated with acute bronchiolitis. We analyzed the epidemiology of bronchiolitis admissions during the COVID-19 pandemic compared with 8 previous epidemic seasons.
MethodsAn observational and ambispective study was performed, including infants admitted with bronchiolitis in a tertiary hospital during 2 periods: COVID-19 pandemic (15th March 2020 to 3rd August 2021) and pre-pandemic (1st September 2012 to 14th March 2020). Demographic, clinical data and etiologies were collected.
ResultsFive hundred ten patients were hospitalized with bronchiolitis: 486 in the pre pandemic period with an average of 61 admissions per season vs 24 during the pandemic, observing a 60.7% reduction in bronchiolitis admissions. During the pandemic, bronchiolitis outbreak was delayed until spring-summer 2021. Respiratory syncytial virus was the most frequent etiological agent in both periods.
ConclusionWe observed a change in the seasonality of bronchiolitis during the pandemic COVID-19, possibly influenced by control measures against SARS-CoV-2.
La pandemia COVID-19 ha modificado la propagación de ciertos virus respiratorios causantes de bronquiolitis aguda. Analizamos la epidemiología de los ingresos por bronquiolitis durante la pandemia COVID-19 en comparación con 8 temporadas epidémicas anteriores.
MétodosEstudio observacional ambispectivo, que incluyó lactantes con bronquiolitis ingresados en un hospital terciario durante dos períodos: pandemia COVID-19 (15 marzo-2020 a 31 agosto-2021) y pre-pandemia (1 septiembre-2012 a 14 marzo-2020). Se recogieron características demográficas, clínicas y etiología.
ResultadosIngresaron 510 pacientes por bronquiolitis: 486 en el período pre-pandemia con una media de 61 ingresos por temporadavs 24 durante la pandemia, observándose una reducción de ingresos del 60,7%. Durante la pandemia, el brote epidémico se inició con retraso abarcando la primavera-verano 2021. El virus respiratorio sincitial fue el agente etiológico más frecuente en ambos períodos.
ConclusionesObservamos un cambio estacional de la bronquiolitis durante la pandemia COVID-19, probablemente influenciado por las medidas de control frente a SARS-CoV-2.
Acute bronchiolitis (AB) is the most common lower respiratory tract infection in infants and the leading cause of their hospitalisation. The main aetiological agent is the respiratory syncytial virus (RSV), which usually presents a very characteristic seasonal epidemiological pattern, with peaks of maximum incidence during the winter months. Between 10% and 20% of cases may be caused by other viruses1.
The COVID-19 pandemic has led to a change in the epidemiology of common respiratory viruses, with changes in the seasonal presentation of AB observed in some countries around the world2–5. The objective of this study is to analyse the epidemiology of hospitalisations for AB during the COVID-19 pandemic compared to previous epidemic seasons.
MethodsAn observational, ambispective study that included children under two years of age admitted for AB to the Hospital Clínico Universitario de Valladolid. It is the Paediatric Department of a tertiary hospital that provides specialised healthcare and critical care coverage to 95,960 children under 14 years of age in an area of the Community of Castile and León, Spain.
From 15 March, 2020, to 31 August, 2021 (COVID-19 pandemic), all infants admitted with a diagnosis of AB according to the McConnochie criteria6, which consider AB as the first episode of respiratory distress coursing with wheezing and/or crackling rales and is preceded by catarrhal clinical symptoms of the upper airways, which affects children under two years of age, were prospectively included. A comparison was made with eight previous epidemic seasons, from 1 September, 2012 to 14 March, 2020 (pre-pandemic period), retrospectively including patients diagnosed with AB at discharge, according to the International Classification of Diseases ICD-9 or ICD-10 (codes: 466.11, 466.19, J21.0, J21.1, J21.8, J21.9), excluding children who did not meet the aforementioned McConnochie criteria.
During the two periods, aetiology was investigated in nasopharyngeal lavage samples with the following molecular diagnostic tests: Luminex® NxTAG Respiratory Pathogen Panel (Luminex Molecular Diagnostics, Toronto, Canada) or FilmArray Respiratory Panel (BioFire Diagnostics, Salt Lake City, UT, USA). These tests detected 17 viruses and three bacteria: RSV, adenovirus, coronavirus (229E, HKU1, OC43 and NL63), human metapneumovirus, rhinovirus/enterovirus, influenza (A, A/H1, A/H1-2009, A/H3), influenza B, parainfluenza (1, 2, 3 and 4), Chlamydophila pneumoniae, Mycoplasma pneumoniae, Legionella pneumophila or Bordetella pertussis. In addition, during the pandemic, an RT-PCR test was performed to detect SARS-CoV-2.
Demographic characteristics, comorbidities, clinical manifestations, aetiology and presence of viral co-infections were collected.
The statistical analysis was performed with the IBM SPSS® 27.0 (SPSS Inc., Chicago, IL, USA) statistics package. The Mann-Whitney U test was used for the analysis of continuous variables and Fisher's exact test or Pearson's chi-square test was used for categorical variables.
The study was approved by the hospital's Medicines Research Ethics Committee (registration number PI 20-1902).
ResultsA total of 509 patients diagnosed with AB were admitted during the study period. In the pre-pandemic period, there were 485 admissions with an average of 61 hospitalisations per epidemic season. The beginning and end of each season ran from October to April or May, with the peak incidence observed during December or January.
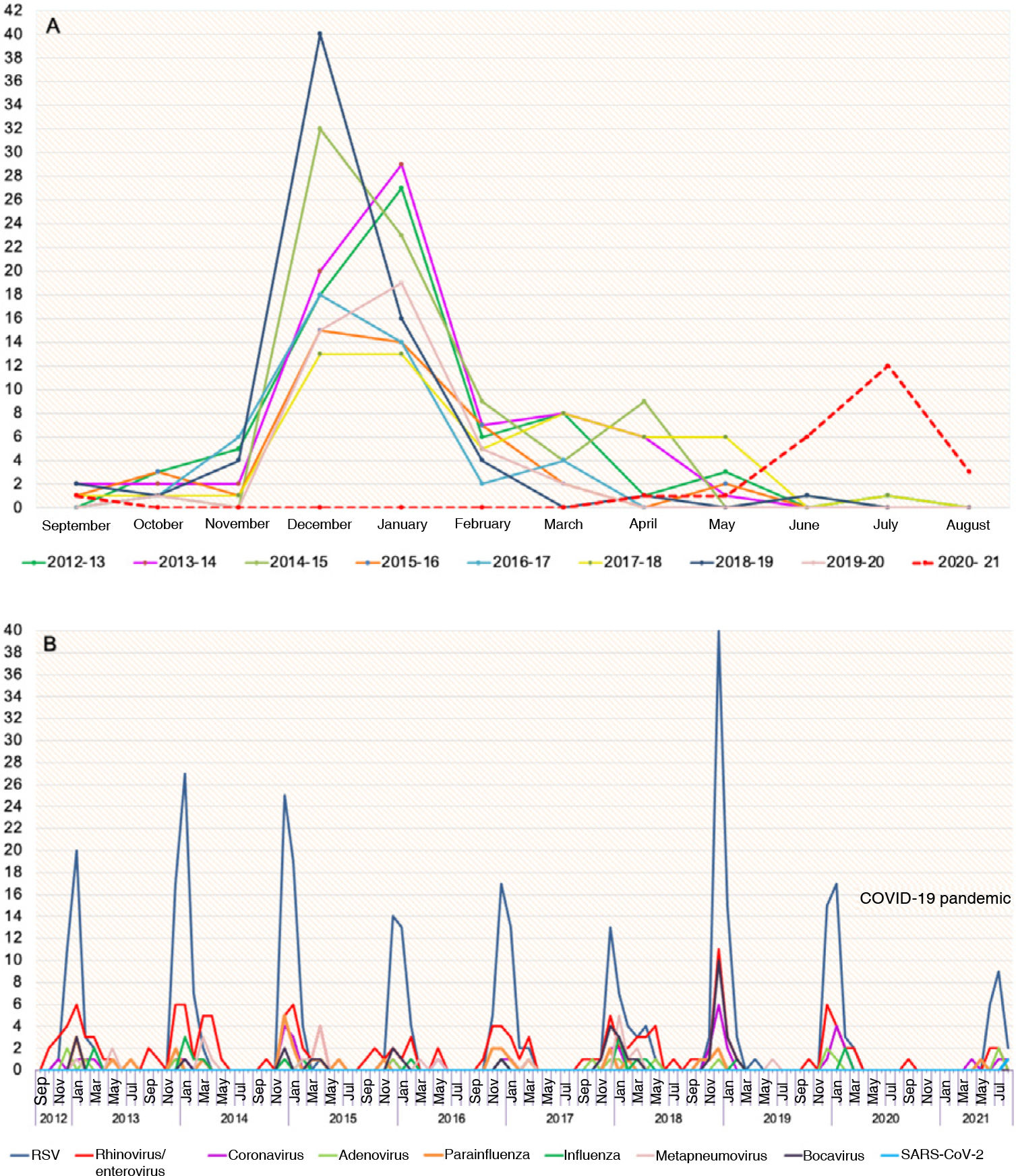
During the COVID-19 pandemic, there was a single admission for AB in September 2020 and there were no patients hospitalised for this reason during the autumn-winter 2020–2021 months, and the first case of the epidemic outbreak was recorded in April 2021. We observed a delay in the beginning of the epidemic season, which spanned spring-summer, with a peak incidence in July. Furthermore, the number of hospitalisations was lower than in previous seasons, with a total of 24 admissions for AB recorded, a percentage reduction of 60.7% in admissions. Fig. 1A shows the number of monthly admissions for AB during each epidemic season.
The aetiology of AB was investigated in 491 patients and at least one respiratory virus was detected in 95.3% of the cases. RSV was the most frequent aetiological agent, being found in isolation or in combination with other viruses in 70.7% of the patients, with no differences observed between the two periods.
Fig. 1B shows the seasonal distribution of the different respiratory viruses throughout the seasons studied. During the pre-pandemic period, RSV was usually detected between October and March, while in the pandemic the incidence peak occurred in July, with a total of 17 admissions recorded for this cause. Rhinovirus/enterovirus was present in all seasons at different times of the year, especially between September and May. During the pandemic, rhinovirus/enterovirus was isolated in five of the 24 patients admitted for AB (20.8%), one of them in September 2020 and the others in June and July 2021. Other viruses detected during the spring-summer of 2021 were coronaviruses OC43 and 229E, adenovirus, parainfluenza 3 and there was one admission of AB for SARS-CoV-2. Although human metapneumovirus, influenza and bocavirus were isolated in the pre-pandemic period, these three viruses were not detected during the COVID-19 pandemic. In addition, there was a lower frequency of viral co-infections in the pandemic period (35.8% vs. 20.8%; P=.103), although this difference was not statistically significant.
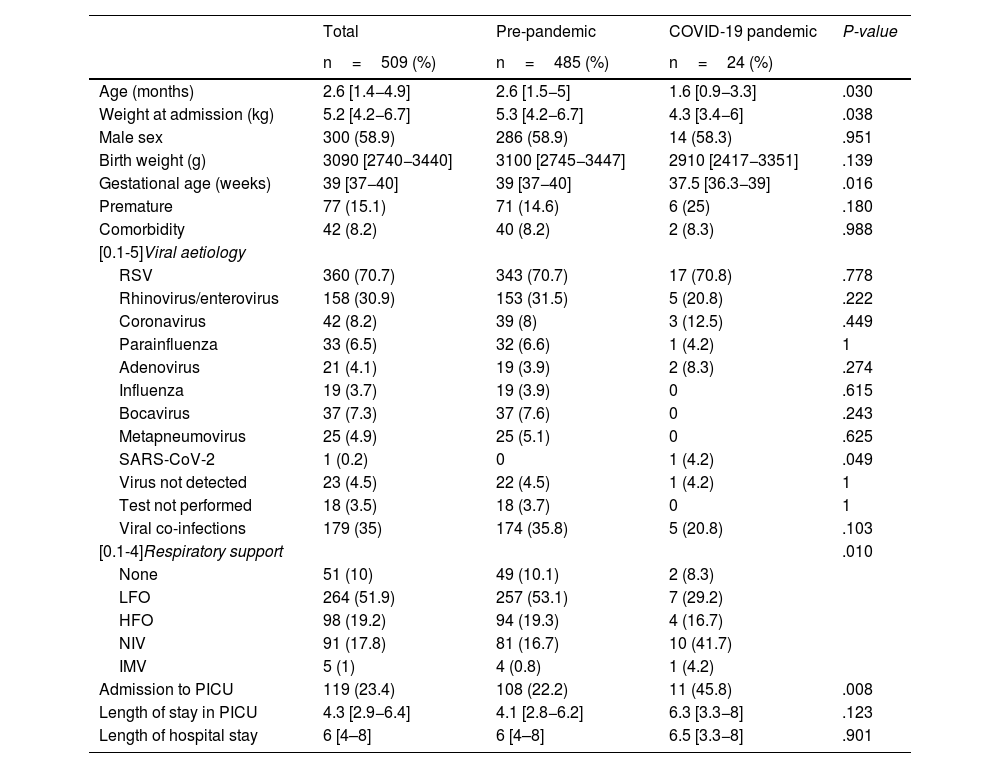
Finally, in relation to the demographic and clinical characteristics, the patients admitted during the pandemic presented lower medians of gestational age, age and weight at admission compared to the pre-pandemic group, and a higher proportion of admissions to the Paediatric Intensive Care Unit and a greater use of both invasive and non-invasive mechanical ventilation was recorded, with these differences being statistically significant between the two periods. Table 1 shows the characteristics of the patients with AB admitted during the pre-pandemic and pandemic periods.
Patient demographic and clinical characteristics during the two periods.
| Total | Pre-pandemic | COVID-19 pandemic | P-value | |
|---|---|---|---|---|
| n=509 (%) | n=485 (%) | n=24 (%) | ||
| Age (months) | 2.6 [1.4−4.9] | 2.6 [1.5−5] | 1.6 [0.9−3.3] | .030 |
| Weight at admission (kg) | 5.2 [4.2−6.7] | 5.3 [4.2−6.7] | 4.3 [3.4−6] | .038 |
| Male sex | 300 (58.9) | 286 (58.9) | 14 (58.3) | .951 |
| Birth weight (g) | 3090 [2740−3440] | 3100 [2745−3447] | 2910 [2417−3351] | .139 |
| Gestational age (weeks) | 39 [37−40] | 39 [37−40] | 37.5 [36.3−39] | .016 |
| Premature | 77 (15.1) | 71 (14.6) | 6 (25) | .180 |
| Comorbidity | 42 (8.2) | 40 (8.2) | 2 (8.3) | .988 |
| [0.1-5]Viral aetiology | ||||
| RSV | 360 (70.7) | 343 (70.7) | 17 (70.8) | .778 |
| Rhinovirus/enterovirus | 158 (30.9) | 153 (31.5) | 5 (20.8) | .222 |
| Coronavirus | 42 (8.2) | 39 (8) | 3 (12.5) | .449 |
| Parainfluenza | 33 (6.5) | 32 (6.6) | 1 (4.2) | 1 |
| Adenovirus | 21 (4.1) | 19 (3.9) | 2 (8.3) | .274 |
| Influenza | 19 (3.7) | 19 (3.9) | 0 | .615 |
| Bocavirus | 37 (7.3) | 37 (7.6) | 0 | .243 |
| Metapneumovirus | 25 (4.9) | 25 (5.1) | 0 | .625 |
| SARS-CoV-2 | 1 (0.2) | 0 | 1 (4.2) | .049 |
| Virus not detected | 23 (4.5) | 22 (4.5) | 1 (4.2) | 1 |
| Test not performed | 18 (3.5) | 18 (3.7) | 0 | 1 |
| Viral co-infections | 179 (35) | 174 (35.8) | 5 (20.8) | .103 |
| [0.1-4]Respiratory support | .010 | |||
| None | 51 (10) | 49 (10.1) | 2 (8.3) | |
| LFO | 264 (51.9) | 257 (53.1) | 7 (29.2) | |
| HFO | 98 (19.2) | 94 (19.3) | 4 (16.7) | |
| NIV | 91 (17.8) | 81 (16.7) | 10 (41.7) | |
| IMV | 5 (1) | 4 (0.8) | 1 (4.2) | |
| Admission to PICU | 119 (23.4) | 108 (22.2) | 11 (45.8) | .008 |
| Length of stay in PICU | 4.3 [2.9−6.4] | 4.1 [2.8−6.2] | 6.3 [3.3−8] | .123 |
| Length of hospital stay | 6 [4–8] | 6 [4–8] | 6.5 [3.3−8] | .901 |
Categorical variables are expressed as absolute values and percentages (%) and quantitative variables as median and interquartile range [IQR].
HFO: high-flow oxygen therapy; IMV: invasive mechanical ventilation; LFO: low-flow oxygen therapy; NIV: non-invasive ventilation; PICU: Paediatric Intensive Care Unit.
During the COVID-19 pandemic, there was a change in the seasonal pattern of AB, as shown by the results of this study.
Every year, when winter arrives, respiratory virus infections increase and cases of AB rise to epidemic levels, creating a significant demand for healthcare with a risk of saturating the health system and having a significant socioeconomic impact. However, during the 2020–2021 autumn-winter season, this disease was practically non-existent in Spain and other countries3,5,7–12.
Our data show an unusual reappearance of AB cases during the spring and summer months in one area of Spain. This late outbreak has also been observed in other countries13,14. In Australia, the mean number of hospitalisations for AB in the autumn-winter 2020 season was 85.9% lower than expected, with an upsurge in RSV cases observed during spring-summer which exceeded the winter epidemic peaks of previous seasons in magnitude12,13. In France, the AB epidemic period started late, in February 2021, peaked at the end of March and lasted until June14. This outbreak was smaller than other pre-pandemic seasons, similar to what was observed in our study cohort.
In relation to this epidemiological change, most authors agree that the measures applied to control the transmission of SARS-CoV-2, such as hand hygiene, the use of face covering and social distancing, contributed to reducing the circulation of other respiratory viruses2,4,8,12. The temporal relationship between the relaxation of social restrictions in Spain in May 2021 and the re-emergence of respiratory viruses such as RSV would appear to support this hypothesis. The mandatory use of face covering in enclosed spaces could have contributed to the epidemic outbreak being smaller than in other years, partly limiting the circulation of certain viruses, which would account for the lower percentage of co-infections.
There is also the theory of the ecological niche of viruses, referring to the place they occupy in the ecosystem, which varies dynamically depending on weather conditions and the presence of other pathogens. Thus, when a seasonal virus enters the environment, it usually displaces other viruses, with positive interactions also observed between them15. This phenomenon of competition or cooperation between viruses is evident every year when there is a fall in RSV cases with the start of the influenza epidemic. However, RSV can coexist with other viruses such as rhinovirus or metapneumovirus. According to this hypothesis, the circulation of SARS-CoV-2 in 2020 could have displaced other viruses, with a spike in common respiratory virus infections being observed as the incidence of COVID-19 diminished.
Classically, the temporal pattern of RSV circulation has been related to certain meteorological factors such as low temperatures and high relative humidity, conditions observed in the autumn and winter seasons in countries with temperate climates. However, our data demonstrate that these climatic conditions are not essential for the activity and spread of this virus, since the peak incidence of RSV shifted to the spring-summer months and was apparently unrelated to the weather.
This study provides information on the characteristics of the patients during the two periods. During the pandemic, we saw infants with a lower gestational age, lower age and weight at admission, which could account for the higher proportion of admissions to the PICU. These results should be interpreted with caution given the small sample size of the hospitalised group during the pandemic. It would be useful to have multicentre studies that analyse the characteristics of infants with AB during the COVID-19 pandemic to draw adequate conclusions in this regard.
Although some authors have speculated on the appearance of a delayed outbreak of AB in Spain during the COVID-19 pandemic7,8, to our knowledge, this is the first study to describe this particular epidemiological phenomenon, providing results about the seasonal behaviour of different respiratory viruses over several seasons in an area of Spain. It would be of great interest to continue to have similar and broader records in the coming years.
The relevance of our findings lies in their possible implications for routine clinical practice. Understanding the seasonal and cyclical variations of viruses and the effect of the measures adopted during the pandemic on the reduction in respiratory infections is essential if we are to be able to adequately plan preventive strategies and control outbreaks in the future. It is necessary to maintain epidemiological surveillance systems that warn us about the circulation pattern of different respiratory viruses in order to optimise health service management, including hospitalisation and intensive care unit occupancy capacity, the adequate provision of human and material resources, as well as the planning of influenza vaccination strategies or the administration of immunoprophylaxis for RSV infection in risk groups.
FundingThis study received no specific funding from public, private or non-profit organisations.
Conflict of interestThe authors declare that they have no conflicts of interest.