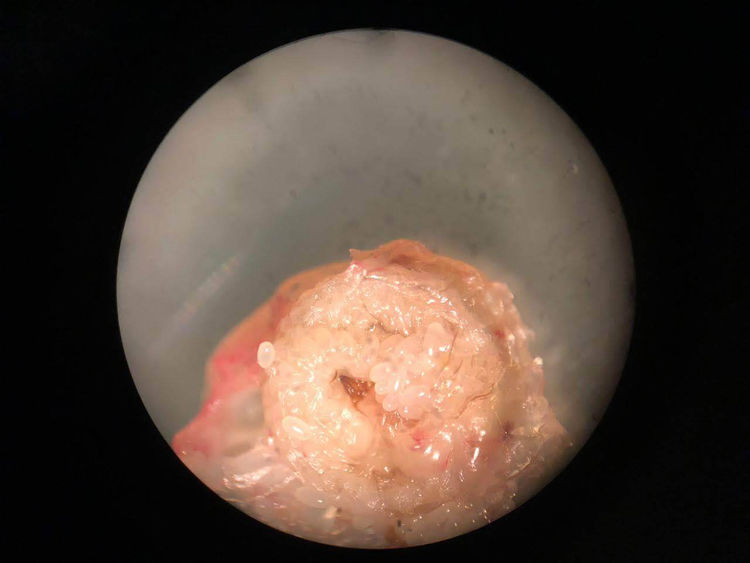
A 37-year-old male from Belgium, who has lived in Buenos Aires for 5 years. He occasionally visits San Pedro in the province of Misiones, Argentina, as a volunteer in a Guaraní village. He went to the infectious diseases clinic due to the appearance of a single, whitish papular lesion with a central black spot (Fig. 1) in the plantar region at the level of the tarsometatarsal joint of the fourth digit. The lesion appeared a week before the consultation, during his stay in San Pedro. The patient walked barefoot with the intention of reproducing the customs of the area.
Following antisepsis, the surgical extraction of the sand flea was performed and the diagnosis of infection by Tunga penetrans was confirmed after visualization of the eggs by optical microscopy (Fig. 2). Local wound treatments were given and the tetanus vaccine was administered. The lesion had a favourable evolution, without complications.
CommentsTungiasis is an ectoparasitic disease, endemic in Latin America, the Caribbean and sub-Saharan Africa, caused by penetration into the skin of the female T. penetrans (commonly known as sand flea) or, less frequently, by the flea Tunga trimamillata.1 The flea feeds on blood, enlarges to a spherical shape of 5–8mm in diameter and produces eggs that are expelled through the skin of the host. The lesions are nodular, can be single or multiple, and often appear with a black dot in the centre.2,3 Acute inflammation, characterized by erythema, oedema, pain and pruritus, is caused by the growth of a biologically active foreign body inside the epidermis, which puts pressure on the surrounding tissue.4
The treatment is removal of the flea. They should be removed as early as possible to avoid infections and other secondary complications. The extraction of the parasite must be complete, since remnants that remain in the host can generate a local inflammatory response. In addition, the tetanus vaccine should be indicated if necessary.
In humans, tungiasis predominantly affects marginalized populations. Although not included in the WHO's list of neglected tropical diseases (NTD), tungiasis has all the characteristics of an NTD to merit the concern of the public health sector.5
It should be suspected with the appearance of hyperkeratotic, whitish lesions with a blackish centre in areas supporting of people with a history of having gone barefoot in regions where this parasitosis is endemic.6 It is an emerging infection in travellers, so it is important to instruct those travelling to endemic areas about the importance of wearing closed shoes to avoid infestation by this parasite.
Please cite this article as: Cancio-Suárez MR, Bruno D, Monroig J, Lloveras S. Lesión plantar en Misiones, Argentina. Enferm Infecc Microbiol Clin. 2020;38:191–192.