We present the case of a 24-year-old man of Spanish origin who reported no relevant medical or epidemiological history except for contact with a rural environment. He consulted with a fluctuant, erythematous, hot, pre-tibial lesion on his left leg, which was painful on palpation and exuded serous fluid when pressed (Fig. 1).
Detailed history from the patient revealed that two weeks previously he had suffered a superficial wound on the affected area after falling from his bike in scrubland, for which he was treated as an outpatient with amoxicillin–clavulanic acid. No other abnormalities were found in the physical examination or blood tests (blood count and CRP normal). Biopsies were taken of the lesion for pathology and microbiology. Syphilis and HIV serology were negative.
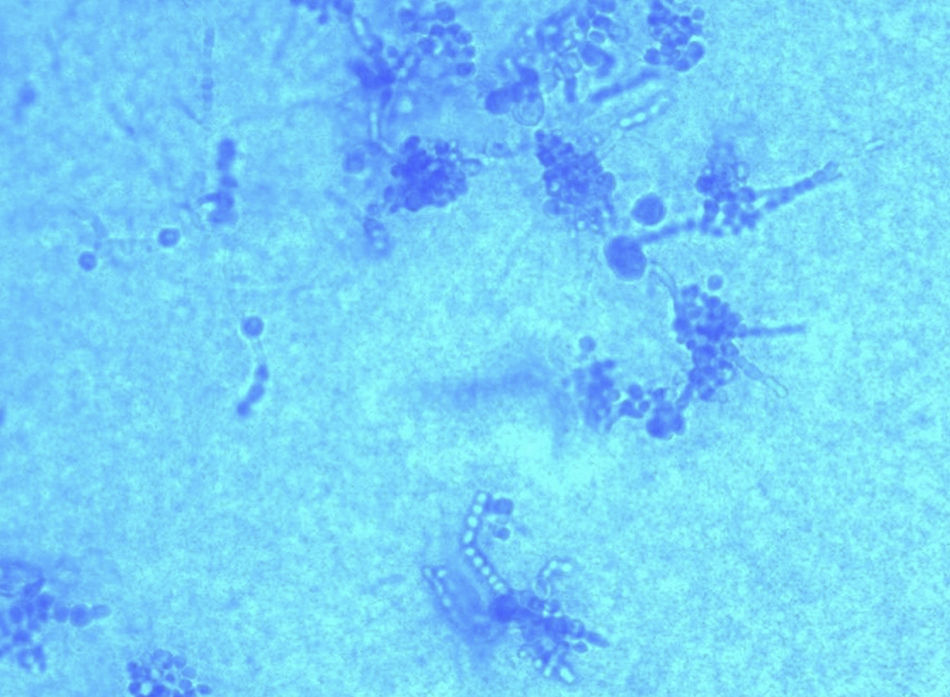
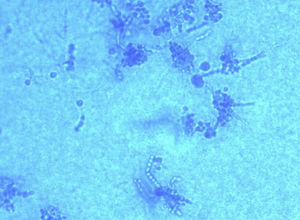
Clinical courseThe samples were processed for bacterial, fungal and mycobacterial culture. After two days of incubation, growth was observed in both samples of waxy, white colonies on blood and chocolate agar (bioMérieux), and, on Sabouraud and Mycosel medium (bioMérieux) incubated at 37°C, there was a white surface with marked creases and yellowish on the other side (Fig. 2). In staining with lactophenol blue, septate hyphae could be seen with long chains of chlamydoconidia (terminal or intercalary), arranged like “threads of beads” along the hyphae (Fig. 3). The final identification of the strain was made by sequencing, after amplification of the internal transcribed spacer-2 (ITS-2) region, obtaining 100% similarity with sequences of Trichophyton verrucosum (GenBank® LT594456.1).
Pathology analysis found significant inflammatory infiltrate composed of lymphocytes and polymorphonuclear neutrophils, which had formed abscesses in some areas, with no evidence of fungal structures or granulomas.
After microbiological isolation, a deep skin infection by T. verrucosum was diagnosed and treatment was started with terbinafine 250mg once a day for two weeks, leading to complete resolution of the lesion.
Final commentsDermatophytoses are mycoses caused by generally superficial invasion of the skin and adnexal structures. The causative agents are filamentous fungi of the genera Trichophyton, Epidermophyton and Microsporum which parasitize the keratin.
The usual clinical presentation is ringworm, when the skin involvement is limited to the epidermis, but cases have also been described where the dermis and subcutaneous tissue are involved. The fungi of the genus Trichophyton have the greatest capacity for invasion, causing a clinical condition called fungal folliculitis, trichophytic granuloma or Majocchi granuloma.1,2 The most common aetiology is due to Trichophyton rubrum,3 but other microorganisms of the same genus can be involved.2,4 Although immunocompromised patients are usually the most likely to be affected, it has also been reported in immunocompetent patients.
The treatment is based on regimens with azoles (itraconazole is the most used) or terbinafine.
We have presented the case of an immunocompetent patient who, after traumatic inoculation in a mountainous area with cattle farms (main host of T. verrucosum), developed a Majocchi granuloma caused by T. verrucosum. The course of the infection was subacute and not very aggressive. Complete resolution of the lesion was achieved after treatment with a two-week terbinafine-based regimen, as therapeutic failures with itraconazole have been reported.5
Please cite this article as: Morán Rodríguez MÁ, Alvarez Paredes L, Buzón Martin LM, Martinez Nuñez P. Lesión pretibial izquierda fluctuante postraumática. Enferm Infecc Microbiol Clin. 2019;37:205–206.