A 51-year-old man with no medical history of interest visited the accident and emergency department with oppressing central chest pain and dyspnoea on exertion. In his initial assessment, he was found to be afebrile and haemodynamically stable, though with evidence of incipient congestion and an oxygen saturation value of 95% while breathing room air. Cardiac auscultation revealed a systolic murmur at the left sternal border. An echocardiogram showed severe aortic insufficiency leading to mild left ventricular dilation with preserved left systolic ventricular function. The aortic root was thickened and not dilated. In addition to the testing done in the accident and emergency department, a computed tomography (CT) scan of the chest was performed, revealing thickening of the aortic wall and the origin of the supra-aortic trunks consistent with a diagnosis of aortitis.
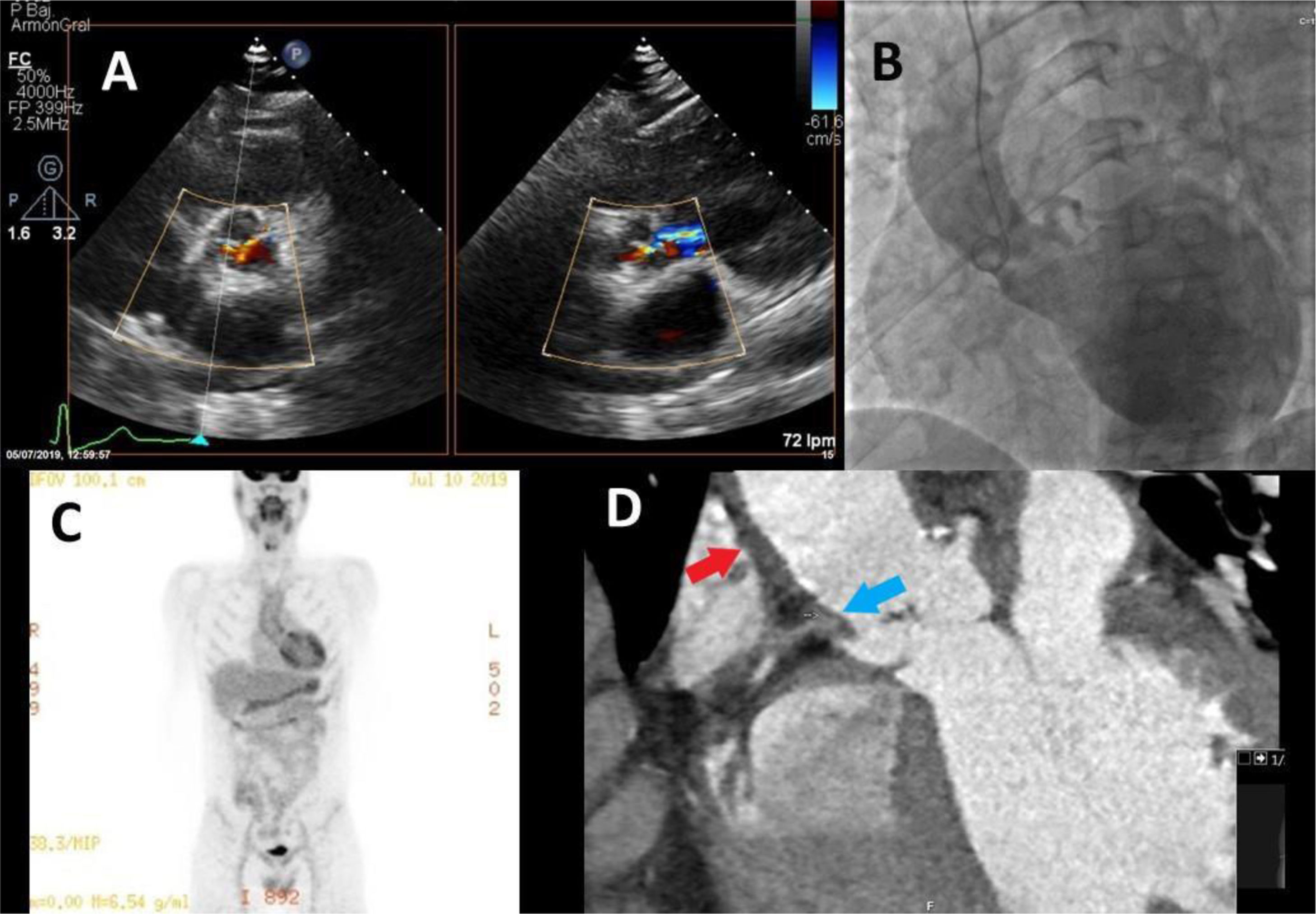
During admission, positron emission tomography/CT with 18F-fluorodeoxyglucose (18F-FDG PET/CT) was ordered and showed hyperenhancement in the wall of the ascending aorta, the aortic arch and the origin of the supra-aortic trunks. Magnetic resonance (MR) angiography of the great vessels ruled out involvement of other vascular regions. Coronary anatomy was examined by means of CT angiography, which revealed an occlusion with a chronic appearance of the ostium of the right coronary artery (RCA); this finding was subsequently confirmed with a coronary angiogram (Fig. 1).
A) Severe aortic insufficiency in a transthoracic echocardiogram. B) An aortogram showing a non-dilated aorta, occlusion at the origin of the right coronary artery (RCA) and severe regurgitation. C) 18F-FDG-PET/CT with significant hyperenhancement in the ascending aorta. D) CT angiography showing thickening of the aortic wall (red arrow) and occlusion of the RCA (blue arrow).
18F-FDG PET/CT: positron emission tomography/computed tomography with 18F-fluorodeoxyglucose; CT angiography: computed tomography angiography.
The patient showed no extracardiac signs or symptoms and had negative results for serology testing for autoimmunity (antinuclear antibodies, anti-DNA antibodies, antineutrophil cytoplasm antibodies, immunoglobulin G4 (IgG4), rheumatoid factor, serum complement, anticardiolipin antibodies and β-2 glycoprotein). His inflammatory parameters, including erythrocyte sedimentation rate (ESR), were not significantly elevated. Hence, we did not consider an underlying systemic inflammatory cause.
Microbiology testing included blood cultures and serology for atypical bacteria, fungi (Aspergillus and Cryptococcus) and viruses (human immunodeficiency virus, cytomegalovirus and hepatitis B and C viruses). All results were negative apart from those of the treponemal test (Treponema pallidum haemagglutination [TPHA] titre 1:640) and the non-treponemal test (rapid plasma reagin [RPR] titre 1:32), which were decidedly positive. As a result, the patient was diagnosed with syphilitic aortitis.
Clinical courseAlthough the patient lacked neurological involvement, he was put on an antibiotic regimen of 3 million international units (MIU) of intravenous penicillin G every four hours for 15 days. Once this treatment was finished, aortic valve replacement and RCA revascularisation surgery was planned. During the procedure, significant stiffness and hardness of the aortic wall was observed; cannulation required the use of dilators. In addition, the entire aorta showed a significant inflammatory reaction, particularly at the root, and the non-coronary leaflet was seen to be adhered to the aortic wall. Ultimately, aortic valve replacement with implantation of a bioprosthetic heart valve, resection of the non-coronary sinus plus aortoplasty with bovine pericardium and revascularisation with a vein graft to the posterior descending artery were performed.
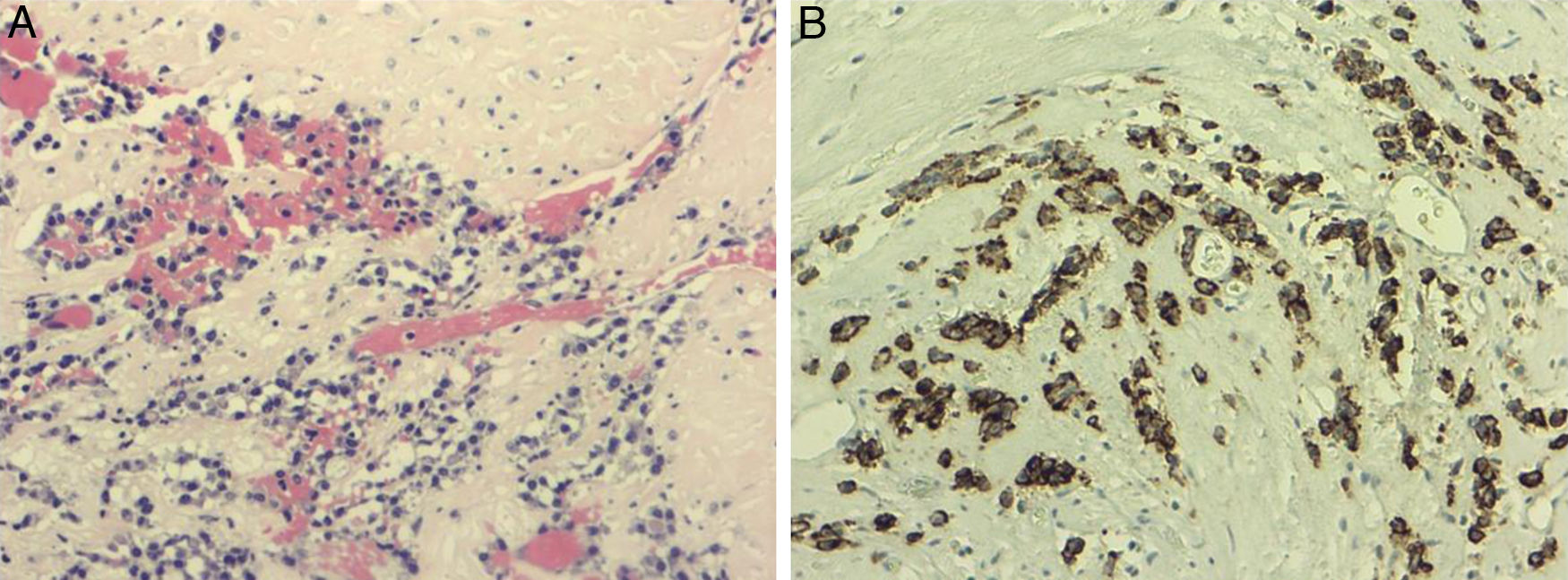
Pathology confirmed the presence of lymphoplasmacytic infiltrate in the adventitia and intima of the aortic wall consistent with the diagnosis of syphilitic aortitis; immunohistochemistry was negative for Treponema pallidum and IgG4 (Fig. 2).
The postoperative period was uneventful. After two months, a two-dilution decrease was seen in the non-treponemal test (RPR titre 1:8).
Closing remarksSyphilis is a sexually transmitted disease caused by the spirochaete T. pallidum. Left untreated, the disease may progress through primary, secondary and tertiary stages. Tertiary syphilis is a very uncommon disease at the present time. It develops around five to 10 years after the primary infection, but its symptoms may not be obvious until more than 20 years have elapsed.1 Cardiovascular involvement is characterised by obliterating endarteritis of the vasa vasorum of the great vessels, especially of the aortic root, coronary ostia and ascending thoracic aorta.2 The presence of lymphocytic inflammatory infiltrate in the pathology study is characteristic.3
The differential diagnosis of aortitis includes infectious causes (Salmonella, Staphylococcus and Streptococcus are the most commonly isolated pathogens) and non-infectious causes, such as vasculitis of the great vessels (giant cell arteritis or Takayasu's arteritis), IgG4-related aortitis or aortitis in the context of systemic inflammatory diseases.4
The mechanism typically associated with syphilitic aortic regurgitation is aortic root dilation.5 Our case was exceptional in that the aorta was not dilated. We believe that the degree of aortic root inflammation and the traction exerted by the fibrotic aortic ring represented the underlying cause of the patient's aortic insufficiency.
Treatment for cardiovascular syphilis consists of weekly injections of 2.4 MIU of benzathine penicillin G for three weeks.6 Surveillance in the hours subsequent to starting treatment is important due to a risk of developing a Jarisch–Herxheimer reaction caused by lysis of the spirochaete in the affected tissues.7
Please cite this article as: Cobas-Paz R, Rioboo-Lestón L, Piñón-Esteban M, Calvo-Iglesias FE. El enemigo olvidado y silencioso del sistema cardio-vascular: un caso de aortitis poco frecuente. Enferm Infecc Microbiol Clin. 2022;40:147–149.