The global health emergency caused by the current COVID-19 pandemic is resulting in a huge challenge at all levels. The use of masks may reduce the spread of the infection by minimising the excretion of Flügge droplets. The objective of this study was to compile the evidence available on the use of masks in relation to respiratory infections.
MethodologyAn umbrella review (review of systematic reviews) was conducted. Two reviewers independently carried out the screening process, data extraction and data analysis. Discrepancies were resolved with a third reviewer, and the assessment of the risk of bias of the studies was carried out using the AMSTAR 2 tool. The Rayyan QCRI program was used for the screening process.
ResultsA total of eight systematic reviews were included. The studies analysed the use of masks in the general population, in long-term care facilities, in hospitals and at mass gatherings, and compared the effectiveness thereof in preventing infection. The results of this review revealed that the use of masks is associated with a protective effect against respiratory infections in healthcare facilities, in long-term care facilities and at mass gatherings.
ConclusionsIn light of the results, it seems reasonable to recommend the use of masks to the general population, but this use should be accompanied by a training programme to improve compliance, as not using them properly may increase the risk of infection.
La emergencia sanitaria global causada por la actual pandemia de Covid-19 está suponiendo un enorme desafío a todos los niveles. El uso de la mascarilla puede reducir la propagación de la infección al minimizar la excreción de las gotitas de Flügge. Así, el objetivo de este trabajo es realizar una recopilación de la evidencia disponible sobre el uso de mascarillas en relación con las infecciones respiratorias.
MetodologíaSe realizó una revisión de revisiones sistemáticas (umbrella review). Dos revisores realizaron de forma independiente el proceso de cribado, la extracción y el análisis de datos, las discrepancias fueron solventadas con un tercer revisor, la evaluación del riesgo de sesgo de los trabajos se realizó mediante la herramienta AMSTAR-2. Para el proceso de cribado se utilizó el programa Rayyan QCRI.
ResultadosSe incluyeron un total de 8 revisiones sistemáticas. Los estudios analizaron el uso en población general, en centros de cuidados de larga duración, centros hospitalarios, eventos masivos y compararon la efectividad para evitar las infecciones. Los resultados de esta revisión ponen de manifiesto que el uso de las mascarillas se asocia a un efecto protector frente a las infecciones respiratorias, tanto en los centros sanitarios, como en los centros de cuidados de larga duración y en los eventos masivos.
ConclusionesA la luz de resultados parece razonable recomendar el uso de las mascarillas a la población general, pero este uso debe venir acompañada de un plan de formación, mejorar el cumplimiento ya que su uso inadecuado puede ser favorecer la infección.
In the last century, humanity has suffered a number of epidemics that have led to millions of cases of disease, hospitalisation and death, as well as an important social and economic burden1. Over this period, globalisation processes, together with advances in medicine and epidemiology, have changed the way such pandemics are experienced. The global health emergency caused by the current COVID-19 pandemic is posing a huge challenge at all levels2.
Leaders require the best evidence to be quickly available in order for it to be of use to them in making decisions with the goal of guaranteeing the safety and health of the population through efficient use of resources. In addition, it must be taken into account that the International Health Regulations 2005, which regulate the management of health emergencies, establish that any public health measure must be based on scientific criteria3.
One important set of measures is personal protective equipment, which includes gloves, goggles, screens, gowns and masks. The use of masks may reduce the spread of the infection by minimising the excretion of Flügge droplets. Masks fall into two broad groups: a) surgical and medical masks, which are designed to avoid only the outbound dissemination or microorganisms and are classified, based on bacterial filtration capacity, as type I or II, being 95% or 98% effective, respectively; b) filtering masks that protect against both outbound and inbound particles. In Europe, they are classified, based on minimal filtration efficacy for airborne particles smaller than 0.3 μm, as FFP1, FFP2 and FFP3, with values of 78%, 92% and 98%, respectively. In the United States, the classification is N95, N99 and N100, with filtration capacities of 95%, 99% and 100%4.
Different countries have recommended generalised use of masks as a potential tool to curb the COVID-19 pandemic5. The evidence regarding and acceptance of the use of masks to prevent respiratory infections during epidemics is scant and contested6. The recommendations of the different international bodies on the use of masks by the general population are heterogeneous. For example, the World Health Organization recommended the use of surgical masks in low-risk situations, while in high-risk situations it recommended N95 masks; in contrast, the US Centers for Disease Control and Prevention (CDC) and European Centre for Disease Prevention and Control (ECDC) were in favour of using N95 masks in both situations5,7. Therefore, the objective of this study was to conduct a review of systematic reviews in order to compile the evidence available on the use of masks in relation to respiratory infections.
MethodsA rapid review8 of systematic reviews was conducted, following the indications in the Joanna Briggs Institute guidance (2014)9. The databases and resources consulted were PubMed, repositories of systematic reviews (the Cochrane Library, Effective Health Care Program AHRQ, McMaster University and the Red de Agencias de Evaluación de Tecnologías Sanitarias [Spanish Network of Agencies for Health Technology Assessment]) and specific databases on COVID-19 (Orientación sobre la COVID-19 y últimas investigaciones en las Américas [COVID-19 guidance and the latest research in the Americas]10), as well as Google Scholar. The references of documents already identified were also reviewed.
The PubMed searches were performed using a combination of free and controlled terms (("Respiratory Tract Infections"[Mesh] OR "Respiratory Tract Infections") AND ("Masks"[Mesh] OR "Masks")). The systematic reviews filter designed by the Scottish Intercollegiate Guidelines Network (SIGN)11 was used to limit the results to systematic reviews. This search was adapted to the language of the other sources consulted. All of this was validated by a librarian specialised in public health.
Those systematic reviews that compiled evidence on the prevention of respiratory infections through the use of masks were included. Those published works where, despite assessing protective measures, the use of masks was not established in less than 50% were excluded; likewise, those published in a language other than English or Spanish were excluded. When two reviews were found that researched the same question, the most up-to-date reference was included, as well as the one with results covering the greatest number of works.
Data extraction and analysisTwo reviewers (AOL and EMR) independently assessed the titles and abstracts to determine whether the documents met the inclusion criteria; those documents though to meet the criteria were saved (first selection) and then their full text was independently assessed (second selection). Discrepancies in both selections were resolved by a third reviewer (CBT). A form was designed and piloted to extract and transfer the information (objective, methodology, results and conclusions), and the results extraction process was carried out by the reviewers, thereby ensuring the accuracy of the information compiled, based on this review's objective. After selecting the articles of interest, two investigators (EM and AOL) performed an independent assessment of the methodological quality of each review. This was done using the AMSTAR-2 (A MeaSurement Tool to Assess systematic Reviews)12 tool to assess the risk of bias in systematic reviews, which consists of 16 questions. Discrepancies were resolved by consensus. For the selection process, the Rayyan QCRI (https://rayyan.qcri.org/) application for systematic reviews was used.
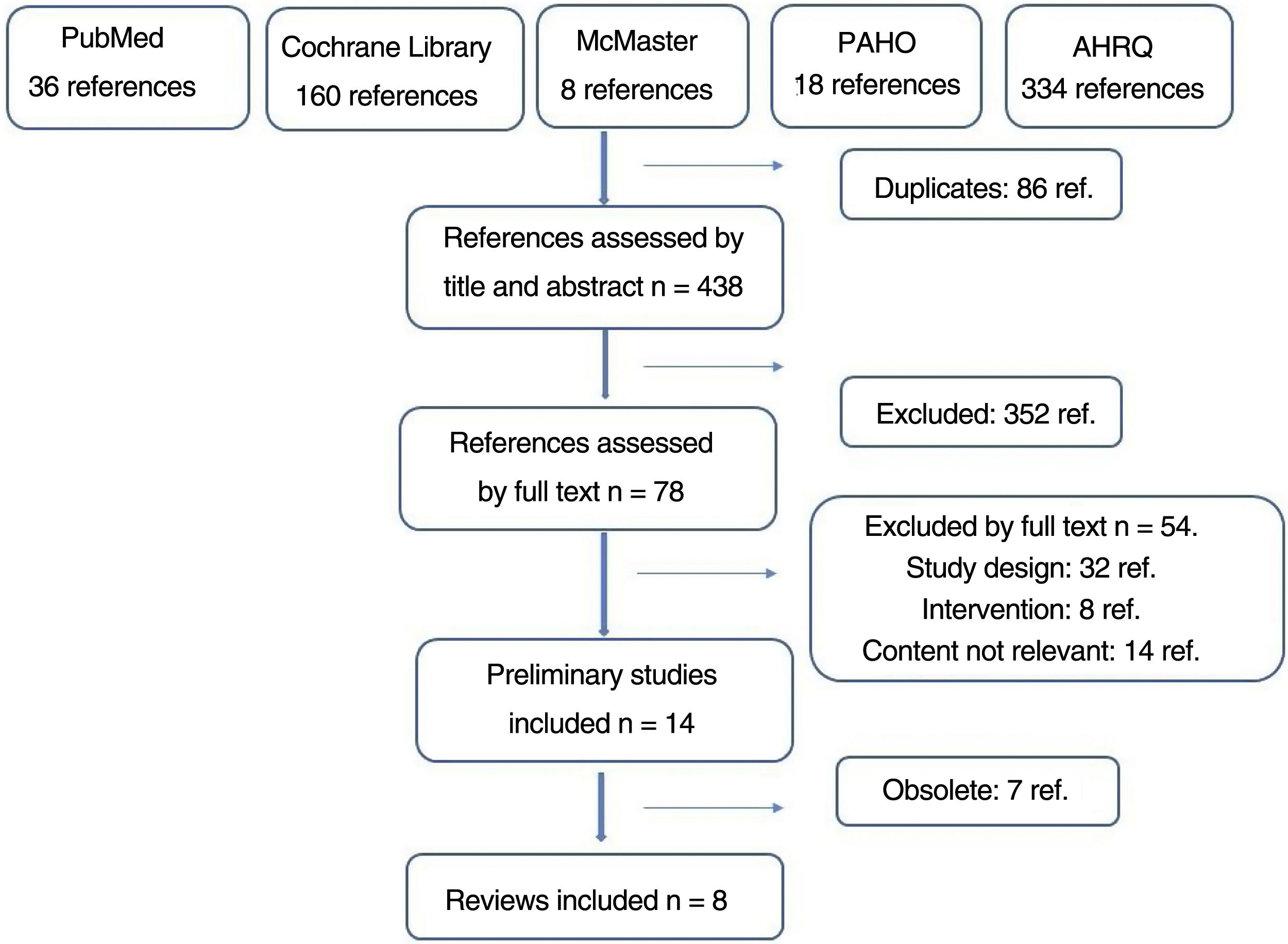
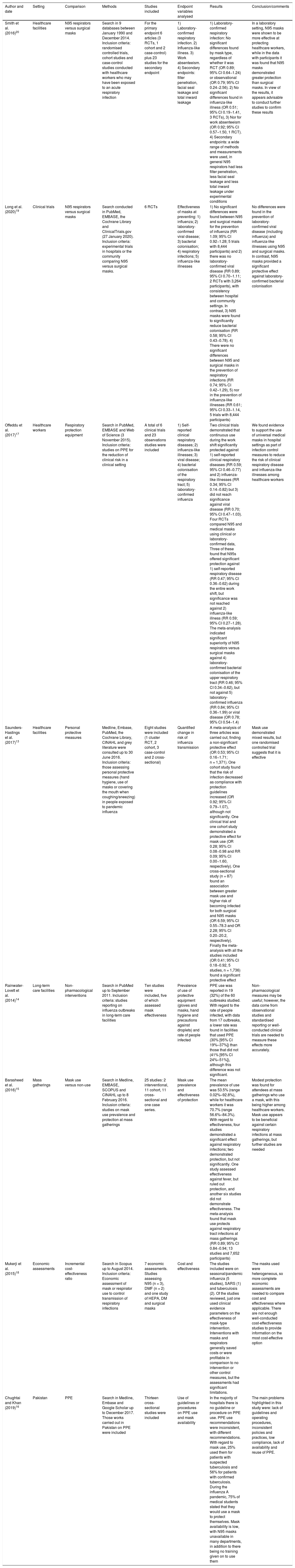
ResultsThe details of the literature search and selection process can be seen in Fig. 1. A total of 520 references were identified after consulting the various databases. After carrying out the selection process, 15 reviews were subsequently selected, of which it was decided to exclude seven as they addressed the same research question as other more up-to-date reviews (Appendix B Table A1 of the additional material). Eight systematic reviews were ultimately included. Table 1 shows their main characteristics, all of them being published after 2014.
Characteristics of the reviews included.
| Author and date | Setting | Comparison | Methods | Studies included | Endpoint variables analysed | Results | Conclusion/comments |
|---|---|---|---|---|---|---|---|
| Smith et al. (2016)20 | Healthcare facilities | N95 respirators versus surgical masks | Search in 9 databases between January 1990 and December 2014. Inclusion criteria: randomised controlled trials, cohort studies and case-control studies conducted with healthcare workers who may have been exposed to an acute respiratory infection | For the primary endpoint 6 articles (3 RCTs, 1 cohort and 2 case-control) plus 23 studies for the secondary endpoint | 1) Laboratory-confirmed respiratory infection. 2) Influenza-like illness. 3) Work absenteeism. 4) Secondary endpoints: filter penetration, facial seal leakage and total inward leakage | 1) Laboratory-confirmed respiratory infection: No significant differences found by mask type, regardless of whether it was RCT (OR 0.89; 95% CI 0.64−1.24) or observational (OR 0.79; 95% CI 0.24−2.56). 2) No significant differences found in influenza-like illness (OR 0.51; 95% CI 0.19−1.41, 3 RCTs), 3) Nor for work absenteeism (OR 0.92; 95% CI 0.57−1.50, 1 RCT). 4) Secondary endpoints: a wide range of methods and measurements were used, in general N95 respirators had less filter penetration, less facial seal leakage and less total inward leakage under experimental conditions | In a laboratory setting, N95 masks were shown to be more effective at protecting healthcare workers, while in the data with participants it was found that N95 masks demonstrated greater protection than surgical masks. In view of the results, it appears advisable to conduct further studies to confirm these results |
| Long et al. (2020)19 | Clinical trials | N95 respirators versus surgical masks | Search conducted in PubMed, EMBASE, the Cochrane Library and ClinicalTrials.gov (27 January 2020). Inclusion criteria: experimental trials in hospitals or the community comparing N95 versus surgical masks. | 6 RCTs | Effectiveness of masks at preventing: 1) influenza; 2) laboratory-confirmed viral disease; 3) bacterial colonisation; 4) respiratory infections; 5) influenza-like illnesses | 1) No significant differences were found between N95 and surgical masks for the prevention of influenza (RR 1.09; 95% CI 0.92−1.28; 5 trials with 8,444 participants) and 2) there was no laboratory-confirmed viral disease (RR 0.89; 95% CI 0.70−1.11; 2 RCTs with 3,264 participants), with consistency between hospital and community settings. In contrast, 3) N95 masks were found to significantly reduce bacterial colonisation (RR 0.58; 95% CI 0.43−0.78). 4) There were no significant differences between N95 and surgical masks in the prevention of respiratory infections (RR 0.74; 95% CI 0.42−1.29), 5) nor in the prevention of influenza-like illnesses (RR 0.61; 95% CI 0.33−1.14, 5 trials with 8,444 participants) | No differences were found in the prevention of laboratory-confirmed viral disease (including influenza) and influenza-like illnesses using N95 and surgical masks. In contrast, N95 masks provided a significant protective effect against laboratory-confirmed bacterial colonisation |
| Offeddu et al. (2017)17 | Healthcare workers | Respiratory protection equipment | Search in PubMed, EMBASE and Web of Science (3 November 2015). Inclusion criteria: studies on PPE for the reduction of clinical risk in a clinical setting | A total of 6 clinical trials and 23 observations studies were included | 1) Self-reported clinical respiratory diseases; 2) influenza-like illnesses; 3) viral disease; 4) bacterial colonisation of the respiratory tract; 5) laboratory-confirmed influenza | Two clinical trials demonstrated that continuous use during the work shift significantly protected against 1) self-reported clinical respiratory diseases (RR 0.59; 95% CI 0.46−0.77) and 2) influenza-like illnesses (RR 0.34; 95% CI 0.14−0.82) but 3) did not reach significance against viral disease (RR 0.70; 95% CI 0.47−1.03). Four RCTs compared N95 and medical masks using clinical or laboratory-confirmed data, Three of these found that N95s offered significant protection against 1) self-reported respiratory disease (RR 0.47; 95% CI 0.36−0.62) during the entire work shift, but significance was not reached against 2) influenza-like illness (RR 0.59; 95% CI 0.27−1.28). The meta-analysis indicated significant superiority of N95 respirators versus surgical masks against 4) laboratory-confirmed bacterial colonisation of the upper respiratory tract (RR 0.46; 95% CI 0.34−0.62), but not against 5) laboratory-confirmed influenza (RR 0.84; 95% CI 0.36−1.99) or viral disease (OR 0.78; 95% CI 0.54−1.4) | We found evidence to support the use of universal medical masks in hospital settings as part of infection control measures to reduce the risk of clinical respiratory disease and influenza-like illnesses among healthcare workers |
| Saunders-Hastings et al. (2017)13 | Healthcare facilities | Personal protective measures | Medline, Embase, PubMed, the Cochrane Library, CINAHL and grey literature were consulted up to 30 June 2016. Inclusion criteria: those assessing personal protective measures (hand hygiene, use of masks or covering the mouth when coughing/sneezing) in people exposed to pandemic influenza | Eight studies were included (1 cluster RCT, 2 cohort, 3 case-control and 2 cross-sectional) | Quantified change in risk of influenza transmission | A meta-analysis of three articles was carried out, finding a non-significant protective effect (OR 0.53; 95% CI 0.16−1.71; n = 1,371). One cohort study found that the risk of infection decreased as compliance with protection guidelines increased (OR 0.92; 95% CI 0.79−1.07), although not significantly. One clinical trial and one cohort study demonstrated a protective effect for mask use (OR 0.28; 95% CI 0.08−0.98 and RR 0.09; 95% CI 0.00−1.60, respectively). One cross-sectional study (n = 87) found an association between greater mask use and higher risk of becoming infected for both surgical and N95 masks (OR 6.59; 95% CI 0.55−78.3 and OR 2.28; 95% CI 0.20−20.2, respectively). Finally the meta-analysis with all the studies included (OR 0.41; 95% CI 0.18−0.92, 5 studies, n = 1,736) found a significant protective effect | Mask use demonstrated mixed results, but one randomised controlled trial suggests that it is effective |
| Rainwater-Lovett et al. (2014)14 | Long-term care facilities | Non-pharmacological interventions | Search in PubMed up to September 2011. Inclusion criteria: studies reporting on influenza outbreaks in long-term care facilities | Ten studies were included, five of which assessed mask effectiveness | Prevalence of use of protective equipment (gloves and masks, hand hygiene and precautions against droplets) and rate of people infected | PPE use was reported in 19 (32%) of the 60 outbreaks studied. With regard to the rate of people infected, with data from 17 outbreaks, a lower rate was found in facilities that used PPE (30% [95% CI 19%–37%]) than those that did not (41% [95% CI 24%–51%]), although this difference was not significant. | Non-pharmacological measures may be useful; however, the data come from observational studies and standardised reporting or well-conducted clinical trials are needed to measure these effects more accurately. |
| Barasheed et al. (2016)15 | Mass gatherings | Mask use versus non-use | Search in Medline, EMBASE, SCOPUS and CINAHL up to 8 February 2016. Inclusion criteria: studies on mask use prevalence and protection at mass gatherings | 25 studies: 2 interventional, 11 cohort, 11 cross-sectional and one case series. | Mask use prevalence and effectiveness of protection | The mean prevalence of use was 53.5% (range 0.02%–92.8%), while for healthcare workers it was 70.7% (range 56.6%–84.3%). With regard to effectiveness, four studies demonstrated a significant effect against respiratory infections; two demonstrated protection, but not significantly. One study assessed effectiveness against fever, but ruled out protection, and another six studies did not demonstrate effectiveness. The meta-analysis found that mask use protects against respiratory tract infections at mass gatherings (RR 0.89; 95% CI 0.84−0.94; 13 studies and 7,652 participants) | Modest protection was found for attendees at mass gatherings who use a mask, with this being higher among healthcare workers. Mask use appears to be beneficial against certain respiratory infections at mass gatherings, but further studies are needed |
| Mukerji et al. (2015)18 | Economic assessments | Incremental cost-effectiveness ratio | Search in Scopus up to August 2014. Inclusion criteria: Economic assessment of mask or respirator use to control transmission of respiratory infections | 7 economic assessments. Studies assessing N95 (n = 3), DMF (n = 2) and one study of HEPA, DM and surgical masks | Cost and effectiveness | The studies included were on seasonal/pandemic influenza (5 studies), SARS (1) and tuberculosis (2). Of the studies reviewed, just one used clinical evidence parameters on the effectiveness of mask-type intervention. Interventions with masks and respirators generally saved costs or were profitable in comparison to no intervention or other control measures, but the assessments had significant limitations. | The masks used were heterogeneous, so more complete economic assessments are needed to compare cost and effectiveness where applicable. There are not enough well-conducted cost-effectiveness studies to provide information on the most cost-effective option |
| Chughtai and Khan (2019)16 | Pakistan | PPE | Search in Medline, Embase and Google Scholar up to December 2017. Those works carried out in Pakistan on PPE were included | Thirteen cross-sectional studies were included | Use of guidelines or procedures on PPE use and mask availability | In the majority of hospitals there is no guideline or procedure on PPE use. PPE use recommendations were inconsistent, with different recommendations. With regard to mask use, 25% used them for patients with suspected tuberculosis and 56% for patients with confirmed tuberculosis. During the influenza A pandemic, 75% of medical students stated that they would use a mask to protect themselves. Mask availability is low, with N95 masks unavailable in many departments, in addition to there being no training given on to use them | The main problems highlighted in this study were: lack of guidelines and operating procedures, inconsistent policies and practices, low compliance, lack of availability and reuse of PPE. |
DM: dust-mist; DMF: dust-mist-fume; HEPA: high-efficiency particulate air; OR: odds ratio; PPE: personal protective equipment; RCT: randomised clinical trial; RR: relative risk; SARS: severe acute respiratory syndrome; 95% CI: 95% confidence interval.
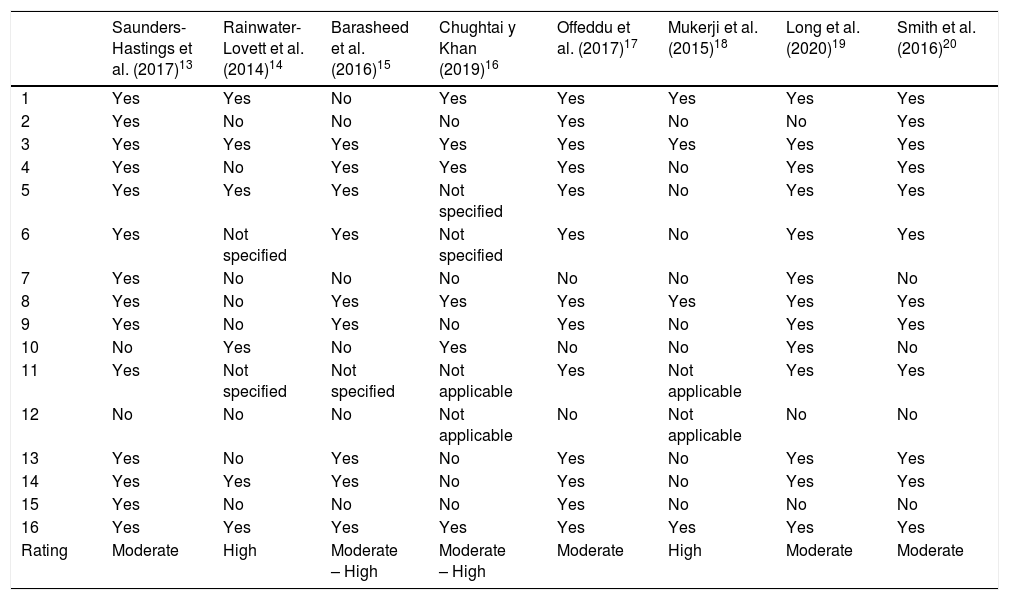
The methodological quality score of the reviews included varies between a high and moderate risk of bias. With regard to this score, it is noteworthy that none of the meta-analysis articles assessed the impact of the risk of bias. In contrast, all of the reviews adequately explained the inclusion criteria used and their potential sources of interest (Table 2).
Bias risk assessment score of the reviews included using the AMSTAR-2 tool.
| Saunders-Hastings et al. (2017)13 | Rainwater-Lovett et al. (2014)14 | Barasheed et al. (2016)15 | Chughtai y Khan (2019)16 | Offeddu et al. (2017)17 | Mukerji et al. (2015)18 | Long et al. (2020)19 | Smith et al. (2016)20 | |
|---|---|---|---|---|---|---|---|---|
| 1 | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| 2 | Yes | No | No | No | Yes | No | No | Yes |
| 3 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 4 | Yes | No | Yes | Yes | Yes | No | Yes | Yes |
| 5 | Yes | Yes | Yes | Not specified | Yes | No | Yes | Yes |
| 6 | Yes | Not specified | Yes | Not specified | Yes | No | Yes | Yes |
| 7 | Yes | No | No | No | No | No | Yes | No |
| 8 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes |
| 9 | Yes | No | Yes | No | Yes | No | Yes | Yes |
| 10 | No | Yes | No | Yes | No | No | Yes | No |
| 11 | Yes | Not specified | Not specified | Not applicable | Yes | Not applicable | Yes | Yes |
| 12 | No | No | No | Not applicable | No | Not applicable | No | No |
| 13 | Yes | No | Yes | No | Yes | No | Yes | Yes |
| 14 | Yes | Yes | Yes | No | Yes | No | Yes | Yes |
| 15 | Yes | No | No | No | Yes | No | No | No |
| 16 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Rating | Moderate | High | Moderate – High | Moderate – High | Moderate | High | Moderate | Moderate |
AMSTAR-2: A MeaSurement Tool to Assess systematic Reviews.
The review by Saunders-Hastings et al. (2017)13 included 16 studies on protective measures (15 on hand-washing and eight on mask effectiveness) versus influenza, in any population. A meta-analysis of three observational studies found that mask use protects against influenza (OR 0.53; 95% CI 0.16−1.71; n = 1,371), although the association found was not significant. This result did achieve statistical significance once experimental and observational studies were included (OR 0.41; 95% CI 0.18−0.92; n = 1,736). The remaining studies included had disparate objectives and methodologies; of note is one prospective study without a control group that found a non-significant reduction of 10% in the risk of infection after increasing adherence to mask use guidelines (OR 0.92; 95% CI 0.79−1.07). Two other studies found that mask use protected against influenza, with one of them being a quasi-experimental study (OR 0.28; 95% CI 0.08−0.98) and the other a cohort study (RR 0.09; 95% CI 0.00−1.60).
With regard to long-term care facilities, Rainwater-Lovett et al. (2014)14 assessed influenza prevention interventions, including 37 articles with data on 60 outbreaks. A total of 19 (32%) articles analysed the use of personal protective equipment (PPE) (masks, gloves, hand hygiene and protection from droplets), with masks used in 50% of the studies. No differences were found in the rate of infected individuals in facilities that used PPE (30% [95% CI 19%–37%]) and those that did not (41% [95% CI 24%–51%]). Moreover, these rates were similar to those where antivirals were used.
The use of masks at mass gatherings was studied by Barasheed et al. (2016)15, who included 13 studies (six cohort, five cross-sectional and two interventional studies). They found moderate mask use at mass gatherings, with a mean of 53.5% (range 0.02%–92.8%), whereas for healthcare workers it was 70.7% (range 56.6%–84.3%). The meta-analysis demonstrated that mask use offered a protective effect against respiratory infections (RR 0.89; 95% CI 0.84−0.94; n = 7,652).
The systematic review by Chughtai and Khan (2019)16 brought together evidence on PPE use in the healthcare field in Pakistan. Thirteen articles were included, covering hospital (n = 7), dental (n = 4) and laboratory (n = 2) settings. This review reveals that the main problems surrounding PPE in Pakistan were: lack of guidelines and operating procedures, inconsistent policies and practices, low compliance in use, lack of availability and reuse.
The review by Offeddu et al. (2017)17 included a total of six clinical trials and 23 observational studies. Two clinical trials demonstrated that continuous use of masks (N95 or surgical) during the work shift significantly protected against self-reported clinical respiratory diseases (RR 0.59; 95% CI 0.46−0.77) and influenza-like illnesses (RR 0.34; 95% CI 0.14−0.82) but was not significant against viral disease (RR 0.70; 95% CI 0.47−1.03). Three studies compared mask use against non-use, finding reductions in reported respiratory infections (RR 0.59; 95% CI 0.46−0.77), influenza-like infection (RR 0.34; 95% CI 0.14−0.82) and, albeit not significantly, laboratory-confirmed viral disease (RR 0.70; 95% CI 0.47−1.03). The meta-analysis of observational studies (six case-control and three cohort) found that mask use among exposed healthcare workers protects against severe acute respiratory syndrome (SARS) (OR 0.22; 95% CI 0.12−0.40) versus non-use, with no significant differences found between surgical and N95 masks (OR 0.86; 95% CI 0.22–3.33). With regard to influenza A (H1N1), eight observational studies with very disparate methodologies and results were included.
To identify and evaluate economic assessments on mask use to avoid respiratory infections, Mukerji et al. (2015)18 included seven studies. This review focuses mainly on the methodology used, and not so much on the results of the assessments. It concludes that a wide variety of assessments and methodologies are used, and that these also present methodological shortcomings that hinder decision-making. Three of the seven articles offered results as cost per unit of effectiveness. The first of these reported on the incremental cost per avoided death due to influenza and SARS, while the other two reported on the cost to prevent one case of tuberculosis.
Finally, two systematic reviews were located that compared the effectiveness of N95 respirators versus surgical masks19,20. The review by Long et al. (2020)19 only included experimental studies, regardless of setting, while that by Smith et al. (2016)20 also included observational studies in healthcare facilities. With regard to the studies included, Smith et al. included six articles for the primary endpoint (three randomised clinical trials [RCT], one cohort study and two case-control studies) plus 23 laboratory studies, while Long et al. included six experimental studies, three of which were also included in the earlier review. The meta-analysis by Long et al.19 found no significant differences between N95 and surgical masks for the prevention of influenza (RR 1.09; 95% CI 0.92−1.28; five trials with 8,444 participants) nor laboratory-confirmed viral disease (RR 0.89; 95% CI 0.70−1.11; four RCTs with 3,264 participants), with these results being consistent between hospital and community settings. In contrast, it was found that N95 masks reduced bacterial colonisation (RR 0.58; 95% CI 0.43−0.78; two trials with 2,538 participants). There were no differences in the prevention of laboratory-confirmed respiratory infections between N95 and surgical masks (RR 0.74; 95% CI 0.42−1.29; two trials with 6,621 participants). Finally, no differences were found in the prevention of influenza-like illnesses using N95 and surgical masks in the hospital setting (RR 0.61; 95% CI 0.33−1.14; five trials with 8,444 participants). Similarly, considering only the observational studies on the review by Smith et al.20, no differences were found in laboratory-confirmed respiratory infection. The 23 studies conducted under laboratory conditions showed that N95 masks presented less filter penetration, less facial seal leakage and less total inward leakage.
DiscussionThe authors of this article did not find any study that looked at the impact of masks and the SARS-CoV-2 coronavirus. It being a new disease with many gaps in our knowledge, it is important to evaluate the context of studies and also to differentiate between “absence of evidence” and “evidence of absence”5,21. We therefore need to judge whether the habitual use of masks provides sufficient information to discriminate between clinically relevant and useful in day-to-day practice.
The methodology used to synthesise the evidence was an umbrella review, which is characterised by having systematic reviews as an inclusion criterion, thus enabling a large quantity of information to be brought together in a single document. It should be taken into account that we find ourselves in a moment of exceptional need for information with a high level of evidence, which has led to a large quantity of information on COVID-19 being produced. Thus, at the time of writing this report, we consulted the Medrxiv database (https://www.medrxiv.org/), finding various systematic reviews that could meet the inclusion criteria. This aspect is a limitation of this work, but it should be taken into account that, having not undergone the peer review process, the data and conclusions of these works may yet change. Ultimately, we decided not to include them. In this sense, the forthcoming review by Marasinghe (2020)22 had the objective of researching the availability of scientific evidence on the use of masks to limit the spread of COVID-19 between individuals without a medical diagnosis of COVID-19, but found no evidence in this regard.
This review has certain potential limitations that should be taken into consideration. There may be a risk of incomplete evidence; however, to minimise this, different databases were consulted. In addition, a systematic search was used to increase the likelihood of finding all reviews that could possibly be included. Likewise, the review methodology used can only offer results on what other researchers have investigated, published and systematically reviewed23.
Based on the information from the different reviews included, the use of masks was associated with a protective effect against respiratory infections in healthcare facilities, in long-term care facilities and at mass gatherings, although many of these associations were not statistically significant. It is worth noting that an important element that differentiates the pandemic and that has fostered rapid spread is the clear evidence of SARS-CoV-2 transmission by asymptomatic individuals21,24. For these reasons, it appears advisable to encourage mask use as a preventive measure that may limit that spread of certain viral respiratory diseases, including COVID-19, with a consequent impact on morbidity and mortality25. Lastly, to all of this we must add another element in support of the mask use recommendation, which is the prudence principle25. We must also take into account the devastating morbidity and mortality figures of this pandemic, in addition to its indirect effects such as the impact on mental health26,27, the economy28, etc.
In this sense, during the process of reviewing the consulted literature, it was possible to identify certain elements associated with the effectiveness of masks, such as constant mask use, maximum time of use and degree of compliance with the associated usage guidelines. Inadequate use of masks may lead to an increase in the risk of infection; they must be used constantly, as it is known that contagion often occurs when protections are removed29. In addition, mask use needs to be accompanied by other measures that have been shown to be efficient in stopping the spread of viral disease, such as hand-washing, use of gloves, or even quarantine29,30. For these reasons, it seems reasonable that, for these measures to be followed adequately, a strong campaign is needed to educate, raise awareness and provide some level of training30. Finally, it is important to indicate that continued mask use is determined by social and cultural factors31.
Among the different reviews included, the one that perhaps most closely aligns with the recommendation for mask use by the general population is the review that assesses the effectiveness of masks at mass gatherings15. Nevertheless, it should be taken into account that 21 of the 25 studies included were conducted in relation to a very specific phenomenon, the Hajj or annual pilgrimage to Mecca in Saudi Arabia, framing them in a very specific reality and circumstances, which complicates the external validity of the results.
During this pandemic, different situations have been experienced that have required particular reflection on the part of decision-makers. One of these situations is the shortage of PPE, both for healthcare workers and the general population. Thus, situations have been seen in which people were using home-made masks to protect themselves, but these home-made masks offer little protection against respiratory diseases and are not recommended to reduce aerosol transmission of infections32. Moreover, the filtration efficacy of home-made masks depends on many factors; on the one hand, the structure and composition of the fabric, and on the other, the size, velocity, shape and physical properties of the particles emitted33.
Finally, the high risk of bias in the reviews included and the scarcity of studies determining the effectiveness of mask use in the community setting mean that further studies are necessary.
Mask use is associated with a significant reduction in influenza infection in healthcare facilities13 and at mass gatherings15, as well as respiratory tract infections, versus non-use, while in long-term care facilities it is associated with a non-significant reduction in the rate of influenza infection14. Lastly, on comparing the effectiveness of surgical masks versus N95 respirators, no significant differences were found for either influenza or viral disease19,20. It should be noted that, although some of the results did not reach statistical significance, mask use does show a protective effect against infection measured in different ways.
RecommendationsTaking into account the results of the review by Barasheed et al. (2016) and the prudence principle, it appears reasonable to encourage mask use in the general population as a measure to avoid spread.
Considering the heavy impact on healthcare and residential facilities, mask use should be encouraged.
Further studies are needed to gain more in-depth knowledge on the effectiveness of masks, especially in minors.
FundingWithout funding.
AuthorsAOL and EMR made substantial contributions to the conception, design, analysis and interpretation of the data with the help of CBT and JMO. EMR and AOL designed the search and data collection strategies. All the authors participated in the preparation and critical review of the manuscript with significant contributions, approved the final content and agreed to be responsible for all aspects of the work.
Transparency declarationThe corresponding author, on behalf of the other signatories, guarantees the accuracy, transparency and honesty of the data and information contained in the study, as well as that no relevant information has been omitted, and that all discrepancies between the authors have been adequately resolved and described.
Conflicts of interestThe authors of this document declare that they have no relevant conflicts of interest that might have an effect on the study design, analysis or the presentation of the results.
To Camila Higueras Callejón, librarian at the Escuela Andaluza de Salud Pública [Andalusian School of Public Health].
Please cite this article as: Olry de Labry-Lima A, Bermúdez-Tamayo C, Martinez-Olmos J, Martin-Ruiz E. El uso de las mascarillas en la protección de las infecciones respiratorias: una revisión de revisiones. Enferm Infecc Microbiol Clin. 2021;39:436–444.